This article has been
cited by other articles in ScienceCentral.
Dear Editor:
We read with great interest the paper by Lee et al.
1 about the effects of one-dose varicella (chickenpox) vaccination on disease severity among pediatric varicella patients in Korea, given the recent concern about the effectiveness of the varicella vaccine in Korea.
23 Lee et al.
1 reported that vaccinated patients (breakthrough cases) had significantly less moderate-to-severe symptoms than non-vaccinated patients, which is consistent with the existing literature from other countries.
45 However, we think the paper by Lee et al.
1 can inadvertently mislead the reader into believing that varicella incidence in Korea has significantly increased even after the introduction of a national varicella immunization program in 2005 and the effectiveness of the varicella vaccine has been insufficient to prevent against varicella in Korea.
The authors said that “In Korea - where one-dose of varicella vaccination for all children aged 12–15 months was recommended by the National Immunization Program (NIP) in 2005 … the incidence rate of varicella has been continuously rising from 22.4 per 100,000 persons to 154.8 from 2006 to 2017.”
1 Based on the varicella incidence statistics, the authors further said that “a universal one-dose varicella vaccination program may have limited effectiveness to decrease in the incidence rate of varicella …” However, we think that the authors should have cautiously used and interpreted the varicella incidence statistics because the statistics were based on the data from the National Notifiable Disease Surveillance System (NNDSS) in which only varicella cases notified by medical doctors and other responsible persons were included and counted. In fact, in contrast to the argument of the authors, utilizing more nationally representative data (i.e., the claims data from the National Health Insurance Review and Assessment Service [NHIRAS]), both Choi et al.
6 and Jung et al.
7 have demonstrated that the incidence rate of varicella has substantially decreased in Korea (e.g., from 5.71/1,000 person-years in 2004 to 1.87/1,000 person-years in 2015) after the introduction of the varicella NIP in 2005. Like Jung et al.,
7 we think that the seemingly increasing incidence rate of varicella with the NNDSS data is a result of an improvement in doctors' reporting rate of national notifiable infectious diseases,
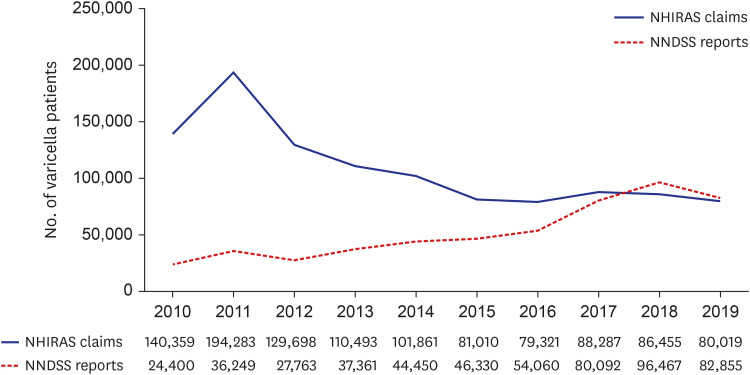
8 including varicella rather than an actual increase in varicella incidence during 2006–2017 in Korea. We have examined the trend of the annual number of total varicella patients in Korea during 2010–2019 using the two data from the NNDSS and NHIRAS.
910
Fig. 1 shows a clear opposite (increasing vs. decreasing) pattern in the trends of varicella patients by the two different data sources. It also indicates that varicella patients have been significantly underreported in the NNDSS data until recent years (2017–2019). The authors should have paid due attention to the limitation of the NNDSS data and the decreasing varicella incidence with the NHIRAS data after the introduction of the varicella NIP in Korea.
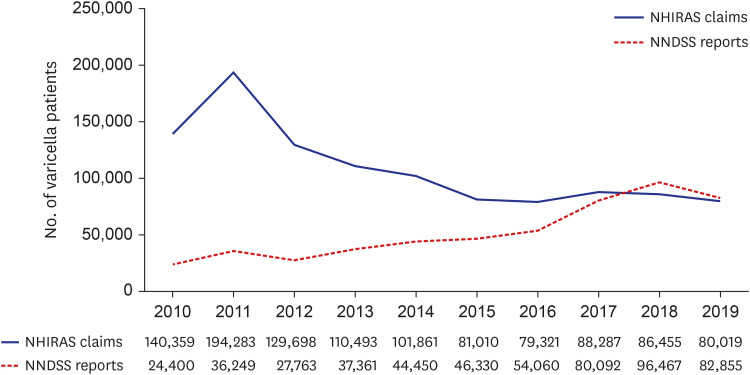 | Fig. 1
The trends of the annual number of total varicella (chickenpox) patients in Korea from 2010 to 2019 according to the two different data sources from the NHIRAS and the NNDSS.
