1. Hsiao PY, Tien HC, Lo CP, Juang JM, Wang YH, Sung RJ. Gene mutations in cardiac arrhythmias: a review of recent evidence in ion channelopathies. Appl Clin Genet. 2013; 6:1–13. PMID:
23837003.
2. Wilde AA, Bezzina CR. Genetics of cardiac arrhythmias. Heart. 2005; 91(10):1352–1358. PMID:
16162633.

3. Chen PS, Garfinkel A, Weiss JN, Karagueuzian HS. CHEN PS. Garfinkel A, Weiss JN, Karagueuzian HS. Spirals, chaos, and new mechanisms of wave propagation. Pacing Clin Electrophysiol. 1997; 20(2):414–421. PMID:
9058845.
4. Kannel WB, Benjamin EJ. Status of the epidemiology of atrial fibrillation. Med Clin North Am. 2008; 92(1):17–40. PMID:
18060995.

5. Stewart S, Hart CL, Hole DJ, McMurray JJ. A population-based study of the long-term risks associated with atrial fibrillation: 20-year follow-up of the Renfrew/Paisley study. Am J Med. 2002; 113(5):359–364. PMID:
12401529.

6. Brugada R, Hong K, Dumaine R, Cordeiro J, Gaita F, Borggrefe M, et al. Sudden death associated with short-QT syndrome linked to mutations in HERG. Circulation. 2004; 109(1):30–35. PMID:
14676148.

7. Gussak I, Brugada P, Brugada J, Wright RS, Kopecky SL, Chaitman BR, et al. Idiopathic short QT interval: a new clinical syndrome? Cardiology. 2000; 94(2):99–102. PMID:
11173780.
8. Giustetto C, Di Monte F, Wolpert C, Borggrefe M, Schimpf R, Sbragia P, et al. Short QT syndrome: clinical findings and diagnostic-therapeutic implications. Eur Heart J. 2006; 27(20):2440–2447. PMID:
16926178.

9. Hong K, Bjerregaard P, Gussak I, Brugada R. Short QT syndrome and atrial fibrillation caused by mutation in KCNH2. J Cardiovasc Electrophysiol. 2005; 16(4):394–396. PMID:
15828882.

10. Zhang YH, Colenso CK, Sessions RB, Dempsey CE, Hancox JC. The hERG K(+) channel S4 domain L532P mutation: characterization at 37°C. Biochim Biophys Acta. 2011; 1808(10):2477–2487. PMID:
21777565.

11. Sanguinetti MC, Jiang C, Curran ME, Keating MT. A mechanistic link between an inherited and an acquired cardiac arrhythmia: HERG encodes the IKr potassium channel. Cell. 1995; 81(2):299–307. PMID:
7736582.
12. Trudeau MC, Warmke JW, Ganetzky B, Robertson GA. HERG, a human inward rectifier in the voltage-gated potassium channel family. Science. 1995; 269(5220):92–95. PMID:
7604285.

13. Hassel D, Scholz EP, Trano N, Friedrich O, Just S, Meder B, et al. CLINICAL PERSPECTIVE. Circulation. 2008; 117(7):866–875. PMID:
18250272.
14. Vandenberg JI, Walker BD, Campbell TJ. HERG K+ channels: friend and foe. Trends Pharmacol Sci. 2001; 22(5):240–246. PMID:
11339975.

15. Adeniran I, El Harchi A, Hancox JC, Zhang H. Proarrhythmia in KCNJ2-linked short QT syndrome: insights from modelling. Cardiovasc Res. 2012; 94(1):66–76. PMID:
22308236.

16. Imaniastuti R, Lee HS, Kim N, Youm JB, Shim EB, Lim KM. Computational prediction of proarrhythmogenic effect of the V241F KCNQ1 mutation in human atrium. Prog Biophys Mol Biol. 2014; 116(1):70–75. PMID:
25230101.

17. Zulfa I, Shim EB, Song KS, Lim KM. Computational simulations of the effects of the G229D KCNQ1 mutation on human atrial fibrillation. J Physiol Sci. 2016; 66(5):407–415. PMID:
26922794.

18. Hodgkin AL, Huxley AF. A quantitative description of membrane current and its application to conduction and excitation in nerve. J Physiol. 1952; 117(4):500–544. PMID:
12991237.

