This article has been
cited by other articles in ScienceCentral.
Abstract
Social distancing has been adopted as one of basic protective measures against coronavirus disease 2019 (COVID-19). During 2019–2020 season, influenza epidemic period was exceptionally short and epidemic peak was low in comparison with previous seasons in Korea. Influenza epidemic pattern was bimodal in 2016–2017 and 2018–2019 seasons, however, influenza viruses have rarely been circulating in spring, 2020 in Korea. Although multiple factors could affect the size of influenza epidemic, extensive application of nonpharmaceutical interventions including mask wearing and social distancing in response to COVID-19 seems to be a major factor of reduced influenza epidemic. Social distancing measures with high feasibility and high acceptability should be implemented even if severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) vaccines are developed in the future. Establishment of guideline for workplace social distancing is needed and it would contribute to reduce disease burden of influenza, especially in vaccine mismatch year.
Go to :

Graphical Abstract
Go to :

Keywords: Social Distancing, Coronavirus Disease 2019, Influenza
Coping with coronavirus disease 2019 (COVID-19), social distancing has been adopted as one of basic protective measures against severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). Nonpharmaceutical interventions (NPIs) include actions to mitigate the spread of respiratory viruses: personal protective measures such as hand hygiene, cough etiquette, and voluntary home stay of ill persons; community measures such as school closures, social distancing in workplace, and avoidance of mass gathering.
1
High viral loads of SARS-CoV-2 in upper respiratory tract of human and transmission potential in asymptomatic patients with COVID-19 emphasize the application of NPIs to control of SARS-CoV-2 transmission especially in situation of lack of vaccine and therapeutics.
23 Previous study showed that SARS-CoV-2 viral load of upper respiratory tract in the asymptomatic patient was similar to those in the symptomatic patients.
4
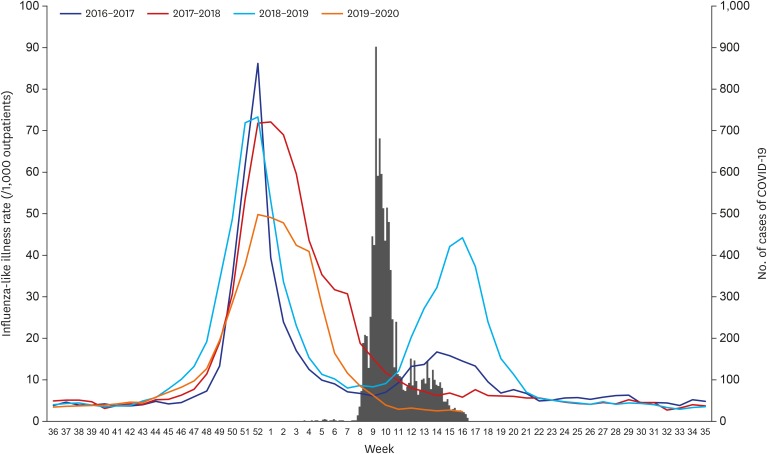
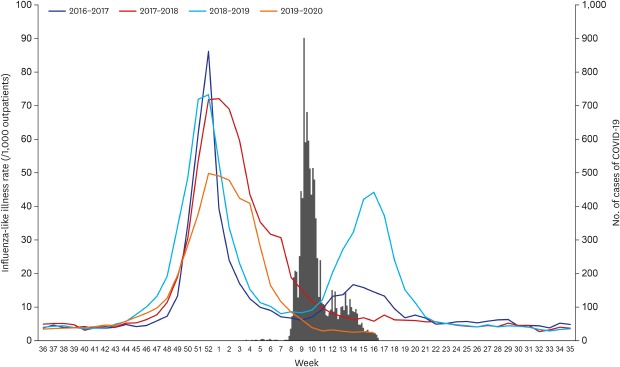
During 2019-2020 season, influenza epidemic period was exceptionally short and epidemic peak was low in comparison with previous seasons in Korea (
Fig. 1 and
Table 1). Official influenza epidemic period by Korea Centers for Disease Control and Prevention (KCDC) was from 15 November 2019 to 27 March 2020, which is 6–12 weeks shorter than those of previous seasons.
5 Influenza epidemic pattern was bimodal in 2016–2017 and 2018-2019 seasons, however, influenza viruses have rarely been circulating in spring, 2020.
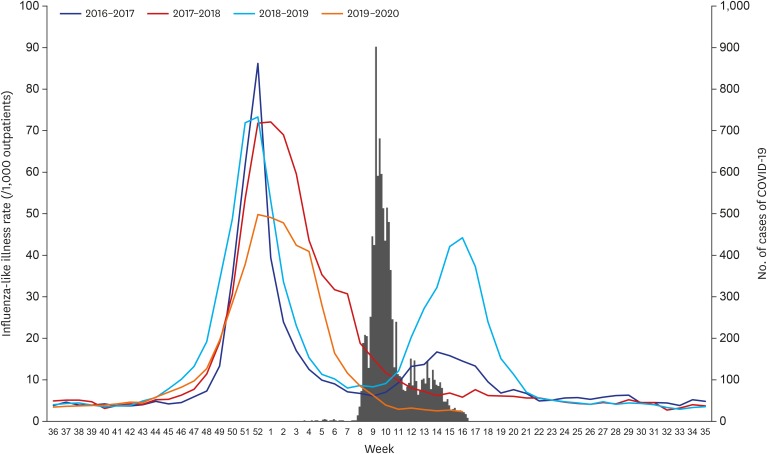 | Fig. 1
Influenza-like illness rate during 2016-2020 seasons and number of cases of COVID-19 as of 18 Apr 2020, Korea.78 ILI rate of the week 53, 2016 (63.5) was not shown in the figure.
COVID-19 = coronavirus disease 2019, ILI = influenza-like illness.