NHIRAS = National Health Insurance Review and Assessment Service, NNDSS = National Notifiable Disease Surveillance System.

|
The authors also mentioned that their finding may be contrasted with some earlier studies on the effectiveness of the varicella vaccine in Korea, including their own previous study.
3 In their previous matched case-control study using the 2013 NNDSS data, the effectiveness of the varicella vaccine was reported to be 13%, which has been used as the main piece of evidence for their argument of insufficient effectiveness of the varicella vaccine in Korea.
3 However, we think that their previous case-control study may have a selection bias, that is, the authors may not have used an appropriate control group for the comparison in their case-control study.
11 In their previous study, the control group was selected among the patients with mumps or scarlet fever in the 2013 NNDSS data, while the case group was selected among the patients with varicella in the same data. But it is questionable whether the exposure (vaccination) information in the control group of their previous study was representative of that in the population at risk where cases arose. For example, Choi et al.
6 pointed out the problem as follows: “the vaccination rates in cases and controls were 76% and 78%, respectively, which was much lower than the results (> 95%) of the nationwide vaccination surveys.” Using the raw data from the authors' case-control study,
3 we have examined how the effectiveness of the varicella vaccine would have changed if the authors had used an alternative population-based (not patient-based) control group with a vaccination rate similar to the nationwide averages (i.e., ≥ 90%; 88.3%–91.7% in 2007 and 98.9% in 2012) around their study period.
212
Table 1 shows that while the crude effectiveness of the varicella vaccine is 12% when the vaccination rate in the control group is 78% as in the authors' previous study, it ranges from 65% to 90% when the vaccination rate in the alternative population-based control group increases from 90% to 97%. This means that the effectiveness of the varicella vaccine in the previous study by the authors
3 may have been considerably underestimated. If it would be the case, we think that their argument of insufficient effectiveness of the varicella vaccine in Korea needs to be cautiously reexamined.
Table 1
The effectiveness of the varicella vaccine by an alternative population-based control group with a national average vaccination rate (≥ 90%) using the raw data from a case-control study3

|
Vaccine coverage |
Case (n = 537) |
Control (n = 537) |
Crude OR |
Crude vaccine effectiveness: (1-OR) × 100% |
|
Data from Lee et al.3
|
|
|
|
|
|
|
Vaccine coverage rate in the control group selected among the patients with mumps or scarlet fever in the 2013 NNDSS data: 78% |
Vaccinated |
407 |
419 |
0.88 |
12% |
|
Unvaccinated |
130 |
118 |
|
If an alternative population-based control group with a national average vaccination rate (≥ 90%2,12) had been used: |
|
|
|
|
|
|
Vaccine coverage rate: 90% |
Vaccinated |
407 |
483 |
0.35 |
65% |
|
Unvaccinated |
130 |
54 |
|
Vaccine coverage rate: 95% |
Vaccinated |
407 |
510 |
0.16 |
84% |
|
Unvaccinated |
130 |
27 |
|
Vaccine coverage rate: 97% |
Vaccinated |
407 |
521 |
0.10 |
90% |
|
Unvaccinated |
130 |
16 |

We do respect the efforts of the authors to examine the effectiveness of the varicella vaccine in Korea. We think that future longitudinal studies with recent high-quality and nationally representative data having detailed and accurate information on varicella vaccination and incident varicella will help us better understand the effectiveness of the varicella vaccine in Korea. Since the reporting rate of NIP vaccination records by medical institutions and the national support program for immunization service expenses significantly improved in the mid-2010s in Korea,
13 we think that best baseline years for future longitudinal studies to examine the effectiveness of the varicella vaccine in Korea would be the mid-2010s (e.g., 2014–2016).
We welcome the interest in our paper expressed by Dr. Choi et al. in their letter. However, we would like to point out that there are some important flaws in their understanding of matched case-control study design and in their interpretation of the recent studies regarding varicella incidence and vaccination.
First, the Table shown in the letter includes serious flaws. Given the nature of a matched case-control study, it is inappropriate to apply alternative vaccination coverage to control group because, in order to assess the exact vaccine effectiveness, age was controlled for the incidence of varicella significantly differing with age. We acknowledge the controls in our study were appropriately selected as described in the study; The daily activities of most children in the same community are very similar, such as attending nursery school or kindergarten, or going to school, which letting the control group of our study, who were age-matched, and the case group be equally exposed to varicella virus. However, there is a misunderstanding by Dr. Choi et al. on the vaccinees' age distribution and their vaccination rates. Study population on our community-based matched case-control study were children younger than 12 years old in 2013 and some cases were excluded who were born prior to June 2004 when the universal varicella vaccination policy was adopted. In such context, the age distribution of both cases and age-matched controls ranges from 1 to 9 years old and it heavily concentrated near an average of 5.7 years old, so the vaccination rate of 78% in the control group may be different from the results (> 95%) of the nationwide vaccination surveys that Dr. Choi et al. has quoted. For reference, the first survey conducted in 2000 to measure vaccination rate among children under 5 years of age showed an overall coverage rate of 72.5%.