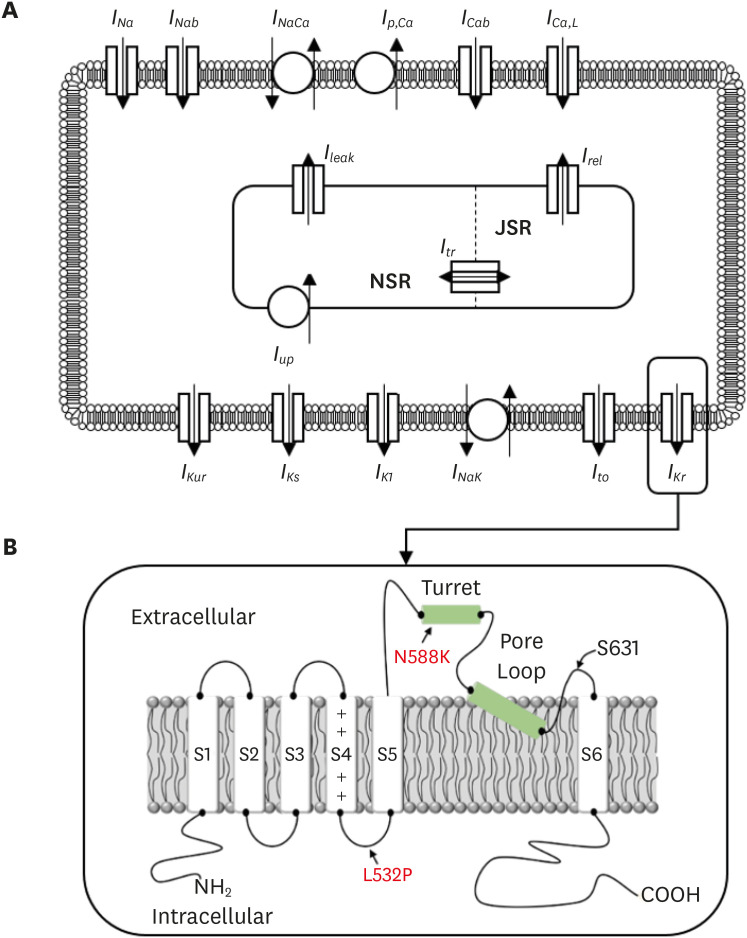
19. Courtemanche M, Ramirez RJ, Nattel S. Ionic mechanisms underlying human atrial action potential properties: insights from a mathematical model. Am J Physiol. 1998; 275(1):H301–21. PMID:
9688927.

20. Jacquemet V, Virag N, Ihara Z, Dang L, Blanc O, Zozor S, et al. Study of unipolar electrogram morphology in a computer model of atrial fibrillation. J Cardiovasc Electrophysiol. 2003; 14(10 Suppl):S172–S179. PMID:
14760921.

21. McPate MJ, Duncan RS, Milnes JT, Witchel HJ, Hancox JC. The N588K-HERG K+ channel mutation in the ‘short QT syndrome’: mechanism of gain-in-function determined at 37 degrees C. Biochem Biophys Res Commun. 2005; 334(2):441–449. PMID:
16011830.
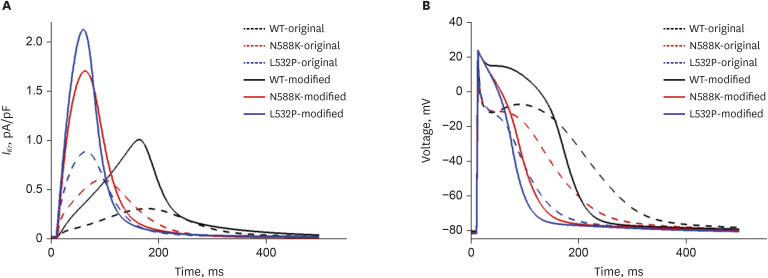
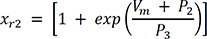
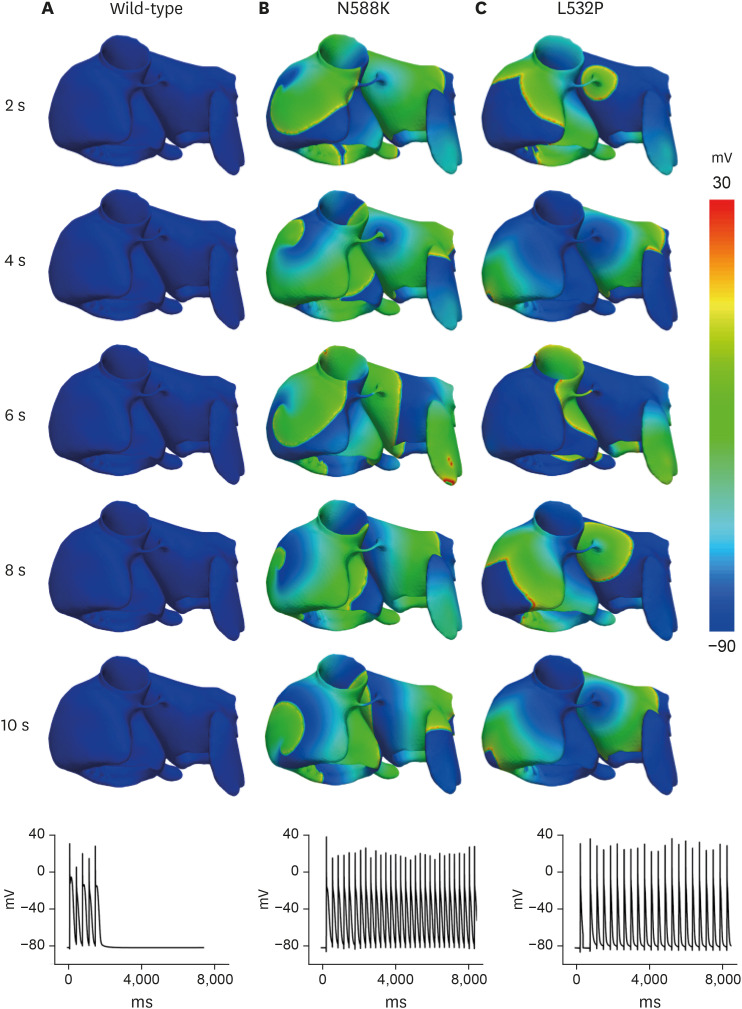
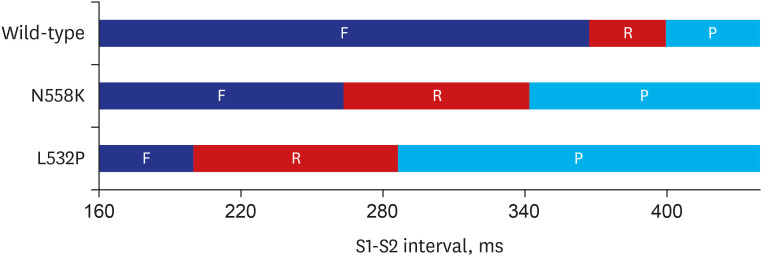
22. Loewe A, Wilhelms M, Fischer F, Scholz EP, Dössel O, Seemann G. Arrhythmic potency of human ether-a-go-go-related gene mutations L532P and N588K in a computational model of human atrial myocytes. Europace. 2014; 16(3):435–443. PMID:
24569898.
23. Hwang M, Kwon SS, Wi J, Park M, Lee HS, Park JS, et al. Virtual ablation for atrial fibrillation in personalized in-silico three-dimensional left atrial modeling: comparison with clinical catheter ablation. Prog Biophys Mol Biol. 2014; 116(1):40–47. PMID:
25261813.

