This article has been
cited by other articles in ScienceCentral.
Abstract
Background
Mortality of coronavirus disease 2019 (COVID-19) is a major concern for quarantine departments in all countries. This is because the mortality of infectious diseases determines the basic policy stance of measures to prevent infectious diseases. Early screening of high-risk groups and taking action are the basics of disease management. This study examined the correlation of comorbidities on the mortality of patients with COVID-19.
Methods
We constructed epidemiologic characteristics and medical history database based on the Korean National Health Insurance Service Big Data and linked COVID-19 registry data of Korea Centers for Disease Control & Prevention (KCDC) for this emergent observational cohort study. A total of 9,148 patients with confirmed COVID-19 were included. Mortalities by sex, age, district, income level and all range of comorbidities classified by International Classification of Diseases-10 based 298 categories were estimated.
Results
There were 3,556 male confirmed cases, 67 deaths, and crude death rate (CDR) of 1.88%. There were 5,592 females, 63 deaths, and CDR of 1.13%. The most confirmed cases were 1,352 patients between the ages of 20 to 24, followed by 25 to 29. As a result of multivariate logistic regression analysis that adjusted epidemiologic factors to view the risk of death, the odds ratio of death would be hemorrhagic conditions and other diseases of blood and blood-forming organs 3.88-fold (95% confidence interval [CI], 1.52–9.88), heart failure 3.17-fold (95% CI, 1.88–5.34), renal failure 3.07-fold (95% CI, 1.43–6.61), prostate malignant neoplasm 2.88-fold (95% CI, 1.01–8.22), acute myocardial infarction 2.38-fold (95% CI, 1.03–5.49), diabetes was 1.82-fold (95% CI, 1.25–2.67), and other ischemic heart disease 1.71-fold (95% CI, 1.09–2.66).
Conclusion
We hope that this study could provide information on high risk groups for preemptive interventions. In the future, if a vaccine for COVID-19 is developed, it is expected that this study will be the basic data for recommending immunization by selecting those with chronic disease that had high risk of death, as recommended target diseases for vaccination.
Keywords: COVID-19, Comorbidities, Chronic Diseases, Mortality Risk
INTRODUCTION
After the coronavirus disease 2019 (COVID-19) in December 2019 in Wuhan, China, the first confirmed patient occurred on January 20 in Korea. And, some sporadic influx occurred mostly from abroad. However, in the middle of February, starting with patient number 31 in the Daegu region, a massive outbreak of COVID-19 occurred in that region and followed by nationwide outbreaks.
1
In the case of representative influenza of respiratory diseases, it is known that chronic disease patients have a reduced immune function due to the underlying disease, which increases the susceptibility to infection that increases the risk of complications such as dysfunction of other organs and exacerbation of the underlying disease or death.
2 In the Wan et al study of China, 31.9% of all 135 hospitalized patients with COVID-19 had underlying disease.
3 The Chen et al.
4 study showed that 36.1% of the total 249 patients with COVID-19 had comorbidity. In addition the Jian-ya
5 study found that 7 out of 51 patients who were discharged were severe, and 6 of them had comorbidity.
In Korea, the mass outbreak of COVID-19 involving the worship of a religious group has become the starting point for the nationwide spread. However, the current situation of community infection is caused by various factors. Most of the deaths were classified as high-risk group, and shown to have high mortality rate when accompanied by underlying disease.
1 Therefore, the purpose of this study is to contribute to the establishment of effective quarantine measures by identifying comorbidities affecting deaths caused by COVID-19 and selecting high-risk groups that require preemptive precautions.
The specific purpose is as follows.
1) Identify the general characteristics of the patients and the crude death rate (CDR).
2) Present the status of history of comorbidity of the study subjects.
3) Identify epidemiological factors affecting the death of the study subjects.
4) The relationship between chronic diseases and death among the comorbidities of the study subjects is comprehensively identified.
METHODS
Registry data of Korea Centers for Disease Control and Prevention (KCDC) of confirmed COVID-19 up to March 26, 2020 and the database of Korean National Health Insurance Service (KNHIS) has been linked to be used as study data.
16
A total of 9,148 subjects were reported by the KCDC, 3,556 males (39.0%) and 5,592 females (61.0%) were identified. A total of 9,148 subjects in the registry data from the KCDC were linked to the NHIS DB's population/health insurance premium table, and workplace table to extract income level variables reflecting the residential area and insurance type. It was considered to have a history of the comorbidity if the medical statement data satisfies the conditions of hospitalization for more than three days, or outpatient visits for more than four days, or prescriptions for medicines for more than 28 days annually, between 2002 and 2019. Sex, age, and death variables were used in the registry data from the KCDC.
The χ2 test was used to see the difference between the general characteristics of patients diagnosed with COVID-19 and their death status in connection with the registry data from the KCDC and the NHIS's database, which came up with the CDR. In addition, the history of comorbidity of confirmed patients according to the classification group of 298 diseases was confirmed. Lastly, to examine the relationship between precedent chronic disease among epidemiologic factors and comorbidity, affecting death in patients who were confirmed, multivariate logistic regression analysis was performed, along with odds ratio and 95% confidence interval (CI) calculation. All analyzes were analyzed using SAS 9.4 (SAS Institute Inc., Cary, NC, USA), and the statistical significance level was indicated to be less than P value 0.05.
Ethics statement
This study was exempted from deliberation by the Yonsei University Institutional Review Board (IRB) for the exemption from IRB deliberation that does not include personally identifiable information (CR320311).
