A Better Understanding of Social Distancing
Social distancing is also called physical distancing. The term social distancing is usually used, but the word 'society' gives the nuance of being alienated from the group I live in, so it is recommended that it be better to call it physical distance. Nevertheless, the term social distancing is still preferred. By definition, this is a whole set of ways to reduce the frequency of physical contact between people and to reduce their frequency as much as possible to reduce the risk of disease transmission. The goal is to slow the spread of the corona virus disease 2019 (COVID-19) as much as possible so that the health care system of a country runs smoothly without overload. Hence social distancing is inseparable from the so-called ‘flattening the curve’.
12 In fact, flattening the curve is a concept that becomes complete when ‘raising the line (expanding the health care capacity)’ is performed simultaneously.
At this point, let's make sure to define one key point of social distancing that many people may misunderstand. Social distancing alone does not completely terminate the COVID-19 epidemic. To be more honest, it cannot eventually stop COVID-19 from spreading. This is a really uncomfortable truth. Let's revisit the definition of social distancing mentioned above. Social distancing is a means to ‘slow down’ the rate at which the disease spreads, not a complete blockade. The definition implies the frightening premise that all of us will someday get COVID-19 anyway if we do not have a specific antiviral agent or vaccine.
Then, why do we implement social distancing?
If the disease spreads rapidly and exceeds the range that can be handled, it can become a heavy burden to even the best medical system and facilities. Even if they could barely deal with the burden, the tragic situation in which critical patients are dying due to lack of medical resources is unfolding.
Once we have grasped the concept of social distancing, we will have an answer on what to do in the future: We have no choice but to save physical space and time to treat every sick and severe patient.
Minimizing the physical contact of each member of society could slow the spreading speed of COVID-19. Then, the outbreak of patients will occur as slowly as possible, and from a medical staff's point of view, they can take care of them all with relatively sufficient time and physical margin to handle the medical facilities. What this means is to keep the disease in a controllable range while minimizing damage until antivirals and vaccines are developed. Of course, we could go for a more relaxed policy, but we have to acknowledge the harsh reality that it may eventually be a measure that will never end.
Go to :

Menu of Social Distancing and Difference with Lockdown
Among the various menus of social distancing, the most basic is isolation and quarantine. Isolation targets confirmed patients as well as those with suspicious symptoms. The quarantine is applied on asymptomatic close contacts. A more stringent policy is to ban people from moving or rallying. The prohibition of movement ranges from preventing travel to distant places, unless it is necessary, to banning people from going out of their house for a certain period of time. If it reaches the level of mandatory prohibition, it is rather classified as a lockdown than social distancing.
Strict immigration procedures at international airports may also fall into the category of social distancing, but they are actually a sort of border restriction. Therefore, they are more likely to be classified as lockdown. In fact, lockdown is a kind of social distancing category, but the distinction is somewhat ambiguous.
If the department that implements the social distancing policy is not a health authority but is directly led by the government and is subjected to strictness and penalties for violations, it can be classified as a lockdown. Prohibition of rally or mass gathering is applied collectively or selectively according to circumstances. Enforcing the school closure is controversial. Because, in particular, most children and adolescents tend to be asymptomatic or mildly ill, it is presumed that they are more at risk of spreading the disease to elderly. This is based on past flu pandemic experience.
34 In addition, although not perfect, a simulation study of COVID-19 also suggested the possibility of increase in the number of new cases by asymptomatic or mild pediatric patients soon after re-opening schools.
5 However, in the case of Sweden which will be immediately mentioned later, the assumption has not been accepted because they thought it has not yet been directly proven yet, which has also been one of the bases of their strategy against COVID-19.
Go to :

