This article has been
cited by other articles in ScienceCentral.
Abstract
Coronavirus disease 2019 (COVID-19) has resulted in an ongoing pandemic; however, the socioeconomic burden of COVID-19 treatment in the pediatric population remains unclear. Thus, the aim of this study was to determine the hospitalization periods and medical costs among children with COVID-19. In total, 145 billing statements for pediatric patients receiving healthcare services because of COVID-19 from February 1, 2020 to March 31, 2020 were used. The study showed that individual treatment costs for children with COVID-19 are approximately USD 2,192 under the Korean National Health Insurance Service System. This study revealed the differences in cost among age groups, determined by the type of hospital wherein admission occurred, as a trend of increasing age, increasing hospitalization time, and increasing cost was observed. Tailored COVID-19 treatment strategies by age group may lower costs and increase the effectiveness of resource allocation.
Go to :

Graphical Abstract
Go to :

Keywords: Coronavirus disease, Severe Acute Respiratory Syndrome Coronavirus 2, Costs and Cost Analysis, Insurance, Pediatrics
Coronavirus disease 2019 (COVID-19) was first identified in December 2019 in Wuhan, China and has since spread globally, resulting in the ongoing pandemic. The first confirmed case of pediatric COVID-19 in Korea was reported on February 18, 2020, when the total number of confirmed cases had increased to 53 since the first reported case in Korea on January 20, 2020.
1 As of May 5, the total number of confirmed cases is 10,804, of which 9,283 patients have been discharged from isolation facilities. Of these, 731 (6.77%) patients are aged < 20 years. No death has been reported among children and adolescents thus far.
2
The governance of the healthcare system in Korea, also known as the Health Security System, has two components: mandatory social health insurance and medical aid. The National Health Insurance Service (NHIS) is available to approximately 98% of the population. The Ministry of Health and Welfare (MOHW) supervises the NHIS program by developing and implementing policies. The Health Insurance Review and Assessment Service (HIRA) evaluates the medical service fee, quality of healthcare, and adequacy of medical services.
3 As part of the policy for easing the financial treatment burden, COVID-19 patients in Korea have been receiving additional support. The co-payment was borne by the central and local governments with disaster relief payments under the Infectious Disease Control and Prevention Act, thereby obliterating patient burden.
4
HIRA databases contain all data from the NHIS and are accessible to healthcare professionals for research purposes. The MOHW initiated the #OpenData4Covid19 project on March 26, wherein researchers can request statistical data from the HIRA for research studies.
5 This project provides a closed dataset composed for global research collaboration, updated irregularly. Data for patients whose treatment has not been completed are also included.
The socioeconomic burden of COVID-19 treatment in the pediatric population remains unclear. The aim of this study was to determine the hospitalization periods and medical costs among children with COVID-19, which would facilitate the development of future policies.
Herein, 145 billing statements for pediatric patients receiving healthcare services because of COVID-19 from February 1, 2020 to March 31, 2020 were obtained from the HIRA, and the demographic data of the patients were recorded. The exchange rates for KRW to USD were presented in this report in March 2020 (1,000 KRW = 0.8194 USD).