RESULTS
General characteristics and survey mortality rate
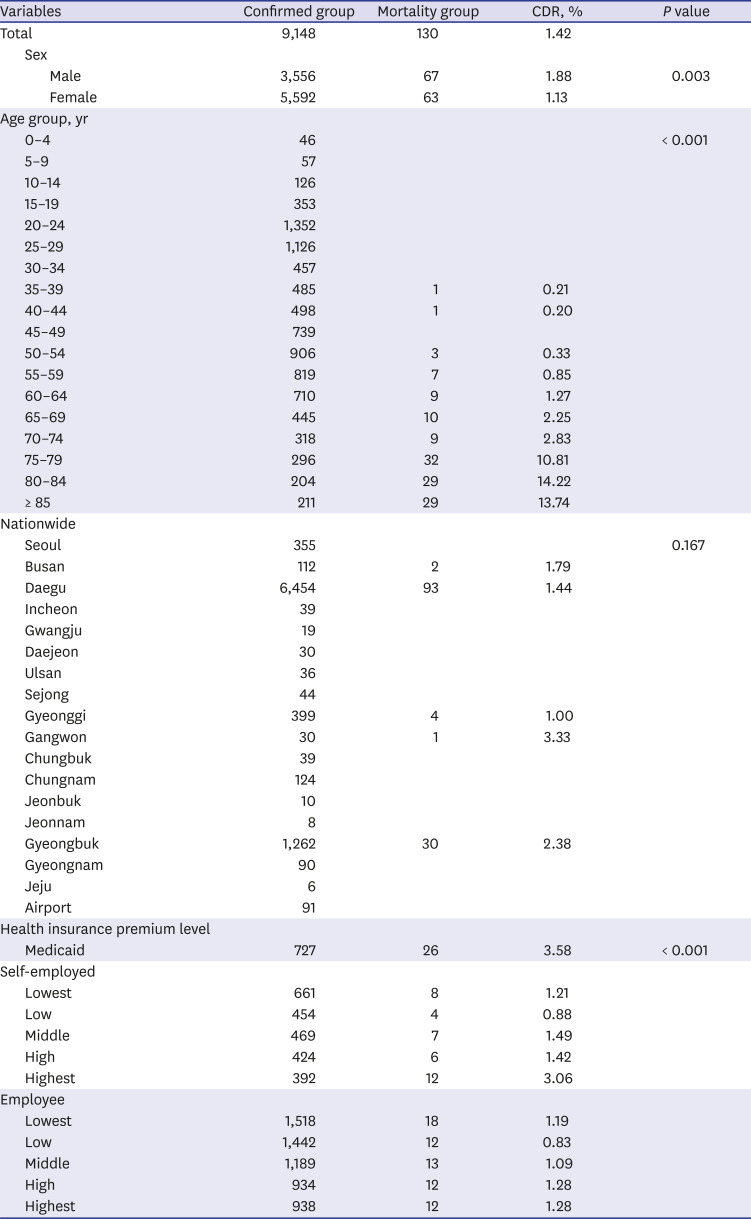
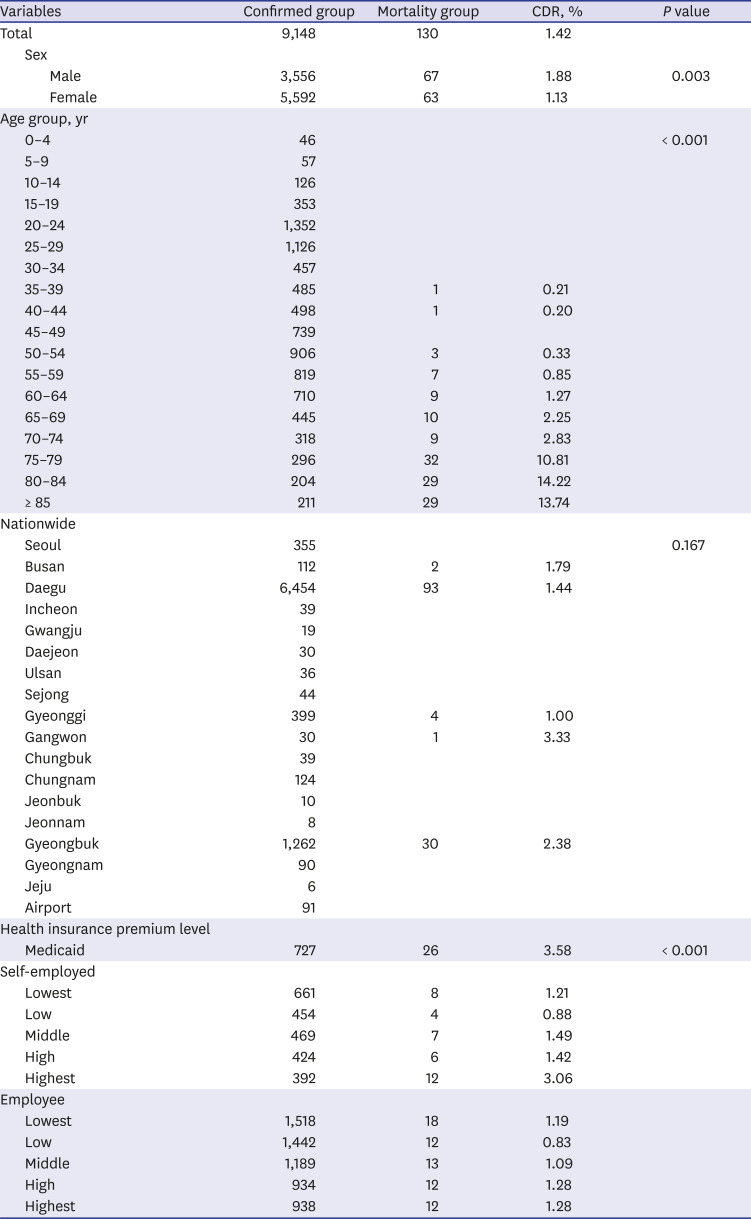
Looking at the general characteristics of the study subjects, 67 deaths were found among 3,556 males confirmed patients, and the mortality rate was 1.88% (
Table 1). Of the 5,592 females, the death was 63, and the mortality rate was 1.13%. Looking at the age group, the highest number of confirmed patients was between 20 to 24 years old and 1,352 patients, followed by 25 to 29 years old. The number of deaths was as high as 32 from age 75 to 79, and the mortality rate was high at 14.22% between age 80 to 84. In the case of the region, the number of confirmed patients was the highest in Daegu with 6,454 patients, and the number of deaths was also high. At the lowest level of employee, the number of confirmed patients was the highest with 1,518, and the number of deaths was 26 among the population with Medicaid Service.
