1. Altkorn D, Vokes T. Treatment of postmenopausal osteoporosis. JAMA. 2001; 285(11):1415–1418. PMID:
11255400.

2. Levinson W, Altkorn D. Primary prevention of postmenopausal osteoporosis. JAMA. 1998; 280(21):1821–1822. PMID:
9846765.

3. Cappola AR, Shoback DM. Osteoporosis therapy in postmenopausal women with high risk of fracture. JAMA. 2016; 316(7):715–716. PMID:
27533154.

4. Siris ES, Miller PD, Barrett-Connor E, Faulkner KG, Wehren LE, Abbott TA, et al. Identification and fracture outcomes of undiagnosed low bone mineral density in postmenopausal women: results from the National Osteoporosis Risk Assessment. JAMA. 2001; 286(22):2815–2822. PMID:
11735756.

5. Pfister AK, Trotter CC. Bisphosphonate use and femoral fractures in older women. JAMA. 2011; 305(20):2068–2069.

6. Sellmeyer DE. Atypical fractures as a potential complication of long-term bisphosphonate therapy. JAMA. 2010; 304(13):1480–1484. PMID:
20924014.

7. Park-Wyllie LY, Mamdani MM, Juurlink DN, Hawker GA, Gunraj N, Austin PC, et al. Bisphosphonate use and the risk of subtrochanteric or femoral shaft fractures in older women. JAMA. 2011; 305(8):783–789. PMID:
21343577.

8. Wang Z, Bhattacharyya T. Trends in incidence of subtrochanteric fragility fractures and bisphosphonate use among the US elderly, 1996–2007. J Bone Miner Res. 2011; 26(3):553–560. PMID:
20814954.

9. Lee YK, Ha YC, Park C, Yoo JJ, Shin CS, Koo KH. Bisphosphonate use and increased incidence of subtrochanteric fracture in South Korea: results from the National Claim Registry. Osteoporos Int. 2013; 24(2):707–711. PMID:
22618268.

10. Shane E, Burr D, Abrahamsen B, Adler RA, Brown TD, Cheung AM, et al. Atypical subtrochanteric and diaphyseal femoral fractures: second report of a task force of the American Society for Bone and Mineral Research. J Bone Miner Res. 2014; 29(1):1–23. PMID:
23712442.

11. Gustafsson A, Schilcher J, Grassi L, Aspenberg P, Isaksson H. Strains caused by daily loading might be responsible for delayed healing of an incomplete atypical femoral fracture. Bone. 2016; 88:125–130. PMID:
27113528.

12. Teo BJ, Koh JS, Goh SK, Png MA, Chua DT, Howe TS. Post-operative outcomes of atypical femoral subtrochanteric fracture in patients on bisphosphonate therapy. Bone Joint J. 2014; 96-B(5):658–664. PMID:
24788502.

13. Egol KA, Park JH, Rosenberg ZS, Peck V, Tejwani NC. Healing delayed but generally reliable after bisphosphonate-associated complete femur fractures treated with IM nails. Clin Orthop Relat Res. 2014; 472(9):2728–2734. PMID:
23604648.

14. Prasarn ML, Ahn J, Helfet DL, Lane JM, Lorich DG. Bisphosphonate-associated femur fractures have high complication rates with operative fixation. Clin Orthop Relat Res. 2012; 470(8):2295–2301. PMID:
22669553.

15. Schilcher J. High revision rate but good healing capacity of atypical femoral fractures. A comparison with common shaft fractures. Injury. 2015; 46(12):2468–2473. PMID:
26477344.

16. Bogdan Y, Tornetta P 3rd, Einhorn TA, Guy P, Leveille L, Robinson J, et al. Healing time and complications in operatively treated atypical femur fractures associated with bisphosphonate use: a multicenter retrospective cohort. J Orthop Trauma. 2016; 30(4):177–181. PMID:
26709814.
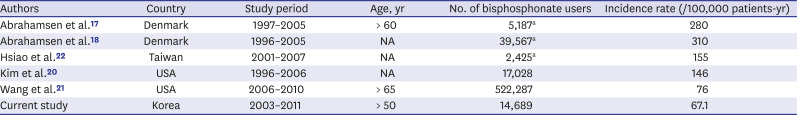
17. Abrahamsen B, Eiken P, Eastell R. Subtrochanteric and diaphyseal femur fractures in patients treated with alendronate: a register-based national cohort study. J Bone Miner Res. 2009; 24(6):1095–1102. PMID:
19113931.

