INTRODUCTION
Permanent newborn hearing loss is a common congenital disease that occurs in 1–3 of every 1,000 newborns.
1 Early detection of hearing loss and the initiation of early aural rehabilitation in newborns with hearing loss is important for the development of language ability, cognitive skills, and social-emotional skills.
23 In newborns and infants, hearing difficulties are not easily detected by routine clinical procedures such as behavioral observation. It is recommended that all newborns undergo newborn hearing screening (NHS) within 1 month of birth, newborns who are referred after NHS undergo a confirmatory hearing test within 3 months of birth and early intervention for hearing impaired infants is performed within 6 months of birth.
45 The impact of hearing loss on language development is greatest for newborns who are born with hearing loss or who experience hearing loss shortly after birth.
6 At birth, the peripheral auditory organs are completely developed, whereas the auditory cerebral cortices rely on sound stimulation during the first 2–3 years of life to develop.
7 It has been discovered that hearing impaired infants should begin aural intervention within 6 months of birth to facilitate advanced language development.
6
Universal newborn hearing screening (UNHS) has been carried out in many developed countries.
489 It was found that 50% of newborns with congenital hearing loss are healthy babies without risk factors such as familial history of hearing loss, meningitis, and congenital cytomegalovirus.
410 In Korea, a government-supported NHS pilot project had been conducted since 2007, and national health insurance has covered the NHS for all newborns since October 2018.
11 In addition economic support for the NHS, there is a need to monitor and evaluate the quality and performance of screening and diagnosis.
4 To achieve high-quality and successful early hearing detection and intervention (EHDI), it is necessary to analyze regional NHS data from a previous pilot project and ensure that the whole country, which includes 17 major cities and provinces, is operating EHDI to a high standard. Thus far, there are no reports that analyze regional NHS data and investigate the differences between various Korean cities and provinces.
Thus, the purpose of this study was to present and analyze the results of government-supported nationwide NHS pilot projects across 5 years in 17 major Korean cities and provinces. Ultimately, we have tried to analyze the differences in the screening state depending on the 17 cities and provinces and associated factors, which would help to establish policy to detect and support hearing loss infants effectively and to control qualities of NHS program.
DISCUSSION
The NHS pilot project, supported by the Korean government, was introduced in 2007. Since 2009, it has expanded to newborns of low-income families across the country using vouchers. Vouchers of the NHS pilot project were used to track and manage the results of screening and ABR tests. During the pilot period, newborn screenings in families not eligible for government support were carried out at the expense of the parents. Since October 2018, all newborns have been covered by national health insurance, however, individual and regional tracking and statistical analysis is not possible. This is because the government supports only the screening tests and has not yet established a system to track and manage infants with hearing loss. As far as the authors know, no paper has reported on the nationwide regional characteristics of NHS in Korea, and this is the first paper to report the characteristics of NHS in 17 cities and provinces for the first time in Korea using the data from the government-funded NHS pilot study.
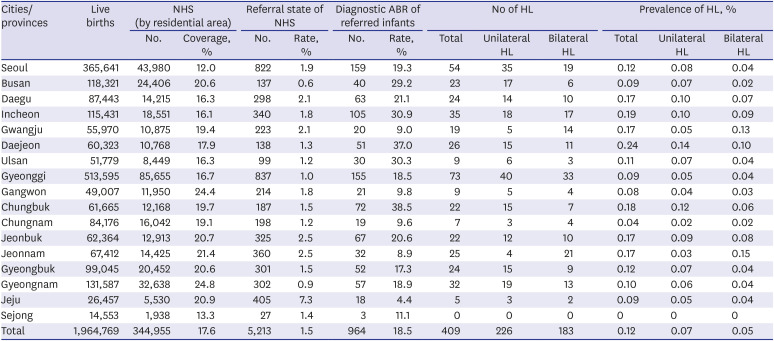
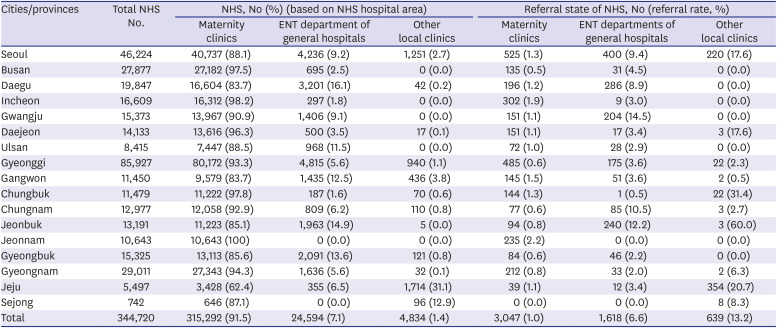
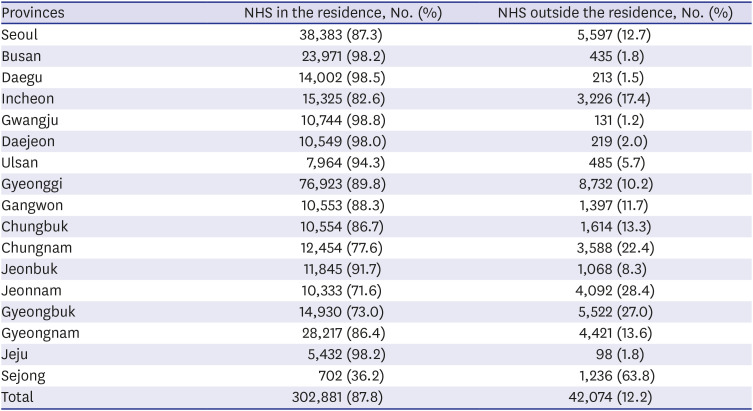