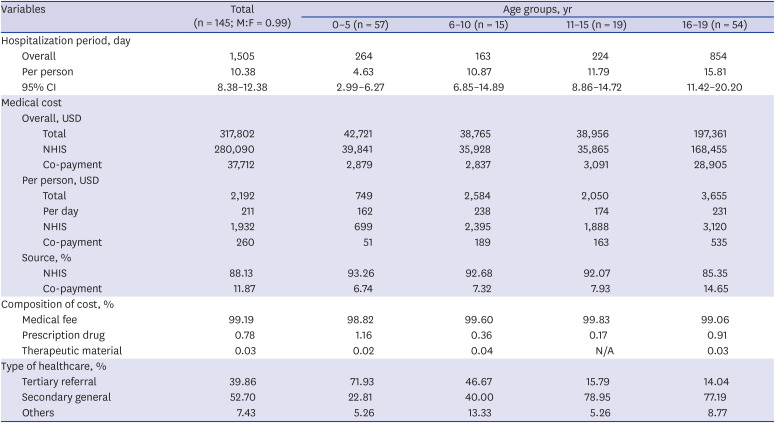
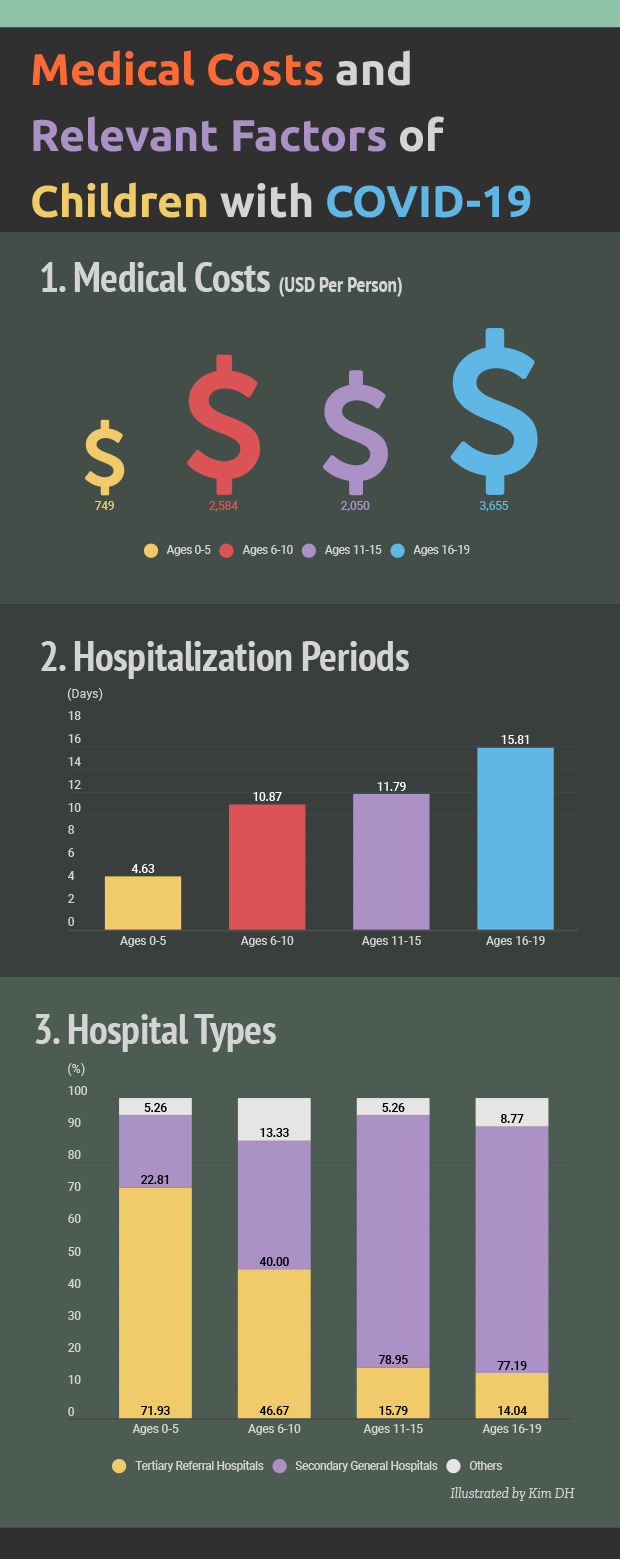
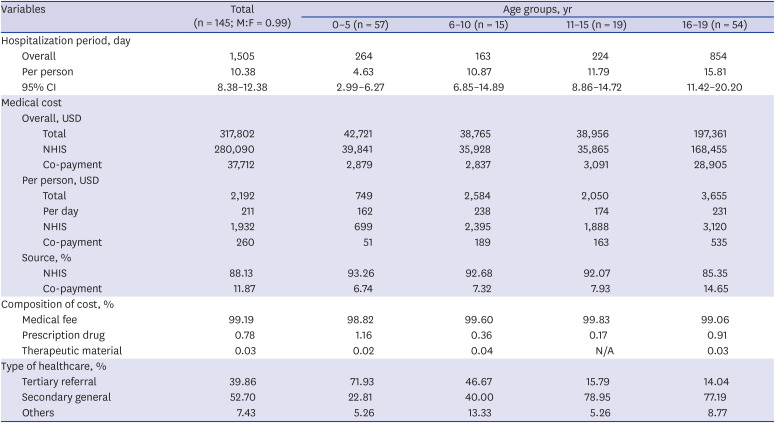
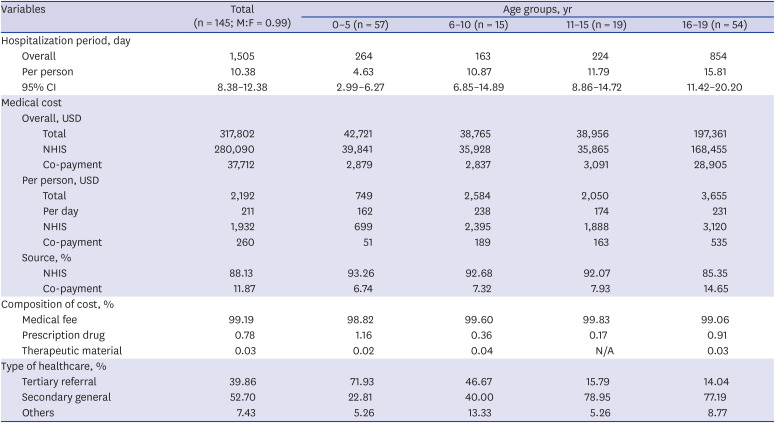
Demographic data, hospitalization periods, and medical costs among pediatric COVID-19 cases are summarized in
Table 1. The mean hospitalization period for 145 confirmed COVID-19 patients was 10.38 days, tending to increase with patient age: 0–5 years, 4.63 days; 6–10 years, 10.87 days; 11–15 years, 14.88 days; and 16–19 years, 15.81 days. Two negative tests are required for home discharge
3; thus, the mean hospitalization period is indicative of the viral shedding period. Therefore, contrary to current reports indicating that young infants and toddlers tend to have extended periods of viral shedding,
6 our results suggest that, given the longer hospitalization period as ages increases, extended shedding may be a unique aspect of COVID-19 in young adults or adolescents.
7 Although prolonged hospitalization period does not necessarily indicate a severe COVID-19 clinical course, further studies are required to elucidate its significance in providing effective medical resources based on age group.