18. Abrahamsen B, Eiken P, Eastell R. Cumulative alendronate dose and the long-term absolute risk of subtrochanteric and diaphyseal femur fractures: a register-based national cohort analysis. J Clin Endocrinol Metab. 2010; 95(12):5258–5265. PMID:
20843943.

19. Vestergaard P, Schwartz F, Rejnmark L, Mosekilde L. Risk of femoral shaft and subtrochanteric fractures among users of bisphosphonates and raloxifene. Osteoporos Int. 2011; 22(3):993–1001. PMID:
21165600.

20. Kim SY, Schneeweiss S, Katz JN, Levin R, Solomon DH. Oral bisphosphonates and risk of subtrochanteric or diaphyseal femur fractures in a population-based cohort. J Bone Miner Res. 2011; 26(5):993–1001. PMID:
21542002.

21. Wang Z, Ward MM, Chan L, Bhattacharyya T. Adherence to oral bisphosphonates and the risk of subtrochanteric and femoral shaft fractures among female medicare beneficiaries. Osteoporos Int. 2014; 25(8):2109–2116. PMID:
24846316.

22. Hsiao FY, Huang WF, Chen YM, Wen YW, Kao YH, Chen LK, et al. Hip and subtrochanteric or diaphyseal femoral fractures in alendronate users: a 10-year, nationwide retrospective cohort study in Taiwanese women. Clin Ther. 2011; 33(11):1659–1667. PMID:
22018450.

23. Ha YC, Kim TY, Lee A, Lee YK, Kim HY, Kim JH, et al. Current trends and future projections of hip fracture in South Korea using nationwide claims data. Osteoporos Int. 2016; 27(8):2603–2609. PMID:
27112763.

24. Kim TY, Jang S, Park CM, Lee A, Lee YK, Kim HY, et al. Trends of incidence, mortality, and future projection of spinal fractures in Korea using Nationwide Claims Data. J Korean Med Sci. 2016; 31(5):801–805. PMID:
27134505.

25. Choi HJ, Shin CS, Ha YC, Jang SM, Jang SH, Park CM, et al. Burden of osteoporosis in adults in Korea: a national health insurance database study. J Bone Miner Metab. 2012; 30(1):54–58. PMID:
21633927.

26. Lee YK, Ha YC, Choi HJ, Jang S, Park C, Lim YT, et al. Bisphosphonate use and subsequent hip fracture in South Korea. Osteoporos Int. 2013; 24(11):2887–2892. PMID:
23681088.

27. Ha YC, Lee YK, Lim YT, Jang SM, Shin CS. Physicians' attitudes to contemporary issues on osteoporosis management in Korea. J Bone Metab. 2014; 21(2):143–149. PMID:
25006571.

28. Lee YK, Jang S, Ha YC. Management of osteoporosis in South Korea. Crit Rev Eukaryot Gene Expr. 2015; 25(1):33–40. PMID:
25955816.

29. Dell RM, Adams AL, Greene DF, Funahashi TT, Silverman SL, Eisemon EO, et al. Incidence of atypical nontraumatic diaphyseal fractures of the femur. J Bone Miner Res. 2012; 27(12):2544–2550. PMID:
22836783.

30. Giusti A, Hamdy NA, Papapoulos SE. Atypical fractures of the femur and bisphosphonate therapy: a systematic review of case/case series studies. Bone. 2010; 47(2):169–180. PMID:
20493982.
31. Lo JC, Huang SY, Lee GA, Khandelwal S, Provus J, Ettinger B, et al. Clinical correlates of atypical femoral fracture. Bone. 2012; 51(1):181–184. PMID:
22414379.

32. Marcano A, Taormina D, Egol KA, Peck V, Tejwani NC. Are race and sex associated with the occurrence of atypical femoral fractures? Clin Orthop Relat Res. 2014; 472(3):1020–1027. PMID:
24166075.

33. Soh HH, Chua IT, Kwek EB. Atypical fractures of the femur: effect of anterolateral bowing of the femur on fracture location. Arch Orthop Trauma Surg. 2015; 135(11):1485–1490. PMID:
26286640.

