1. Cha YH, Ha YC, Yoo JI, Min YS, Lee YK, Koo KH. Effect of causes of surgical delay on early and late mortality in patients with proximal hip fracture. Arch Orthop Trauma Surg. 2017; 137(5):625–630. PMID:
28321571.

2. Wu J, Qu Y, Wang K, Chen Y. Healthcare resource utilization and direct medical costs for patients with osteoporotic fractures in China. Value Health Reg Issues. 2019; 18:106–111. PMID:
30909083.

3. Peeters CM, Visser E, Van de Ree CL, Gosens T, Den Oudsten BL, De Vries J. Quality of life after hip fracture in the elderly: a systematic literature review. Injury. 2016; 47(7):1369–1382. PMID:
27178770.

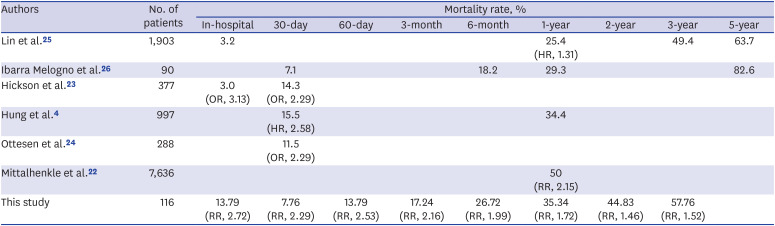
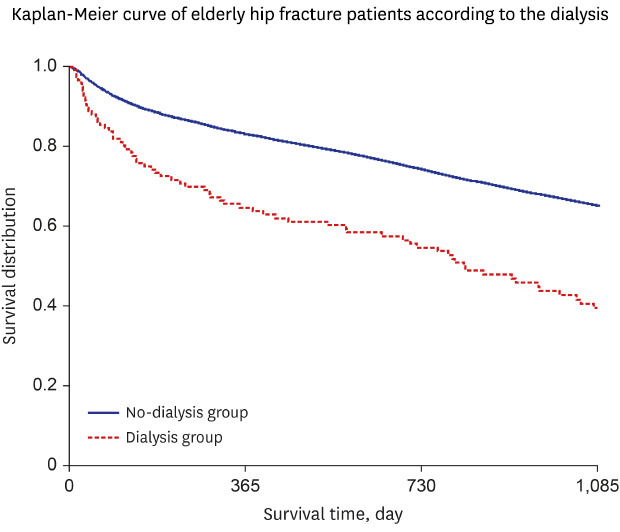
4. Hung LW, Hwang YT, Huang GS, Liang CC, Lin J. The influence of renal dialysis and hip fracture sites on the 10-year mortality of elderly hip fracture patients: a nationwide population-based observational study. Medicine (Baltimore). 2017; 96(37):e7618. PMID:
28906354.
5. Jager KJ, van Dijk PC, Dekker FW, Stengel B, Simpson K, Briggs JD, et al. The epidemic of aging in renal replacement therapy: an update on elderly patients and their outcomes. Clin Nephrol. 2003; 60(5):352–360. PMID:
14640241.

6. Saran R, Li Y, Robinson B, Abbott KC, Agodoa LY, Ayanian J, et al. US Renal Data System 2015 annual data report: epidemiology of kidney disease in the United States. Am J Kidney Dis. 2016; 67(3 Suppl 1):S1–S305.
7. Coco M, Rush H. Increased incidence of hip fractures in dialysis patients with low serum parathyroid hormone. Am J Kidney Dis. 2000; 36(6):1115–1121. PMID:
11096034.

8. Kim SM, Liu S, Long J, Montez-Rath ME, Leonard MB, Chertow GM. Declining rates of hip fracture in end-stage renal disease: analysis from the 2003–2011 Nationwide Inpatient Sample. J Bone Miner Res. 2017; 32(11):2297–2303. PMID:
28639740.

9. Kim SM, Long J, Montez-Rath M, Leonard M, Chertow GM. Hip fracture in patients with non-dialysis-requiring chronic kidney disease. J Bone Miner Res. 2016; 31(10):1803–1809. PMID:
27145189.

10. Song KS, Yoon SP, Lee SK, Lee SH, Yang BS, Park BM, et al. The results of proximal femoral nail for intertrochanteric fracture in hemodialysis patient. Hip Pelvis. 2017; 29(1):54–61. PMID:
28316963.

11. Yoon BH, Koo KH. Hip fracture in chronic kidney disease patients: necessity of multidisciplinary approach. J Korean Med Sci. 2017; 32(12):1906–1907. PMID:
29115068.

12. Seong SC, Kim YY, Park SK, Khang YH, Kim HC, Park JH, et al. Cohort profile: the National Health Insurance Service-National Health Screening Cohort (NHIS-HEALS) in Korea. BMJ Open. 2017; 7(9):e016640.