Newborns who received support as part of the pilot project accounted for 17.6% of all live births in Korea. NHS pilot program screening coverage rates vary between cities and provinces. Notably, the coverage rates in Gyeongsang, Jeolla, Gangwon, Jeju, and Busan provinces were more than 20%, which is higher than the national average. The pilot project targeted mainly low-income families, and it could be inferred that the proportion of low-income families eligible for NHS support was higher than other provinces. Screening rates by NHS hospitals also showed regional differences. Although 91.5% of overall screening tests were performed in maternity clinics nationwide, the screening coverages of maternity clinics in Gangwon (83.7%), Daegu (83.7%), and Jeju (62.4%) were less than 85%. Additionally, the screening rates of primary local clinics in Gangwon (3.8%) and Jeju (31.1%) were comparatively higher than those in other provinces. This phenomenon was related to Korea's low fertility rate. The total fertility rate was 1.2 in 2014 and 0.92 in 2018, the lowest in the world.
15 In addition, the number of maternity clinics offering hearing screening is gradually decreasing as a result of the low fertility rate.
16 In the areas where there are very few delivery institutions as in Jeju and Gangwon, the need for a linking system that connects the maternity clinics that do not have a NHS device with the ENT clinics with a device should be considered for newborns to undergo timely screening tests.
In the present study, the screening rate varied according to factors such as regional income level, birth rate, and maternity distribution. Therefore, the government should establish a support policy for EHDI according to the regional specificities. It would be useful to facilitate an integrated system by providing inter-hospital linkages and practical NHS device support that would subsequently enable screening tests at other primary institutions that do not have an NHS device.
Several NHS guidelines and some states in North America recommend the following: 1) infants who did not pass the rescreen should not continue to further screening, 2) the referral rate of the primary NHS test within 3 months of starting an NHS program should be maintained to not exceed 8%, 3) the referral rate at the rescreen of the outpatient hospital should be maintained not to exceed 4%, 4) babies born through a cesarean section should be screened after more than 24 hours post-birth to allow debris in the ear canal to clear, and 5) at least 95% of newborns should be screened before discharge or within 1 month of birth.
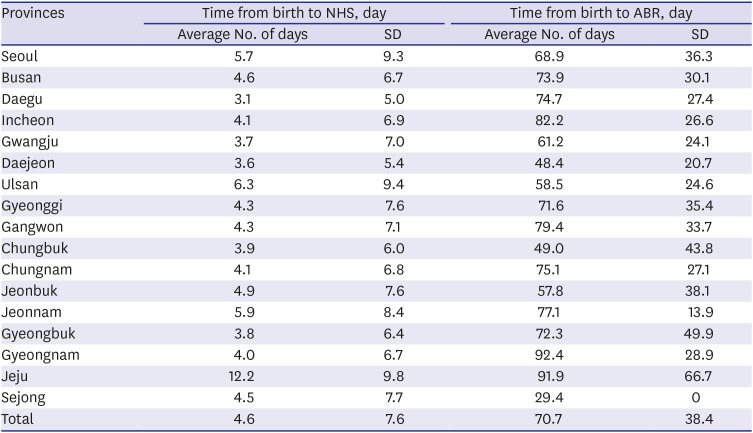
451718 In this study, the mean referral rate was 1.5%; however, regional referral rates varied from 0.6% (Busan) to 7.3% (Jeju). The reason why Jeju's referral rate was higher than other regions was because that in Jeju, screening had not been routinely performed before discharge from a birthing facility, instead it had been performed at an outpatient ENT or other primary clinic. The number of NHS tests performed at local primary clinics was less than that performed at large-scale maternity clinics or hospitals; therefore, screener bias or operator error may be the reason for the high referral rate. Another reason for the higher referral rate could be the later screening time that coincides with newborns' shorter natural sleep time and increases the tendency of more movement. The referral rate in Busan was low, at only 0.6%, which is problematic due to the possibility of false negatives. According to an unpublished survey conducted by the Ministry of Welfare in 2010, some screening facilities misidentified the screening test as a confirmatory test and repeated the test more than 10 times. The Joint Committee on Infant Hearing (JCIH), along with other guidelines, recommends that the screening test is performed a maximum of twice, as it is possible to accidentally achieve a “pass” result when repeating the automated screening test.