Table 1
General characteristics in the study population
|
Variables |
Confirmed group |
Mortality group |
CDR, % |
P value |
|
Total |
9,148 |
130 |
1.42 |
|
|
Sex |
|
|
|
|
|
|
Male |
3,556 |
67 |
1.88 |
0.003 |
|
|
Female |
5,592 |
63 |
1.13 |
|
|
Age group, yr |
|
|
|
|
|
0–4 |
46 |
|
|
< 0.001 |
|
5–9 |
57 |
|
|
|
|
10–14 |
126 |
|
|
|
|
15–19 |
353 |
|
|
|
|
20–24 |
1,352 |
|
|
|
|
25–29 |
1,126 |
|
|
|
|
30–34 |
457 |
|
|
|
|
35–39 |
485 |
1 |
0.21 |
|
|
40–44 |
498 |
1 |
0.20 |
|
|
45–49 |
739 |
|
|
|
|
50–54 |
906 |
3 |
0.33 |
|
|
55–59 |
819 |
7 |
0.85 |
|
|
60–64 |
710 |
9 |
1.27 |
|
|
65–69 |
445 |
10 |
2.25 |
|
|
70–74 |
318 |
9 |
2.83 |
|
|
75–79 |
296 |
32 |
10.81 |
|
|
80–84 |
204 |
29 |
14.22 |
|
|
≥ 85 |
211 |
29 |
13.74 |
|
|
Nationwide |
|
|
|
|
|
Seoul |
355 |
|
|
0.167 |
|
Busan |
112 |
2 |
1.79 |
|
|
Daegu |
6,454 |
93 |
1.44 |
|
|
Incheon |
39 |
|
|
|
|
Gwangju |
19 |
|
|
|
|
Daejeon |
30 |
|
|
|
|
Ulsan |
36 |
|
|
|
|
Sejong |
44 |
|
|
|
|
Gyeonggi |
399 |
4 |
1.00 |
|
|
Gangwon |
30 |
1 |
3.33 |
|
|
Chungbuk |
39 |
|
|
|
|
Chungnam |
124 |
|
|
|
|
Jeonbuk |
10 |
|
|
|
|
Jeonnam |
8 |
|
|
|
|
Gyeongbuk |
1,262 |
30 |
2.38 |
|
|
Gyeongnam |
90 |
|
|
|
|
Jeju |
6 |
|
|
|
|
Airport |
91 |
|
|
|
|
Health insurance premium level |
|
|
|
|
|
Medicaid |
727 |
26 |
3.58 |
< 0.001 |
|
Self-employed |
|
|
|
|
|
Lowest |
661 |
8 |
1.21 |
|
|
Low |
454 |
4 |
0.88 |
|
|
Middle |
469 |
7 |
1.49 |
|
|
High |
424 |
6 |
1.42 |
|
|
Highest |
392 |
12 |
3.06 |
|
|
Employee |
|
|
|
|
|
Lowest |
1,518 |
18 |
1.19 |
|
|
Low |
1,442 |
12 |
0.83 |
|
|
Middle |
1,189 |
13 |
1.09 |
|
|
High |
934 |
12 |
1.28 |
|
|
Highest |
938 |
12 |
1.28 |
|
Status of history of comorbidity
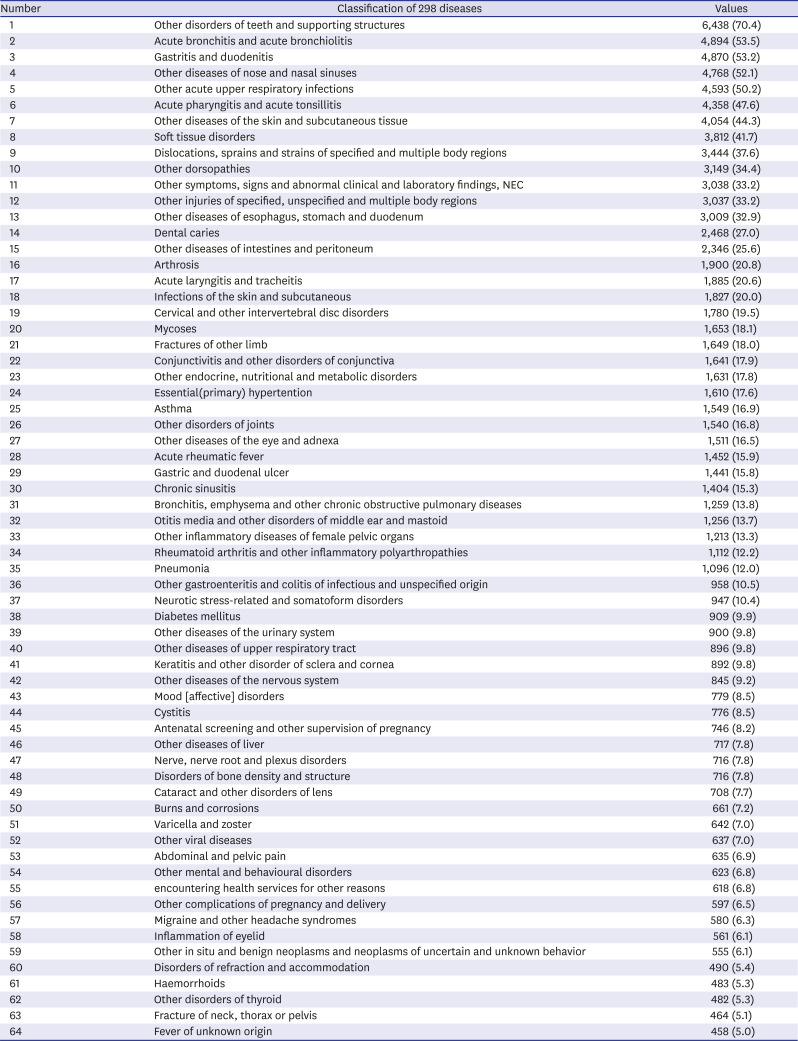
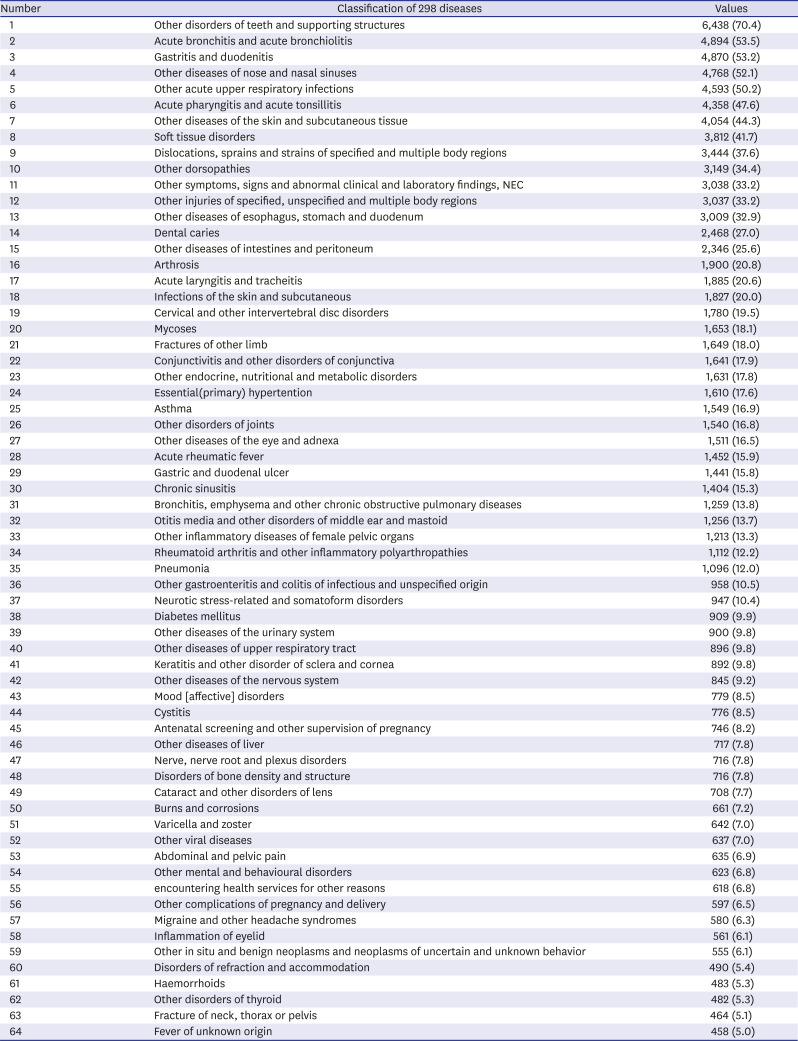
Looking at the history of comorbidities in patients with COVID-19, other disorders of the teeth and supporting structures were the highest at 70.4%, followed by acute bronchitis and acute bronchiolitis 53.5%, gastritis and duodenitis 53.2%, 52.1% of other nose and nasal sinuses, and 50.2% of other acute upper respiratory infections (
Table 2). Among comorbidities, in case of chronic disease, essential hypertension was 17.6%, asthma 16.9%, bronchitis, emphysema and other chronic obstructive pulmonary diseases 13.8%, rheumatoid arthritis and other inflammatory polyarthropathies were 12.2% and diabetes mellitus 9.9%.