Sweden's Lenient Strategy against COVID-19
Sweden devised a strategy by looking at and approaching the dynamics of COVID-19 from a different perspective: COVID-19 is highly contagious and cannot be completely eradicated. As mentioned earlier, even if social distancing is used, the premise is that the disease spreads all over the country anyway. After all, until vaccines and antiviral drugs are released, it is the same that they cannot be completely blocked. Although the mortality rate is high in the elderly, the youngers are suffering from mild illness. However, the rate of transmission is very fast, and the Swedish medical and health care capacity is not enough to cover all patients. Therefore, they mainly focus on the seriously ill and let the rest go. And social distancing is conducted nationwide. Like any other country, if we enforce strict social distance or lockdown, we can control the epidemic right away, but as time goes by, we must pay the price for the depression and disruption of domestic socio-economic system. Considering this, lockdown will never be enforced, and social distancing will be conducted with a lenient way.
67
They seem to have set the basic principles as described above, and have begun fighting the COVID-19. Therefore, they did basic social distancing, but all the schools were open so that they could have a regular academic schedule, and the workplace was encouraged to work at home, but it was not mandatory, and the socio-economic activities were generally allowed as usual. When a confirmed patient comes out, if it is mild, he or she will stay at home if possible, and adheres to the policy of focusing on hospitalization of patients with severe or elderly conditions.
In summary, it was a defense strategy with maximum autonomy.
Some have interpreted the strategy as aiming to end the COVID-19 epidemic by inducing herd immunity, but Swedish health authorities strongly deny it. However, in my personal opinion, anyway, if they operate with such a strategy, they will inevitably go to establish the herd immunity. Anyway, as a result of coping with the epidemic through this policy, the Swedish society itself seems to work well. However, when Sweden's morbidity and mortality rates are compared with those of Korea, it shows quite different results from our point of view as shown in
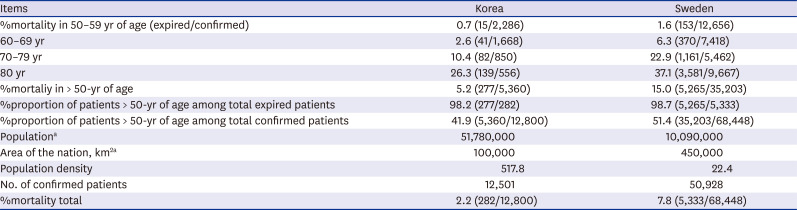
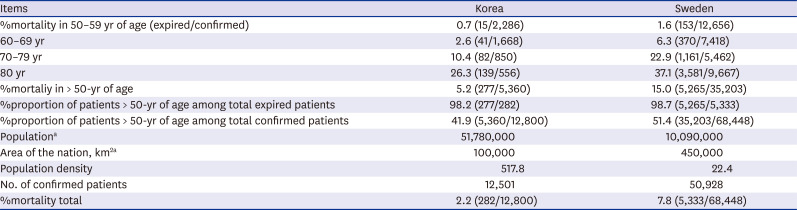
Table 1.
89
Table 1
Comparison of coronavirus disease 2019 statistics between Korea and Sweden (as of June 30, 2020)
|
Items |
Korea |
Sweden |
|
%mortality in 50–59 yr of age (expired/confirmed) |
0.7 (15/2,286) |
1.6 (153/12,656) |
|
60–69 yr |
2.6 (41/1,668) |
6.3 (370/7,418) |
|
70–79 yr |
10.4 (82/850) |
22.9 (1,161/5,462) |
|
80 yr |
26.3 (139/556) |
37.1 (3,581/9,667) |
|
%mortaliy in > 50-yr of age |
5.2 (277/5,360) |
15.0 (5,265/35,203) |
|
%proportion of patients > 50-yr of age among total expired patients |
98.2 (277/282) |
98.7 (5,265/5,333) |
|
%proportion of patients > 50-yr of age among total confirmed patients |
41.9 (5,360/12,800) |
51.4 (35,203/68,448) |
|
Populationa
|
51,780,000 |
10,090,000 |
|
Area of the nation, km2a
|
100,000 |
450,000 |
|
Population density |
517.8 |
22.4 |
|
No. of confirmed patients |
12,501 |
50,928 |
|
%mortality total |
2.2 (282/12,800) |
7.8 (5,333/68,448) |

First of all, the death rate per number of confirmed patients in Korea is about 2%, while that in Sweden is around 7%–8%. In addition, Sweden's mortality rate among people over age of 50 (elderly) is higher than that of Korea. Sweden has only one fifth of population of Korea. Population density is also lower than ours. However, Sweden has a much higher number of confirmed persons per population size than Korea. In a way, this may be a natural result. Lockdown was never implemented, and relaxed social distancing would not have significantly slowed the rate of disease transmission. But how would it be explained that many elderly people died?
However, if you look at these statistics more carefully, they can be interpreted differently.
In the proportion of the elderly among the dead, Korea accounted for 98.2% and Sweden for 98.7%. There is no significant difference. After all, both countries showed the same result in that the elderly and vulnerable group had a bad prognosis. It would be more accurate to interpret the higher mortality rate as actually revealing the problems in terms of patient care, rather than failure of their defense strategy.
I think Sweden has made trial and error in the following aspects. They seem to have underestimated the consequences of asymptomatic transmission.
1011 And the formation of herd immunity appears to be less beneficial than expected. In fact, several studies have shown that natural immunity to coronavirus does not last long.
1213 Immunity to colds is less than half a year, and immunity to severe acute respiratory syndrome or Middle East respiratory syndrome coronavirus is about 1-3 years, which is based on the results of small-scale.
141516 In any case, it is certain that immunity against coronavirus is not permanent, so even if herd immunity is formed, there is no way to stop getting it again when the seasons change.
Go to :