Table 1
Hospitalization period and medical cost by age group in the management of pediatric coronavirus disease 2019 patients
|
Variables |
Total (n = 145; M:F = 0.99) |
Age groups, yr |
|
0–5 (n = 57) |
6–10 (n = 15) |
11–15 (n = 19) |
16–19 (n = 54) |
|
Hospitalization period, day |
|
|
|
|
|
|
Overall |
1,505 |
264 |
163 |
224 |
854 |
|
Per person |
10.38 |
4.63 |
10.87 |
11.79 |
15.81 |
|
95% CI |
8.38–12.38 |
2.99–6.27 |
6.85–14.89 |
8.86–14.72 |
11.42–20.20 |
|
Medical cost |
|
|
|
|
|
|
Overall, USD |
|
|
|
|
|
|
|
Total |
317,802 |
42,721 |
38,765 |
38,956 |
197,361 |
|
|
NHIS |
280,090 |
39,841 |
35,928 |
35,865 |
168,455 |
|
|
Co-payment |
37,712 |
2,879 |
2,837 |
3,091 |
28,905 |
|
Per person, USD |
|
|
|
|
|
|
|
Total |
2,192 |
749 |
2,584 |
2,050 |
3,655 |
|
|
Per day |
211 |
162 |
238 |
174 |
231 |
|
|
NHIS |
1,932 |
699 |
2,395 |
1,888 |
3,120 |
|
|
Co-payment |
260 |
51 |
189 |
163 |
535 |
|
Source, % |
|
|
|
|
|
|
|
NHIS |
88.13 |
93.26 |
92.68 |
92.07 |
85.35 |
|
|
Co-payment |
11.87 |
6.74 |
7.32 |
7.93 |
14.65 |
|
Composition of cost, % |
|
|
|
|
|
|
Medical fee |
99.19 |
98.82 |
99.60 |
99.83 |
99.06 |
|
Prescription drug |
0.78 |
1.16 |
0.36 |
0.17 |
0.91 |
|
Therapeutic material |
0.03 |
0.02 |
0.04 |
N/A |
0.03 |
|
Type of healthcare, % |
|
|
|
|
|
|
Tertiary referral |
39.86 |
71.93 |
46.67 |
15.79 |
14.04 |
|
Secondary general |
52.70 |
22.81 |
40.00 |
78.95 |
77.19 |
|
Others |
7.43 |
5.26 |
13.33 |
5.26 |
8.77 |

The total medical cost among 145 children in Korea was USD 317,802 (KRW 387,763,170), with USD 280,090 (KRW 341,748,770), i.e., 88.13%, of the total medical cost being borne by the NHIS. The mean individual medical cost was USD 2,192 (KRW 2,674,229); the mean individual medical cost for 16–19-year-old patients was USD 3,655 (KRW 4,459,403), with approximately USD 3,916 (KRW 4,780,000) being estimated through cost simulation for adult patients with mild-to-moderate COVID-19, according to the NHIS.
8 The proportion of medical fee was very high among children with COVID-19, accounting for approximately 99.19% of the total medical cost.
In general, medical costs increased with patient age. However, mean medical costs were lower for patients aged 11–15 years than for those aged 6–10 years, potentially because more patients aged 6–10 years were admitted to upper-level hospitals than those aged 11–15 years. Furthermore, considering the list of medications for each age group, patients aged 11–15 years needed the fewest medications in terms of both variety and quantity. The type of hospital and medical products obtained by the caregivers of the patients, such as cough and cold medications, might have influenced these findings.
This study has the following limitations. Our knowledge was limited to the dataset provided by the research system. Specifically, the medical fee, which accounted for most of the medical cost, included various components. However, we were not able to scrutinize each item of the medical fee. Second, as the dataset includes information for both patients whose treatment had ended and those still being treated with irregular updates, the results of this study should not be assumed as final. Despite these limitations, as this study is one of the first to report the financial burden of children with COVID-19 based on a reliable dataset, we believe that it will provide a useful basis for availing medical resources in response to COVID-19. Further studies are needed to consider factors including, but not limited to, disease severity, clinician specialty, prescription drugs, and expenditure on therapeutic materials.
Previous studies have reported that cases of pediatric COVID-19 might be less severe than those of adults and that the spectrum of COVID-19 symptoms is wider among children than among adults.
9 Although limited in predicting the hospital needs of children and adolescents with COVID-19, differences in hospitalization periods and the financial burden by age group were observed herein. The present result suggests that the requirement and utilization of medical services may vary depending on the age group.
This study provides an estimation of the financial burden of children with COVID-19. Despite the current results not being comparable with other reports because of limited data, the current findings are applicable in allocating limited medical resources and establishing effective policies for further emerging surges of COVID-19.
Ethics Statement
This study was exempted from review by the Institutional Review Board of Inha University Hospital (IUH-IRB-2020-04-018).
Go to :