Table 2
History of comorbiditiesa in the study population
|
Number |
Classification of 298 diseases |
Values |
|
1 |
Other disorders of teeth and supporting structures |
6,438 (70.4) |
|
2 |
Acute bronchitis and acute bronchiolitis |
4,894 (53.5) |
|
3 |
Gastritis and duodenitis |
4,870 (53.2) |
|
4 |
Other diseases of nose and nasal sinuses |
4,768 (52.1) |
|
5 |
Other acute upper respiratory infections |
4,593 (50.2) |
|
6 |
Acute pharyngitis and acute tonsillitis |
4,358 (47.6) |
|
7 |
Other diseases of the skin and subcutaneous tissue |
4,054 (44.3) |
|
8 |
Soft tissue disorders |
3,812 (41.7) |
|
9 |
Dislocations, sprains and strains of specified and multiple body regions |
3,444 (37.6) |
|
10 |
Other dorsopathies |
3,149 (34.4) |
|
11 |
Other symptoms, signs and abnormal clinical and laboratory findings, NEC |
3,038 (33.2) |
|
12 |
Other injuries of specified, unspecified and multiple body regions |
3,037 (33.2) |
|
13 |
Other diseases of esophagus, stomach and duodenum |
3,009 (32.9) |
|
14 |
Dental caries |
2,468 (27.0) |
|
15 |
Other diseases of intestines and peritoneum |
2,346 (25.6) |
|
16 |
Arthrosis |
1,900 (20.8) |
|
17 |
Acute laryngitis and tracheitis |
1,885 (20.6) |
|
18 |
Infections of the skin and subcutaneous |
1,827 (20.0) |
|
19 |
Cervical and other intervertebral disc disorders |
1,780 (19.5) |
|
20 |
Mycoses |
1,653 (18.1) |
|
21 |
Fractures of other limb |
1,649 (18.0) |
|
22 |
Conjunctivitis and other disorders of conjunctiva |
1,641 (17.9) |
|
23 |
Other endocrine, nutritional and metabolic disorders |
1,631 (17.8) |
|
24 |
Essential(primary) hypertention |
1,610 (17.6) |
|
25 |
Asthma |
1,549 (16.9) |
|
26 |
Other disorders of joints |
1,540 (16.8) |
|
27 |
Other diseases of the eye and adnexa |
1,511 (16.5) |
|
28 |
Acute rheumatic fever |
1,452 (15.9) |
|
29 |
Gastric and duodenal ulcer |
1,441 (15.8) |
|
30 |
Chronic sinusitis |
1,404 (15.3) |
|
31 |
Bronchitis, emphysema and other chronic obstructive pulmonary diseases |
1,259 (13.8) |
|
32 |
Otitis media and other disorders of middle ear and mastoid |
1,256 (13.7) |
|
33 |
Other inflammatory diseases of female pelvic organs |
1,213 (13.3) |
|
34 |
Rheumatoid arthritis and other inflammatory polyarthropathies |
1,112 (12.2) |
|
35 |
Pneumonia |
1,096 (12.0) |
|
36 |
Other gastroenteritis and colitis of infectious and unspecified origin |
958 (10.5) |
|
37 |
Neurotic stress-related and somatoform disorders |