4517 To solve these problems, the Korean otology and audiological societies have produced guidelines
5 and provided online training to provide continuous education for screeners; however, national education and surveillance are ultimately required.
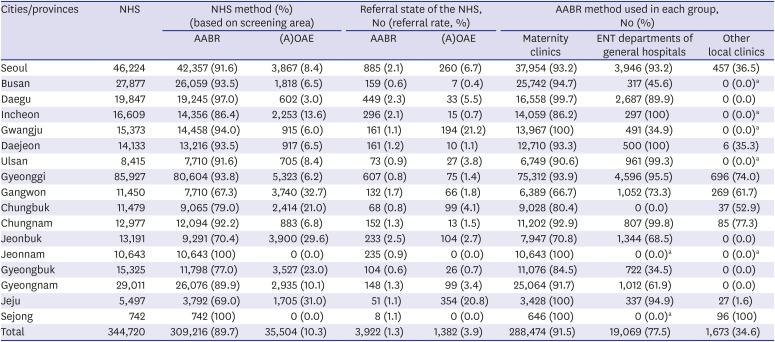
The referral rate in maternity clinics was found to be less than 4%; however, the referral rates in Busan (0.5%), Gyeonggi (0.5%), Chungnam (0.6%), and Gyeongbuk (0.6%) were less than 1%. The referral rates in ENT departments varied from 0.5% to 14.5%. The high referral rates in ENT departments of general hospitals in Seoul, Daegu, Chungnam, and Jeonbuk were thought to be due to the fact that newborns with hearing loss risk factors were usually hospitalized and treated in the neonatal intensive care unit of general hospitals. The referral rates of (A)OAE were generally higher than those of AABR, with 65.1% in some regions. Especially, in Jeju, the referral rate of (A)OAE was very high (20.8%), and 98.4% of other local clinics performed screening with (A)OAE. It can be necessary to check the (A)OAE methodology and conduct a quality evaluation in Jeju's screening clinics. The referral rates according to the NHS method also differed significantly according to the device and the region. The average referral rate was 1.3% for AABR and 3.9% for (A)OAE. The referral rate of AABR was significantly lower than that of (A)OAE. In some countries, AABR has a low referral rate; hence, nationally, it is recommended that only AABR is used as an NHS test to reduce the referral rate and prevent the waste of resources.
19 In this study, 89.7% of newborns involved in a Korean pilot program underwent screening using AABR. Local clinics primarily used (A)OAE (65.4%); therefore, it may be possible to consider maintaining the appropriate referral rates by promoting, supporting, and providing training on AABR across the country.
Although a diagnostic ABR test is currently covered by national health insurance at about 70%, the remaining cost for the ABR test has been supported by the public health center if the parents submit the ABR result and its receipt. One of the reasons for the low diagnostic ABR rate may be the inconvenience of the refund process for co-payments. If the parents whose infants had undergone ABR testing did not request a refund at the public health center, then the results were not included in the data. The introduction of national hearing coordinators or automatic guidance systems, such as vaccinations, may be considered so that the infants who did not pass NHS can be tested at an appropriate time for diagnostic ABR tests by caregivers.
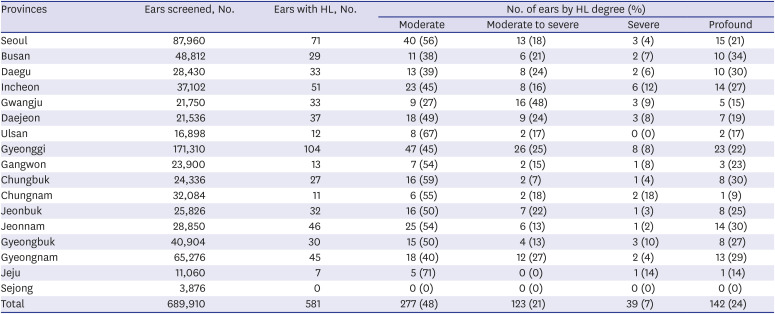
The prevalence of hearing loss was 0.12% (≥ 40 dB nHL); however, this was the result of only 18.5% of the referred newborns who underwent ABR. Thus, the actual prevalence of hearing loss should consider the ABR performing rate. Subsequently, the overall hearing loss adjusted prevalence with ABR rate was 0.64% (0.35% on one side, 0.29% on both sides). The prevalence of UNHS-detected hearing loss in highly developed countries is 0.11%
20; however, it is difficult to simply compare the prevalence of hearing loss because the definition of hearing loss and the diagnostic ABR rate varies by countries and papers. The government needs to make efforts to increase the ABR performing rate after an NHS test, not to fade the meaning of EHDI to help children with hearing loss.