I Do Not Think Sweden's Strategy Has Failed.
There is something we should not misunderstand about the Swedish policy. They never let COVID-19 spread, and they did all the appropriate social distancing, while they just don't have strict lockdowns like border restrictions or school and workplace closures.
67
Keep in mind that the current COVID-19 pandemic is just the beginning. We can't argue that a stringent policy is not always right, and we shall have to look at the final result after at least one or two years to see if the Swedish lenient strategy is wrong or more correct than the strict one.
Anyway, after paying the price of such a severe hardship, Sweden now seems to be flattening their curve.
9
In addition to Sweden, France, Spain, and the United Kingdom, which had high mortality rates, have also entered a stabilization trend. These countries are now beginning to alleviate the social distancing policy. Their starting points were different, but from the time these countries began to relax the policy, they are changing in some ways like Sweden. Sweden is also taking lessons from the trials and errors pointed out above, and supplementing and improving their policies. It may have started as a less stringent strategy, but it will have a lot of potential to evolve into a reasonable and effective defense policy.
There is another point.
Which country do you think is the most contrary to Sweden's policy?
Republic of Korea?
No.
Taiwan.
First of all, Taiwan has thoroughly implemented lockdown such as border restrictions with China at the beginning of the war against COVID-19, even though Taiwan's dependence on China's trade economy is much higher than that of Korea. As of June 2020, there are about 400 confirmed cases, and fewer than 10 have died.
17 There is still much debate as to whether it was right not to do border closures or travel ban at the beginning of the epidemic.
181920 However, it is clear that the current outbreak of COVID-19 in countries where border restrictions have been thoroughly enforced from the beginning, such as Taiwan, has entered a stable phase.
Korea's initial policy is similar to that of Sweden except for postponing school opening and taking care of all confirmed patients. We have not implemented hardcore measures such as lockdown, border closures, and travel bans like Sweden. Moreover, if our social distancing policy is gradationally mitigated, it will gradually become more similar to Sweden's. This can lead to two contradictory interpretations and prospects as follows.
One is that the Swedish policy should have been put in place only after the epidemic had stabilized to some extent, not in the early stage.
On the other hand, in terms of our policy of not locking down, someday we may have met the same hardships that Sweden experienced. Even if the starting point is different, the singularity with no difference between Sweden or other countries will come at the end of the pandemic.
Go to :

