1. Correa P, Piazuelo MB. Natural history of
Helicobacter pylori infection. Dig Liver Dis. 2008; 40(7):490–496. PMID:
18396115.
2. Yamaoka Y. Mechanisms of disease:
Helicobacter pylori virulence factors. Nat Rev Gastroenterol Hepatol. 2010; 7(11):629–641. PMID:
20938460.
3. Shiota S, Suzuki R, Yamaoka Y. The significance of virulence factors in
Helicobacter pylori
. J Dig Dis. 2013; 14(7):341–349. PMID:
23452293.
4. Kim JY, Kim N, Nam RH, Suh JH, Chang H, Lee JW, et al. Association of polymorphisms in virulence factor of
Helicobacter pylori and gastroduodenal diseases in South Korea. J Gastroenterol Hepatol. 2014; 29(5):984–991. PMID:
24372834.
5. Hatakeyama M. Oncogenic mechanisms of the
Helicobacter pylori CagA protein. Nat Rev Cancer. 2004; 4(9):688–694. PMID:
15343275.
6. Eusebi LH, Zagari RM, Bazzoli F. Epidemiology of Helicobacter pylori infection. Helicobacter. 2014; 19(Suppl 1):1–5.
7. Dorer MS, Talarico S, Salama NR.
Helicobacter pylori's unconventional role in health and disease. PLoS Pathog. 2009; 5(10):e1000544. PMID:
19855816.
8. Parkin DM. The global health burden of infection-associated cancers in the year 2002. Int J Cancer. 2006; 118(12):3030–3044. PMID:
16404738.

9. Wex T, Venerito M, Kreutzer J, Götze T, Kandulski A, Malfertheiner P. Serological prevalence of
Helicobacter
pylori infection in Saxony-Anhalt, Germany, in 2010. Clin Vaccine Immunol. 2011; 18(12):2109–2112. PMID:
22012975.
10. den Hoed CM, Vila AJ, Holster IL, Perez-Perez GI, Blaser MJ, de Jongste JC, et al.
Helicobacter pylori and the birth cohort effect: evidence for stabilized colonization rates in childhood. Helicobacter. 2011; 16(5):405–409. PMID:
21923687.
11. Lim SH, Kwon JW, Kim N, Kim GH, Kang JM, Park MJ, et al. Prevalence and risk factors of
Helicobacter pylori infection in Korea: nationwide multicenter study over 13 years. BMC Gastroenterol. 2013; 13(1):104. PMID:
23800201.

12. Lee SY, Moon HW, Hur M, Yun YM. Validation of western
Helicobacter pylori IgG antibody assays in Korean adults. J Med Microbiol. 2015; 64(Pt 5):513–518. PMID:
25752852.
13. Lim SH, Kim N, Kwon JW, Kim SE, Baik GH, Lee JY, et al. Trends in the seroprevalence of
Helicobacter pylori infection and its putative eradication rate over 18 years in Korea: a cross-sectional nationwide multicenter study. PLoS One. 2018; 13(10):e0204762. PMID:
30332428.
14. Youn HS, Baik S, Lee WK, Cho MJ, Ryou HH, Choi HJ, et al. Serodiagnosis of Helicobacter pylori infection. J Korean Soc Microbiol. 1990; 25(6):463–474.
15. Jeong HL, Jung YS, Jun JS, Yeom JS, Park JS, Seo JH, et al. Comparison of four commercial ELISA kits and in-house immunoblotting for diagnosis of Helicobacter pylori infection. Pediatr Gastroenterol Hepatol Nutr. 2012; 15(2):85–90.
16. Rhee KH, Youn HS, Baik SC, Lee WK, Cho MJ, Choi HJ, et al. Prevalence of Helicobacter pylori infection in Korea. J Korean Soc Microbiol. 1990; 25(6):475–490.
17. Gologan A, Graham DY, Sepulveda AR. Molecular markers in
Helicobacter pylori-associated gastric carcinogenesis. Clin Lab Med. 2005; 25(1):197–222. PMID:
15749238.
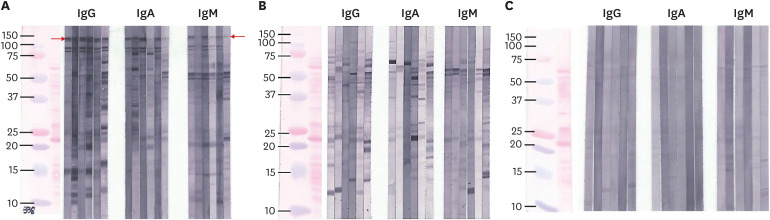
18. Seo JH, Youn JH, Kim EA, Jun JS, Park JS, Yeom JS, et al.
Helicobacter pylori antigens inducing early immune response in infants. J Korean Med Sci. 2017; 32(7):1139–1146. PMID:
28581271.
19. Malaty HM, Kim JG, Kim SD, Graham DY. Prevalence of
Helicobacter pylori infection in Korean children: inverse relation to socioeconomic status despite a uniformly high prevalence in adults. Am J Epidemiol. 1996; 143(3):257–262. PMID:
8561159.
20. Patel SK, Pratap CB, Jain AK, Gulati AK, Nath G. Diagnosis of
Helicobacter pylori: what should be the gold standard? World J Gastroenterol. 2014; 20(36):12847–12859. PMID:
25278682.
21. Sörberg M, Engstrand L, Ström M, Jönsson KA, Jörbeck H, Granström M. The diagnostic value of enzyme immunoassay and immunoblot in monitoring eradication of
Helicobacter pylori
. Scand J Infect Dis. 1997; 29(2):147–151. PMID:
9181650.
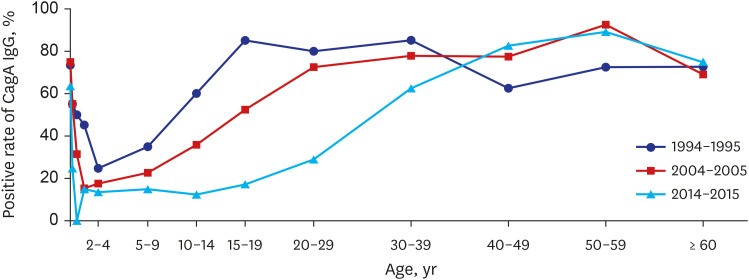
22. Seo JH, Lim CW, Park JS, Yeom JS, Lim JY, Jun JS, et al. Correlations between the CagA antigen and serum levels of anti-
Helicobacter pylori IgG and IgA in children. J Korean Med Sci. 2016; 31(3):417–422. PMID:
26955243.
23. Banatvala N, Mayo K, Megraud F, Jennings R, Deeks JJ, Feldman RA. The cohort effect and
Helicobacter pylori. J Infect Dis. 1993; 168(1):219–221. PMID:
8515114.
24. Youn HS, Baik SC, Cho YK, Woo HO, Ahn YO, Kim K, et al. Comparison of
Helicobacter pylori infection between Fukuoka, Japan and Chinju, Korea. Helicobacter. 1998; 3(1):9–14. PMID:
9546112.
25. Rhee KH, Cho MJ, Kim JB, Choi SK, Park CK, Kim YC, et al. A prospective study on the Campylopbacter pylori isolated from patients of gastroduodenal inflammatory conditions. J Korean Soc Microbiol. 1988; 23(1):9–16.
26. Song JY, Choi SH, Byun EY, Lee SG, Park YH, Park SG, et al. Characterization of a small cryptic plasmid, pHP51, from a Korean isolate of strain 51 of
Helicobacter pylori
. Plasmid. 2003; 50(2):145–151. PMID:
12932740.
27. Seo JH, Jun JS, Youn HS, Yeom JS, Park JS, Park CH, et al. Development of an ELISA for quantitative detection of immunoglobulin G (IgG) and IgA antibodies to
Helicobacter pylori for use in Korean patients with
H. pylori-associated diseases. Gut Liver. 2013; 7(4):437–442. PMID:
23898384.
28. Laemmli UK. Cleavage of structural proteins during the assembly of the head of bacteriophage T4. Nature. 1970; 227(5259):680–685. PMID:
5432063.