13. Lee J, Lee JS, Park SH, Shin SA, Kim K. Cohort profile: the National Health Insurance Service-National Sample Cohort (NHIS-NSC), South Korea. Int J Epidemiol. 2017; 46(2):e15. PMID:
26822938.

14. Park C, Jang S, Jang S, Ha YC, Lee YK, Yoon HK, et al. Identification and validation of osteoporotic hip fracture using the national health insurance database. J Korean Hip Soc. 2010; 22(4):305–311.

15. Lee YK, Ha YC, Choi HJ, Jang S, Park C, Lim YT, et al. Bisphosphonate use and subsequent hip fracture in South Korea. Osteoporos Int. 2013; 24(11):2887–2892. PMID:
23681088.

16. Choi HS, Han KD, Jung JH, Kim CS, Bae EH, Ma SK, et al. The risk of end-stage renal disease in systemic lupus erythematosus: a nationwide population-based study in Korea. Medicine (Baltimore). 2019; 98(28):e16420. PMID:
31305460.
17. Quan H, Sundararajan V, Halfon P, Fong A, Burnand B, Luthi JC, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005; 43(11):1130–1139. PMID:
16224307.

18. Papademetriou V, Lovato L, Doumas M, Nylen E, Mottl A, Cohen RM, et al. Chronic kidney disease and intensive glycemic control increase cardiovascular risk in patients with type 2 diabetes. Kidney Int. 2015; 87(3):649–659. PMID:
25229335.

19. Fang Y, Ginsberg C, Sugatani T, Monier-Faugere MC, Malluche H, Hruska KA. Early chronic kidney disease-mineral bone disorder stimulates vascular calcification. Kidney Int. 2014; 85(1):142–150. PMID:
23884339.

20. Hruska KA, Sugatani T, Agapova O, Fang Y. The chronic kidney disease - Mineral bone disorder (CKD-MBD): advances in pathophysiology. Bone. 2017; 100:80–86. PMID:
28119179.

21. Nitsch D, Mylne A, Roderick PJ, Smeeth L, Hubbard R, Fletcher A. Chronic kidney disease and hip fracture-related mortality in older people in the UK. Nephrol Dial Transplant. 2009; 24(5):1539–1544. PMID:
19075194.

22. Mittalhenkle A, Gillen DL, Stehman-Breen CO. Increased risk of mortality associated with hip fracture in the dialysis population. Am J Kidney Dis. 2004; 44(4):672–679. PMID:
15384018.

23. Hickson LJ, Farah WH, Johnson RL, Thorsteinsdottir B, Ubl DS, Yuan BJ, et al. Death and postoperative complications after hip fracture repair: dialysis effect. Kidney Int Rep. 2018; 3(6):1294–1303. PMID:
30450456.

24. Ottesen TD, Yurter A, Shultz BN, Galivanche AR, Zogg CK, Bovonratwet P, et al. Dialysis dependence is associated with significantly increased odds of perioperative adverse events after geriatric hip fracture surgery even after controlling for demographic factors and comorbidities. J Am Acad Orthop Surg Glob Res Rev. 2019; 3(8):e086. PMID:
31592508.

25. Lin ZZ, Wang JJ, Chung CR, Huang PC, Su BA, Cheng KC, et al. Epidemiology and mortality of hip fracture among patients on dialysis: Taiwan National Cohort Study. Bone. 2014; 64:235–239. PMID:
24780875.

26. Ibarra Melogno S, Chifflet L, Rey R, Leiva G, Morales N, Albornoz H. Long-term results of hip arthroplasty in patients on dialysis for chronic renal failure. Mortality and implant survival in the National Registry of Uruguay since 2000. Rev Esp Cir Ortop Traumatol. 2019; 63(3):187–191. PMID:
30910466.

27. Tosun B, Atmaca H, Gok U. Operative treatment of hip fractures in patients receiving hemodialysis. Musculoskelet Surg. 2010; 94(2):71–75. PMID:
20882378.

28. Kalra S, McBryde CW, Lawrence T. Intracapsular hip fractures in end-stage renal failure. Injury. 2006; 37(2):175–184. PMID:
16426611.

29. Karaeminogullari O, Demirors H, Sahin O, Ozalay M, Ozdemir N, Tandogan RN. Analysis of outcomes for surgically treated hip fractures in patients undergoing chronic hemodialysis. J Bone Joint Surg Am. 2007; 89(2):324–331. PMID:
17272447.

30. Sakabe T, Imai R, Murata H, Fujioka M, Iwamoto N, Ono T, et al. Life expectancy and functional prognosis after femoral neck fractures in hemodialysis patients. J Orthop Trauma. 2006; 20(5):330–336. PMID:
16766936.

31. Blacha J, Kolodziej R, Karwanski M. Bipolar cemented hip hemiarthroplasty in patients with femoral neck fracture who are on hemodialysis is associated with risk of stem migration. Acta Orthop. 2009; 80(2):174–178. PMID:
19404798.





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download