947 (10.4) |
|
38 |
Diabetes mellitus |
909 (9.9) |
|
39 |
Other diseases of the urinary system |
900 (9.8) |
|
40 |
Other diseases of upper respiratory tract |
896 (9.8) |
|
41 |
Keratitis and other disorder of sclera and cornea |
892 (9.8) |
|
42 |
Other diseases of the nervous system |
845 (9.2) |
|
43 |
Mood [affective] disorders |
779 (8.5) |
|
44 |
Cystitis |
776 (8.5) |
|
45 |
Antenatal screening and other supervision of pregnancy |
746 (8.2) |
|
46 |
Other diseases of liver |
717 (7.8) |
|
47 |
Nerve, nerve root and plexus disorders |
716 (7.8) |
|
48 |
Disorders of bone density and structure |
716 (7.8) |
|
49 |
Cataract and other disorders of lens |
708 (7.7) |
|
50 |
Burns and corrosions |
661 (7.2) |
|
51 |
Varicella and zoster |
642 (7.0) |
|
52 |
Other viral diseases |
637 (7.0) |
|
53 |
Abdominal and pelvic pain |
635 (6.9) |
|
54 |
Other mental and behavioural disorders |
623 (6.8) |
|
55 |
encountering health services for other reasons |
618 (6.8) |
|
56 |
Other complications of pregnancy and delivery |
597 (6.5) |
|
57 |
Migraine and other headache syndromes |
580 (6.3) |
|
58 |
Inflammation of eyelid |
561 (6.1) |
|
59 |
Other in situ and benign neoplasms and neoplasms of uncertain and unknown behavior |
555 (6.1) |
|
60 |
Disorders of refraction and accommodation |
490 (5.4) |
|
61 |
Haemorrhoids |
483 (5.3) |
|
62 |
Other disorders of thyroid |
482 (5.3) |
|
63 |
Fracture of neck, thorax or pelvis |
464 (5.1) |
|
64 |
Fever of unknown origin |
458 (5.0) |
Epidemiological factors affecting the death of the study subjects
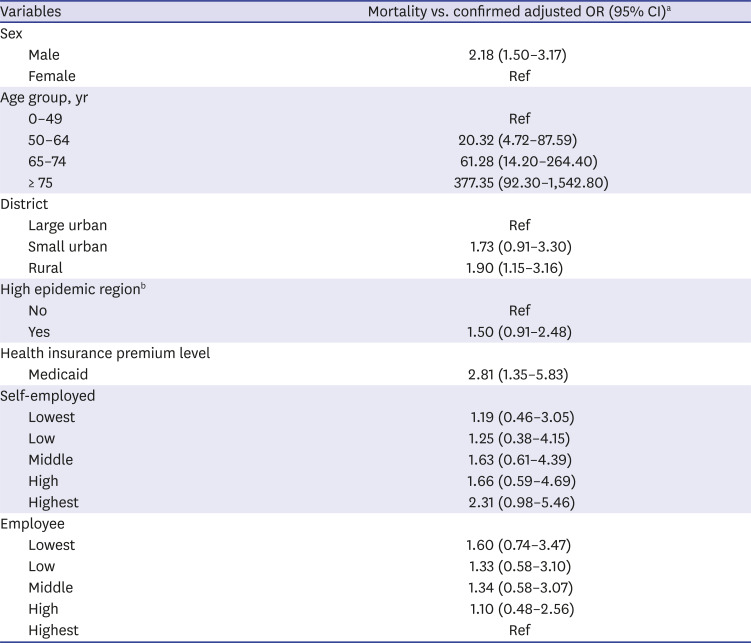
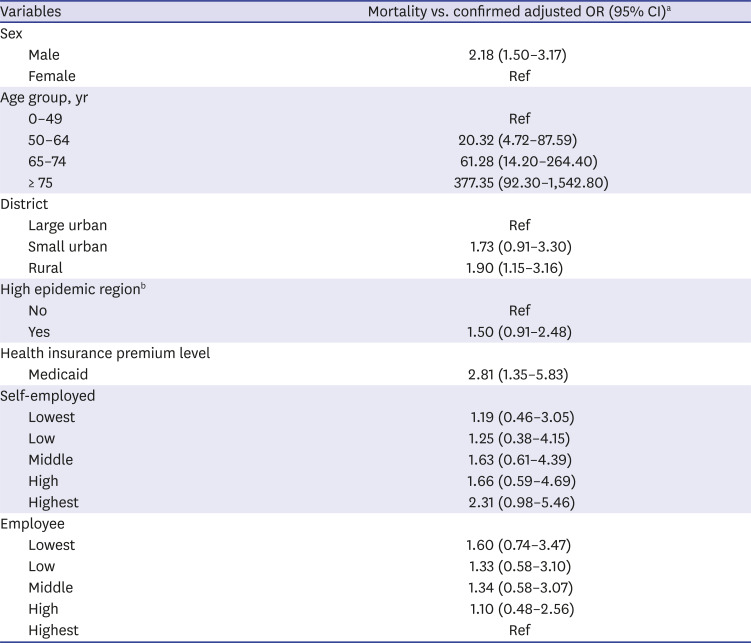
According to epidemiologic factors affecting death in patients with COVID-19, the odds ratio of death increased as age increased from age 0–49 (
Table 3). By the type region, the odds ratio of death was 1.73-fold (95% CI, 0.91–3.30) higher in small and medium-sized urban, 1.90-fold (95% CI, 1.15–3.16) higher in rural compared to large urban. In addition, the odds ratio of death was 1.50-fold (95% CI, 0.91–2.48) higher in the Daegu where massive outbreak occurred compared to the other regions, but was not statistically significant. By the income level reflecting the insurance type, odds ratio was found to be 2.81-fold higher (95% CI, 1.35–5.83) higher in patients with Medicaid Service than the employee with highest income level.