The analysis of early intervention using simple telephone surveys by the public health center staff did not work well in the pilot project. Infants with bilateral hearing loss of more than 60 dB were required to register for national hearing impaired status to receive early intervention such as hearing aids or cochlear implants. During the pilot project, there was no government support for infants with bilateral hearing loss up to 40–59 dB in Korea. Since 2019, The Ministry of Health and Welfare has started to provide one hearing aid to children with 40–59 dB hearing loss (under 3 years of age) who are unable to register for national hearing-impaired status. Even though NHS has been performed universally in Korea since October 2018, the results of screening and confirmatory tests are unknown, and it is still impossible to trace the intervention state. Therefore, it is necessary to establish a data management service and a tracking system so that children with hearing loss can be detected early and undergo timely intervention such as in the United States
21 and the United Kingdom.
22
The study of the government-led NHS pilot project mainly included newborns of low-income families. Therefore, the results and statistics of this study do not represent all of Korea, and this is a limitation of this study. However, as many as 17.6% of total live births were included nationwide and there were no formal national statistics about NHS prior to the application of the national health insurance in October 2018; thus, this study provides the first statistical results that can describe the regional NHS status in Korea. Another limitation of this study is that the criteria for hearing loss were determined only by the diagnostic ABR results. The proportion of unilateral sensorineural hearing loss in congenital hearing loss is known to be about 30%–40% in developed countries.
23 Among the hearing-impaired children in this study, the proportion of bilateral hearing loss was 44.7% (183 out of 409 newborns with hearing loss) and that of unilateral hearing loss was 55.3% (226 out of 409 newborns with hearing loss). The reason that the proportion of bilateral and unilateral hearing loss was different from other literature results is because hearing loss of this study was diagnosed based on the results of the diagnostic ABR test only, and conductive hearing loss as well as sensorineural hearing loss was included in this study. Herein, the prevalence of bilateral hearing loss and unilateral hearing loss had almost the same rate in Jeonbuk, Gyeonggi, Gangwon, Chungnam and Jeju. In order to accurately classify the type of hearing loss in future studies, it is necessary to analyze not only the ABR results but also the eardrum findings and tympanometry results.
The NHS guidelines recommend one-step or two-step NHS (AABR after OAEs or AABR), depending on the hospital system and circumstances.
45 The two-step NHS test was reported to significantly decrease the referral rate when compared with the one-step NHS test.
2425 However, as a support procedure, we only analyzed the results of one-step NHS, because the Korean Ministry of Health and Welfare only provided financial support for one hearing screening. If two-step NHS were performed, the referral rate might be < 1.5%. As we mentioned above, some maternity clinics with AABR tended to repeat the NHS test at a single test cost, and these institutions had low referral rates. On the other hand, if a screening test was performed in the outpatient primary clinic, the screening test was carried out in a one-step method, and the referral rate could be high. Therefore, it is necessary for the government to conduct continuous education on NHS guidelines and quality control for screening hospitals. The last limitation of this study was that the risk factors of hearing loss were not reflected in the analysis of the regional NHS results in this study. The investigation of the risk factors of hearing loss and regular hearing screening are very important in detecting delayed-onset or progressive hearing loss. However, this study was carried out using vouchers of the government-led pilot project. The voucher contained only one risk factor, admission to the neonatal intensive care unit (NICU) for more than 5 days, among JCIH risk factors associated with hearing loss. The study aimed to review regional NHS characteristics and did not include the results for newborns admitted to NICU for more than 5 days. In future studies, we plan to report the results of the NHS tests of infants who were admitted to NICU for more than 5 days. When the government establishes an EHDI management system for children with hearing loss, it is necessary to manage not only the NICU admission but also other risk factors.
In conclusion, although the NHS and following diagnostic ABR was conducted in a timely manner, there were significant differences in the screening rates and referral rates by screening hospital type and NHS method depending on the cities and provinces in Korea. For successful EHDI and quality control, it will be necessary to provide support according to the regional NHS requirements and ensure that the whole country is included through the establishment of a national data-management and tracking system that integrates infants and children into the healthcare system.




 PDF
PDF Citation
Citation Print
Print




 XML Download
XML Download