24. Xie F, Qu Z, Yang J, Baher A, Weiss JN, Garfinkel A. A simulation study of the effects of cardiac anatomy in ventricular fibrillation. J Clin Invest. 2004; 113(5):686–693. PMID:
14991066.

25. Jeong DU, Lim KM. Influence of the KCNQ1 S140G mutation on human ventricular arrhythmogenesis and pumping performance: simulation study. Front Physiol. 2018; 9:926. PMID:
30108508.

26. Adeniran I, Hancox JC, Zhang H. In silico investigation of the short QT syndrome, using human ventricle models incorporating electromechanical coupling. Front Physiol. 2013; 4:166. PMID:
23847545.

27. Kamiya K, Mitcheson JS, Yasui K, Kodama I, Sanguinetti MC. Open channel block of HERG K(+) channels by vesnarinone. Mol Pharmacol. 2001; 60(2):244–253. PMID:
11455010.

28. Volberg WA, Koci BJ, Su W, Lin J, Zhou J. Blockade of human cardiac potassium channel human ether-a-go-go-related gene (HERG) by macrolide antibiotics. J Pharmacol Exp Ther. 2002; 302(1):320–327. PMID:
12065733.

29. Dumaine R, Roy ML, Brown AM. Blockade of HERG and Kv1.5 by ketoconazole. J Pharmacol Exp Ther. 1998; 286(2):727–735. PMID:
9694927.
30. Roy M, Dumaine R, Brown AM. HERG, a primary human ventricular target of the nonsedating antihistamine terfenadine. Circulation. 1996; 94(4):817–823. PMID:
8772706.

31. Heikhmakhtiar AK, Rasyidin FA, Lim KM. V241F KCNQ1 mutation shortens electrical wavelength and reduces ventricular pumping capabilities: a simulation study with an electro-mechanical model. Front Phys. 2018; 6:147.

32. Yuniarti AR, Setianto F, Marcellinus A, Hwang HJ, Choi SW, Trayanova N, et al. Effect of KCNQ1 G229D mutation on cardiac pumping efficacy and reentrant dynamics in ventricles: computational study. Int J Numer Methods Biomed Eng. 2018; 34(6):e2970.

33. Heikhmakhtiar AK, Lee CH, Song KS, Lim KM. Computational prediction of the effect of D172N KCNJ2 mutation on ventricular pumping during sinus rhythm and reentry. Med Biol Eng Comput. 2020; 58(5):977–990. PMID:
32095980.

34. Tamargo J, Caballero R, Gómez R, Valenzuela C, Delpón E. Pharmacology of cardiac potassium channels. Cardiovasc Res. 2004; 62(1):9–33. PMID:
15023549.





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download