Table 3
Epidemiological factors affecting mortality in the study population
|
Variables |
Mortality vs. confirmed adjusted OR (95% CI)a
|
|
Sex |
|
|
Male |
2.18 (1.50–3.17) |
|
Female |
Ref |
|
Age group, yr |
|
|
0–49 |
Ref |
|
50–64 |
20.32 (4.72–87.59) |
|
65–74 |
61.28 (14.20–264.40) |
|
≥ 75 |
377.35 (92.30–1,542.80) |
|
District |
|
|
Large urban |
Ref |
|
Small urban |
1.73 (0.91–3.30) |
|
Rural |
1.90 (1.15–3.16) |
|
High epidemic regionb
|
|
|
No |
Ref |
|
Yes |
1.50 (0.91–2.48) |
|
Health insurance premium level |
|
|
Medicaid |
2.81 (1.35–5.83) |
|
Self-employed |
|
|
Lowest |
1.19 (0.46–3.05) |
|
Low |
1.25 (0.38–4.15) |
|
Middle |
1.63 (0.61–4.39) |
|
High |
1.66 (0.59–4.69) |
|
Highest |
2.31 (0.98–5.46) |
|
Employee |
|
|
Lowest |
1.60 (0.74–3.47) |
|
Low |
1.33 (0.58–3.10) |
|
Middle |
1.34 (0.58–3.07) |
|
High |
1.10 (0.48–2.56) |
|
Highest |
Ref |
Relationship between chronic disease and death
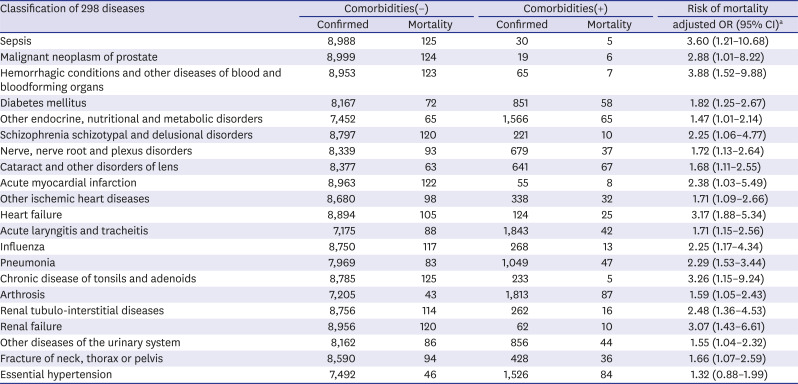
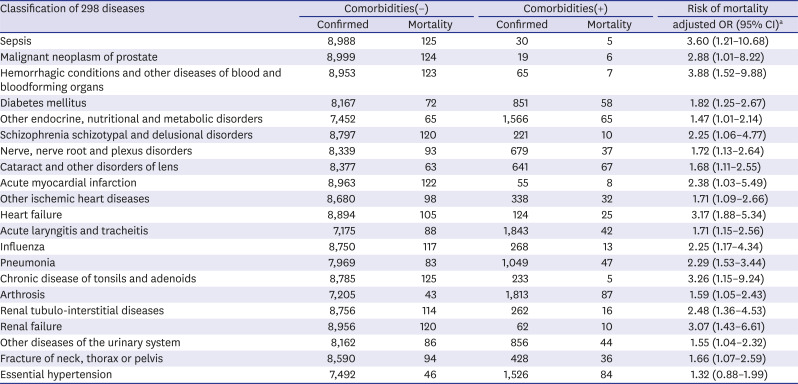
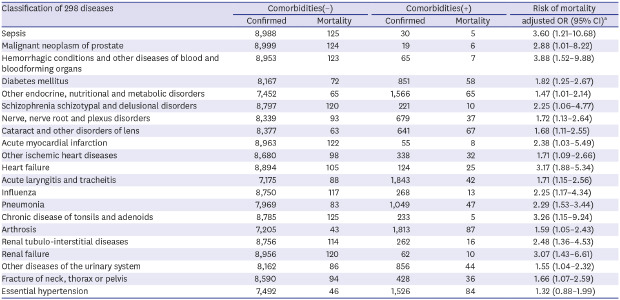
Adjusting the epidemiological factors and looking at the association between comorbidities and death, when patients with COVID-19 have comorbidity the odds ratio of death by sepsis was the highest with 3.60-fold (95% CI, 1.21–10.68), acute laryngitis and tracheitis were 1.71-fold (95% CI, 1.15–2.56), influenza was 2.25-fold (95% CI, 1.17–4.34), and pneumonia was 2.29-fold (95% CI, 1.53–3.44) (
Table 4). In the relationship between chronic comorbidities and death, the odds ratio of death with malignant neoplasm of prostate is 2.88-fold (95% CI, 1.01–8.22), hemorrhagic conditions and other diseases of the blood and blood-forming organs are 3.88-fold (95% CI, 1.52–9.88), diabetes mellitus 1.82-fold (95% CI, 1.25–2.67), acute myocardial infarction 2.38-fold (95% CI, 1.03–5.49), other ischemic heart disease 1.71-fold (95% CI, 1.09–2.66), heart failure was 3.17-fold (95% CI, 1.88–5.34), and renal failure was 3.07-fold (95% CI, 1.43–6.61).