34. Chen LP, Chang TK, Huang TY, Kwok TG, Lu YC. The correlation between lateral bowing angle of the femur and the location of atypical femur fractures. Calcif Tissue Int. 2014; 95(3):240–247. PMID:
24980895.

35. Lee YK, Ahn S, Kim KM, Suh CS, Koo KH. Incidence rate of atypical femoral fracture after bisphosphonates treatment in Korea. J Korean Med Sci. 2018; 33(5):e38. PMID:
29349947.

36. Lee J, Lee JS, Park SH, Shin SA, Kim K. Cohort profile: the National Health Insurance Service-National Sample Cohort (NHIS-NSC), South Korea. Int J Epidemiol. 2017; 46(2):e15. PMID:
26822938.

37. Cheol Seong S, Kim YY, Khang YH, Heon Park J, Kang HJ, Lee H, et al. Data resource profile: the National Health Information Database of the National Health Insurance Service in South Korea. Int J Epidemiol. 2017; 46(3):799–800. PMID:
27794523.

39. Kim L, Kim JA, Kim S. A guide for the utilization of Health Insurance Review and Assessment Service National Patient Samples. Epidemiol Health. 2014; 36:e2014008. PMID:
25078381.

40. Jung SY, Sohn HS, Park EJ, Suh HS, Park JW, Kwon JW. Oral bisphosphonates and upper gastrointestinal cancer risks in Asians with osteoporosis: a nested case-control study using national retrospective cohort sample data from Korea. PLoS One. 2016; 11(3):e0150531. PMID:
26937968.

41. Schilcher J, Aspenberg P. Incidence of stress fractures of the femoral shaft in women treated with bisphosphonate. Acta Orthop. 2009; 80(4):413–415. PMID:
19568963.

42. Schilcher J, Michaëlsson K, Aspenberg P. Bisphosphonate use and atypical fractures of the femoral shaft. N Engl J Med. 2011; 364(18):1728–1737. PMID:
21542743.

43. Lyles KW, Colón-Emeric CS, Magaziner JS, Adachi JD, Pieper CF, Mautalen C, et al. Zoledronic acid and clinical fractures and mortality after hip fracture. N Engl J Med. 2007; 357(18):1799–1809. PMID:
17878149.

44. Camacho PM, Petak SM, Binkley N, Clarke BL, Harris ST, Hurley DL, et al. American Association of Clinical Endocrinologists and American College of Endocrinology Clinical Practice Guidelines for the diagnosis and treatment of postmenopausal osteoporosis - 2016--executive summary. Endocr Pract. 2016; 22(9):1111–1118. PMID:
27643923.

45. Hernlund E, Svedbom A, Ivergård M, Compston J, Cooper C, Stenmark J, et al. Osteoporosis in the European Union: medical management, epidemiology and economic burden. A report prepared in collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA). Arch Osteoporos. 2013; 8(1-2):136. PMID:
24113837.

46. Wang CC, Wu CH, Farley JF. Patterns of pharmacological treatment for osteoporosis among patients qualified for pharmacotherapy according to the national osteoporosis foundation guidelines. Ann Pharmacother. 2015; 49(9):995–1003. PMID:
26041809.

47. Compston J. NOGG and NICE: new guidelines and quality standards for osteoporosis. Maturitas. 2017; 106:97–98. PMID:
28803757.

48. Narongroeknawin P, Patkar NM, Shakoory B, Jain A, Curtis JR, Delzell E, et al. Validation of diagnostic codes for subtrochanteric, diaphyseal, and atypical femoral fractures using administrative claims data. J Clin Densitom. 2012; 15(1):92–102. PMID:
22071028.

49. Park BJ, Sung JH, Park KD, Seo SW, Kim S. Report of the Evaluation for Validity of Discharged Diagnoses in Korean Health Insurance Database. Seoul: Seoul National University;2003.
50. Lee J, Lee JS, Park SH, Shin SA, Kim K. Cohort profile: the National Health Insurance Service-National Sample Cohort (NHIS-NSC), South Korea. Int J Epidemiol. 2017; 46(2):e15. PMID:
26822938.





 PDF
PDF Citation
Citation Print
Print




 XML Download
XML Download