How Will It All End?
Now everyone is exhausted and comes up with the following common question: How long should we keep social distancing? The answer is until COVID-19 ends. However, complete termination is not possible until specific antivirals and vaccines are developed. Until that point, social distancing must go on.
Do not let us just look at Sweden's policy negatively. Wouldn't it be worth taking seriously to consider it as an alternative? I am not trying to determine whether the Swedish policy is inferior to Korean or Taiwanese. At least at this point, they are facing with high number of confirmed patients and high mortality rates, but I think the Swedish strategy in the overall framework is also worth considering seriously. Unless vaccines and antivirals are available, this war will never end and will repeat every year. I am wondering how we can endure another COVID-19 that will come back this winter in an obvious battle where the economy might be disrupted and medical resources exhausted.
Swedish policy may be difficult to accept emotionally with our viewpoint. If the current COVID-19 situation persists even if there is no major explosion, the time will come to reconsider the measures currently being implemented. In other words, we should now be considering even the steps to accept COVID-19 as a member of our society, like a cold or influenza. I know it is an uncomfortable truth. In this regard, I think it would be better to review the current policies of Sweden as an alternative reference, not just criticize them.
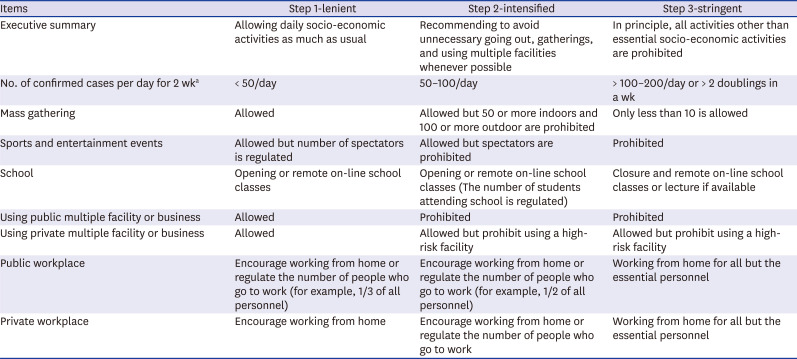
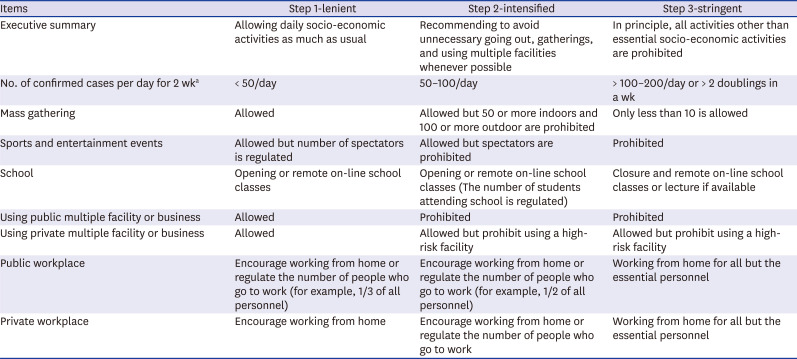
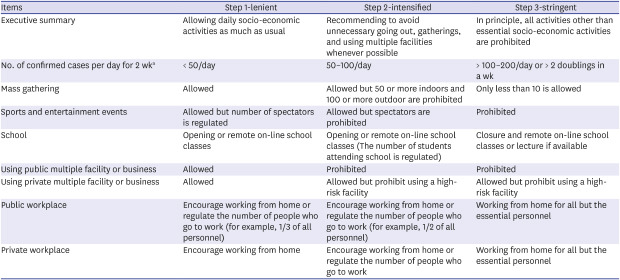
As of June 28, 2020, the social distancing policy has been changed to a step-by-step response guideline as summarized in
Table 2.
21
Table 2
Guideline for 3 steps of social distancing formally announced by Korean Ministry of Health and Welfare and Central Disaster Safety Task Force under the Korean Ministry of the Interior and Safety on June 28, 2020
|
Items |
Step 1-lenient |
Step 2-intensified |
Step 3-stringent |
|
Executive summary |
Allowing daily socio-economic activities as much as usual |
Recommending to avoid unnecessary going out, gatherings, and using multiple facilities whenever possible |
In principle, all activities other than essential socio-economic activities are prohibited |
|
No. of confirmed cases per day for 2 wka
|
< 50/day |
50–100/day |
> 100–200/day or > 2 doublings in a wk |
|
Mass gathering |
Allowed |
Allowed but 50 or more indoors and 100 or more outdoor are prohibited |
Only less than 10 is allowed |
|
Sports and entertainment events |
Allowed but number of spectators is regulated |
Allowed but spectators are prohibited |
Prohibited |
|
School |
Opening or remote on-line school classes |
Opening or remote on-line school classes (The number of students attending school is regulated) |
Closure and remote on-line school classes or lecture if available |
|
Using public multiple facility or business |
Allowed |
Prohibited |
Prohibited |
|
Using private multiple facility or business |
Allowed |
Allowed but prohibit using a high-risk facility |
Allowed but prohibit using a high-risk facility |
|
Public workplace |
Encourage working from home or regulate the number of people who go to work (for example, 1/3 of all personnel) |
Encourage working from home or regulate the number of people who go to work (for example, 1/2 of all personnel) |
Working from home for all but the essential personnel |
|
Private workplace |
Encourage working from home |
Encourage working from home or regulate the number of people who go to work |
Working from home for all but the essential personnel |

We must go to a tedious and long war, either by mitigating or reinforcing social distancing by following the guidelines provided by governments and health authorities. This is the reality we are facing now. For the time being, it is difficult to expect the termination of COVID-19, so the first step is now something we should always keep. Let's not forget that what we enjoy in step 1 is the best. Without self-restraint, it is difficult to enjoy even this. If step 1 remains as it is now, you may soon be able to go to the ballpark and watch the game. However, if you do not, things can get worse and go into the step 2. It depends on our obedience of the guideline.
Go to :





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download