Table 4
Risk of mortality in the study population by comorbidities
|
Classification of 298 diseases |
Comorbidities(−) |
Comorbidities(+) |
Risk of mortality |
|
Confirmed |
Mortality |
Confirmed |
Mortality |
adjusted OR (95% CI)a
|
|
Sepsis |
8,988 |
125 |
30 |
5 |
3.60 (1.21–10.68) |
|
Malignant neoplasm of prostate |
8,999 |
124 |
19 |
6 |
2.88 (1.01–8.22) |
|
Hemorrhagic conditions and other diseases of blood and bloodforming organs |
8,953 |
123 |
65 |
7 |
3.88 (1.52–9.88) |
|
Diabetes mellitus |
8,167 |
72 |
851 |
58 |
1.82 (1.25–2.67) |
|
Other endocrine, nutritional and metabolic disorders |
7,452 |
65 |
1,566 |
65 |
1.47 (1.01–2.14) |
|
Schizophrenia schizotypal and delusional disorders |
8,797 |
120 |
221 |
10 |
2.25 (1.06–4.77) |
|
Nerve, nerve root and plexus disorders |
8,339 |
93 |
679 |
37 |
1.72 (1.13–2.64) |
|
Cataract and other disorders of lens |
8,377 |
63 |
641 |
67 |
1.68 (1.11–2.55) |
|
Acute myocardial infarction |
8,963 |
122 |
55 |
8 |
2.38 (1.03–5.49) |
|
Other ischemic heart diseases |
8,680 |
98 |
338 |
32 |
1.71 (1.09–2.66) |
|
Heart failure |
8,894 |
105 |
124 |
25 |
3.17 (1.88–5.34) |
|
Acute laryngitis and tracheitis |
7,175 |
88 |
1,843 |
42 |
1.71 (1.15–2.56) |
|
Influenza |
8,750 |
117 |
268 |
13 |
2.25 (1.17–4.34) |
|
Pneumonia |
7,969 |
83 |
1,049 |
47 |
2.29 (1.53–3.44) |
|
Chronic disease of tonsils and adenoids |
8,785 |
125 |
233 |
5 |
3.26 (1.15–9.24) |
|
Arthrosis |
7,205 |
43 |
1,813 |
87 |
1.59 (1.05–2.43) |
|
Renal tubulo-interstitial diseases |
8,756 |
114 |
262 |
16 |
2.48 (1.36–4.53) |
|
Renal failure |
8,956 |
120 |
62 |
10 |
3.07 (1.43–6.61) |
|
Other diseases of the urinary system |
8,162 |
86 |
856 |
44 |
1.55 (1.04–2.32) |
|
Fracture of neck, thorax or pelvis |
8,590 |
94 |
428 |
36 |
1.66 (1.07–2.59) |
|
Essential hypertension |
7,492 |
46 |
1,526 |
84 |
1.32 (0.88–1.99) |
DISCUSSION
In the current state, it is possible to confirm the high mortality rate when aged over 65 classified as a high risk group and accompanying underlying diseases are accompanied.
1 Even though, 71.79% of patients with COVID-19 occurred in the Daegu region, the death rate was not significantly different compared to other regions. This may be related to Korea's preemptive intervention strategy of early diagnosis, tracking and action.
The main purpose of this study was to report the relationship between chronic comorbidities and death by correcting the epidemiological factors of patients with COVID-19 in Korea by linking the KNHIS's database with the registry data from the KCDC. According to the history of comorbidities, there include 17.6% of essential hypertension, 16.9% of asthma, 13.8% of bronchitis, emphysema and other chronic obstructive pulmonary diseases, 12.2% of rheumatoid arthritis and other inflammatory polyarthropathies, and 9.9% of diabetes. According to the results of multivariate logistic regression analysis adjusted by sex, age, type of distiricts, high epidemic region and socio-economic status, the odds ratio of dying with hemorrhagic conditions and other diseases of the blood and blood-forming organs was 3.88-fold (95% CI, 1.52–9.88), and heart failure was 3.17-fold (95% CI, 1.88–5.34), renal failure 3.07-fold (95% CI, 1.43–6.61), malignant neoplasm of prostate 2.88-fold (95% CI, 1.01–8.22), acute myocardial infarction 2.38-fold (95% CI, 1.03–5.49), diabetes mellitus was 1.82-fold (95% CI, 1.25–2.67), and other ischemic heart disease 1.71-fold (95% CI, 1.09–2.66). Even though, odds ratio of dying with essential hypertension was 1.32-fold, but was not statistically significant (95% CI, 0.88–1.99) in this nationwide study.
In the Yang et al.
7 study, a systematic literature review and meta-analysis of the prevalence of comorbidities in patients with COVID-19, the prevalence of comorbidities was evaluated to be high in hypertension and diabetes, and it was suggested that underlying diseases such as hypertension, respiratory disease, and cardiovascular disease could be risk factors for severe patients. Also Rodriguez-Morales et al.
8 systematic literature review and meta-analysis study showed that the prevalence of comorbidities in patients confirmed with COVID-19 was 36.8%, especially the highest in hypertension, followed by cardiovascular disease and diabetes. It was concluded that infection with COVID-19 was associated with serious morbidity, especially in patients with chronic disease. Arentz et al.