1 Furthermore, there is no accurate data on nationwide varicella vaccine coverage rate until the Korea Centers for Disease Control and Prevention released it since 2015, which targeted 3-year-old children who were born three years ago; in 2015, varicella vaccine coverage was 97.8% for 2012 birth cohort.
Second, we have to underline that, in our case-control study, not all types of varicella vaccines were ineffective; the two vaccines based on Oka strain, which has the wide-range of field effectiveness data worldwide, have resulted in effectiveness of 71.4% and 88.9%, respectively, while MAV strain-based vaccine and the other Oka strain vaccine resulted in effectiveness of −5% and −100%, respectively. This finding is in concordance with other studies. A case-control study conducted from 2007 to 2008 showed effectiveness of 8 types of varicella vaccine including MAV strain-based vaccine estimated to be 54% suggesting insufficient immunogenicity.
2 According to a recent project titled ‘Effectiveness of varicella immunization in Korea’, which conducted a retrospective cohort study, vaccine effectiveness for one-dose vaccination for all varicella was −10.8% (40.8% when propensity score matched) and there is a difference in vaccine product-specific effectiveness estimates against varicella.
3
Third, the logic is invalid that the decrease in the incidence of varicella implies the effectiveness of the varicella vaccine. We have to take into the account that it is identified in common for both data that the age peak in the incidence rate has shifted from 4 or 5 to 6 years old, although the incidence rate of varicella with the National Health Insurance Service (NHIS) data decreased contrary to an increasing trend with the National Notifiable Disease Surveillance System (NNDSS) data. The lack of age-shifting phenomenon strongly suggests that the varicella vaccination program has not been effective in preventing varicella in Korea.
2 We have stated the limitation of the NNDSS data in our recent study,
4 where an increase in notification rate due to reporting bias partly may contribute to the rapid increase of varicella notification. The observed notifications in early surveillance periods might be under-reported because national surveillance of varicella, which started in 2005, which may have not been fully activated during the initial stages. Also, changes in the reporting system, such as a transition from a paper-based to the web-based system in 2007, development of internet-based reporting system in 2009, and expansion of the reporting parties from medical institutions to diagnostic laboratory agencies in 2016, likely have enhanced the reporting rates. Nonetheless, the NHIS data itself have its own bias. The NHIS once stated that its data had the following limitation in regard to monitoring infectious disease: “To claim medical expenses by submitting rule-out diagnoses, insurance data are likely to be over-reported. Besides, since insurance data are recorded based on only an initial diagnosis without further examination, the data might not represent the exact incidence of disease”.
5
Lastly, the interpretation of the studies on varicella incidence and vaccination efficacy is inappropriate. As we discussed in our studies on varicella incidence in Korea,
467 we believe most of the varicella incidence is associated with breakthrough cases considering Korea's high rate of vaccine coverage. The surveillance data suggest secondary vaccine failure, which refers to the waning of vaccine-induced immunity over time. In our case-control study, varicella vaccine effectiveness sharply declined from 75.8% in the first year of vaccination to −7.2% in the fourth year. The recent project which conducted a cohort study showed a similar result, where vaccine effectiveness also declined from 75.0% in the first follow-up year to −4.4% in the sixth year (84.2% in first follow-up year to 44.5% in the sixth year when propensity score matched).
3 Furthermore, if the vaccine has a positive effect in the attenuation of disease severity despite that the vaccination failed to protect against varicella incidence, this could lead to a growing number of breakthrough cases as being unsuccessful in isolating patients with mild symptoms. A recent article referring both our varicella vaccination on disease severity study
8 and a study assessing the Korean national immunization program on varicella incidence using the NHIS data
9 claimed that, although varicella-associated medical utilization has been declined based on the NHIS data, questions still remain regarding the effectiveness of varicella vaccines in Korea because a previous study that assessed the effectiveness of the vaccine suggested reduced vaccine effectiveness.
2
As a concluding remark, regarding the issues Dr. Choi et al. raised about the limitation of the surveillance data, we elaborated on the issues as well as their potential impact in the discussion of our paper.
4 Given the nature of the case-control study and the information being sought, the current study was deemed sufficient to inform the scientific community transparently. As we stated in the paper, the limitation does not change the conclusion of the study.





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download