29. den Hollander WJ, Holster IL, den Hoed CM, van Deurzen F, van Vuuren AJ, Jaddoe VW, et al. Ethnicity is a strong predictor for
Helicobacter pylori infection in young women in a multi-ethnic European city. J Gastroenterol Hepatol. 2013; 28(11):1705–1711. PMID:
23808840.
30. Mourad-Baars PE, Verspaget HW, Mertens BJ, Mearin ML. Low prevalence of
Helicobacter pylori infection in young children in the Netherlands. Eur J Gastroenterol Hepatol. 2007; 19(3):213–216. PMID:
17301647.
31. Zabala Torrres B, Lucero Y, Lagomarcino AJ, Orellana-Manzano A, George S, Torres JP, et al. Review: prevalence and dynamics of Helicobacter pylori infection during childhood. Helicobacter. 2017; 22(5):e12399.
32. Andersen LP, Rosenstock SJ, Bonnevie O, Jørgensen T. Seroprevalence of immunoglobulin G, M, and A antibodies to
Helicobacter pylori in an unselected Danish population. Am J Epidemiol. 1996; 143(11):1157–1164. PMID:
8633606.
33. Raymond J, Sauvestre C, Kalach N, Bergeret M, Dupont C. Immunoblotting and serology for diagnosis of
Helicobacter pylori infection in children. Pediatr Infect Dis J. 2000; 19(2):118–121. PMID:
10693997.
34. Cho MJ, Lee WK, Jeon YS, Kim KH, Kim SH, Baik SC, et al. Intrafamilial transmission of Helicobacter pylori detected by random amplified polymorphic DNA fingerprinting. Mol Cells. 1995; 5(5):508–513.
35. Kivi M, Tindberg Y, Sörberg M, Casswall TH, Befrits R, Hellström PM, et al. Concordance of
Helicobacter pylori strains within families. J Clin Microbiol. 2003; 41(12):5604–5608. PMID:
14662948.
36. Krueger WS, Hilborn ED, Converse RR, Wade TJ. Environmental risk factors associated with
Helicobacter pylori seroprevalence in the United States: a cross-sectional analysis of NHANES data. Epidemiol Infect. 2015; 143(12):2520–2531. PMID:
25592266.
37. O'Ryan ML, Rabello M, Cortés H, Lucero Y, Peña A, Torres JP. Dynamics of
Helicobacter pylori detection in stools during the first 5 years of life in Chile, a rapidly developing country. Pediatr Infect Dis J. 2013; 32(2):99–103. PMID:
23076385.
38. Seo JH, Park JS, Rhee KH, Youn HS. Diagnosis of
Helicobacter pylori infection in children and adolescents in korea. Pediatr Gastroenterol Hepatol Nutr. 2018; 21(4):219–233. PMID:
30345235.
39. Jun JS, Seo JH, Park JS, Rhee KH, Youn HS. Changes in the treatment strategies for
Helicobacter pylori infection in children and adolescents in Korea. Pediatr Gastroenterol Hepatol Nutr. 2019; 22(5):417–430. PMID:
31555566.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download