9 study found that 21 patients admitted to the intensive care unit accounted for 47.6% of chronic kidney disease, 42.9% of congestive heart failure, 33.3% of chronic obstructive pulmonary disease and diabetes among comorbidities. The results of the study are also consistent with prior studies in diabetes, heart diseases, respiratory diseases and kidney diseases. Hypertension also was a common comorbidity, but this was not a significant risk factor for death by adjusting critical epidemiologic factors like sex, age and income level. High mortality in older population seems due to physiological changes that come with ageing and potential underlying comorbidities, like malignant neoplasm, diabetes, heart disease, and so forth. The study also observed an increase in statistically significant odds ratio in the major disease groups common in older people.
Chronic patients are at degraded immunity function state due to underlying disease. Since patients with chronic diseases have increased sensitivity to COVID-19 infection, they are at higher risk for complications such as deterioration of underlying diseases, pneumonia, failure of other organs and sepsis, etc.; as a result, their chronic diseases may become severe, or the patients may die. These results suggest that comorbidities may be risk factors of death for patients exposed to the virus of COVID-19.
7
COVID-19 is infected by exposure to the virus in various ways by the propagation route, but in the exposed environment, precedent chronic diseases are susceptible to infection by COVID-19, increasing morbidity, which is considered to be a high-risk recipient, so intensive care is necessary.
10
The limitation of this study was that we used the diagnosis information in the KNHIS's claim data. The validity of the claimed diagnosis is a very traditional issue. However, we tried to overcome some of limitations by applying certain criteria like hospitalization for more than three days, or outpatient visits for more than four days, or prescriptions for medicines for more than 28 days annually. And, it is likely that the registration and evaluation system of KNHIS and Health Insurance Review and Assessment Service implemented over the past two decades in chronic and high cost diseases has affected the validity of the data.
This study analyzed the registry data of confirmed patients in connection with the NHIS's database. Among the chronic comorbidities, Hemorrhagic conditions and other diseases of the blood and blood-forming organs, heart failure, renal failure, malignant neoplasm of the prostate, acute myocardial infarction, diabetes, and, other ischemic heart diseases showed significant correlation with high mortality. We expect that the results of this study could we hope that this study could provide information on high risk groups for preemptive interventions to prevent progression to severe conditions and death. In the future, if a vaccine for COVID-19 is developed, it is expected that this study could be the basic data for recommending immunization by selecting those with chronic disease that had high risk of death, as recommended target diseases for vaccination. Lastly, it is necessary to study the effect of clinical interventions to prevent severe status or death with considerations of comorbidities in COVID-19 patients. In Korea, such research is also expected to be possible in the near future, depending on the accumulation of clinical information.
ACKNOWLEDGMENTS
We thank all of the people who are struggling in healthcare fields to overcome the COVID-19 outbreak. In addition, we would like to thank epidemiological team of the Centers for Disease Control and Prevention, for providing registry data for the study. This study was performed under the research project named ‘Research and Development on Integrated Surveillance System for Early Warning of Infectious Diseases (RISEWIDs)’. The investigators of this project were Jaiyong Kim (Yonsei University), Sunworl Kim (National Medical Center), Eui Jung Kwon (National Health Insurance Review and Assessment Service), Dong Wook Kim (National Health Insurance Service), Moran Ki (National Cancer Center), Hyunjin Son (Pusan National University Hospital), Jong-Hun Kim (Sungkyunkwan University), Jin Yong Kim(Incheon Medical Center), Heeyoung Lee (Seoul National University Bundang Hospital), Boyoung Park (Hanyang University), Woo-Sik Son (National Institute for Mathematical Sciences), Jungsoon Choi (Hanyang University), Sunhwa Choi (National Cancer Center), Okyu Kwon (National Institute for Mathematical Sciences), Hyojung Lee (National Institute for Mathematical Sciences), Jong-Hoon Kim (International Vaccine Institute), Heecheon Kim (MISO INFO TECH), and Bo Youl Choi (Hanyang University).
References
2. Baek JH, Seo YB, Choi WS, Kee SY, Jeong HW, Lee HY, et al. Guideline on the prevention and control of seasonal influenza in healthcare setting. Korean J Intern Med. 2014; 29(2):265–280. PMID:
24648817.

3. Wan S, Xiang Y, Fang W, Zheng Y, Li B, Hu Y, et al. Clinical features and treatment of COVID-19 patients in northeast Chongqing. J Med Virol. 2020; 92(7):797–806. PMID:
32198776.

4. Chen J, Qi T, Liu L, Ling Y, Qian Z, Li T, et al. Clinical progression of patients with COVID-19 in Shanghai, China. J Infect. 2020; 80(5):e1–6.

7. Yang J, Zheng Y, Gou X, Pu K, Chen Z, Guo Q, et al. Prevalence of comorbidities in the novel Wuhan coronavirus (COVID-19) infection: a systematic review and meta-analysis. Int J Infect Dis. Forthcoming. 2020; DOI:
10.1016/j.ijid.2020.03.017.
8. Rodriguez-Morales AJ, Cardona-Ospina JA, Gutiérrez-Ocampo E, Villamizar-Peña R, Holguin-Rivera Y, Escalera-Antezana JP, et al. Clinical, laboratory and imaging features of COVID-19: a systematic review and meta-analysis. Travel Med Infect Dis. 2020; 34:101623. PMID:
32179124.

9. Arentz M, Yim E, Klaff L, Lokhandwala S, Riedo FX, Chong M, et al. Characteristics and outcomes of 21 critically ill patients with COVID-19 in Washington State. JAMA. 2020; 323(16):1612.

10. Wang Z, Yang B, Li Q, Wen L, Zhang R. Clinical features of 69 cases with coronavirus disease 2019 in Wuhan, China. Clin Infect Dis. Forthcoming. 2020; DOI:
10.1093/cid/ciaa272.





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download