|
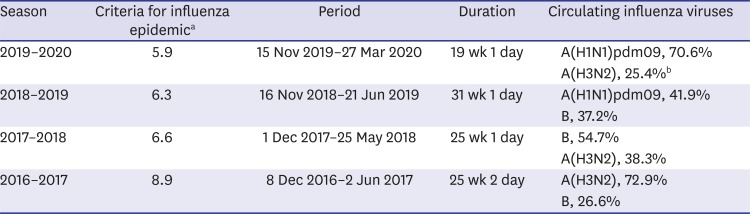
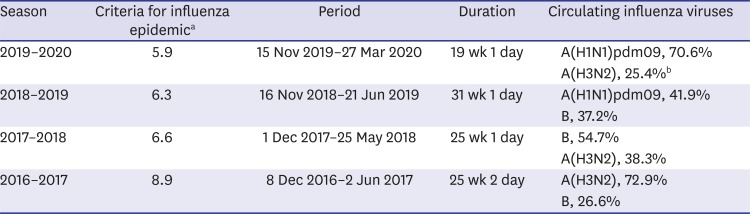
Table 1
Current influenza epidemic in Korea by Korea Centers for Disease Control and Prevention511121314
|
Season |
Criteria for influenza epidemica
|
Period |
Duration |
Circulating influenza viruses |
|
2019–2020 |
5.9 |
15 Nov 2019–27 Mar 2020 |
19 wk 1 day |
A(H1N1)pdm09, 70.6% |
|
A(H3N2), 25.4%b
|
|
2018–2019 |
6.3 |
16 Nov 2018–21 Jun 2019 |
31 wk 1 day |
A(H1N1)pdm09, 41.9% |
|
B, 37.2% |
|
2017–2018 |
6.6 |
1 Dec 2017–25 May 2018 |
25 wk 1 day |
B, 54.7% |
|
A(H3N2), 38.3% |
|
2016–2017 |
8.9 |
8 Dec 2016–2 Jun 2017 |
25 wk 2 day |
A(H3N2), 72.9% |
|
B, 26.6% |

Extent and duration of influenza epidemic vary from year to year. Multiple factors such as characteristics of circulating influenza viruses, immunity of the population, and transmissibility of viruses could affect the size of influenza epidemic. Reduced health-care-seeking behaviors of the population under COVID-19 pandemic could affect short duration of influenza epidemic during 2019-2020 season. However, extensive application of NPIs including wearing a mask and social distancing in response to COVID-19 seems to be a major factor of reduced influenza epidemic in 2019-2020, Korea.
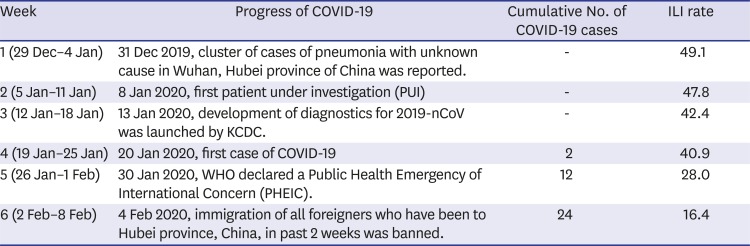
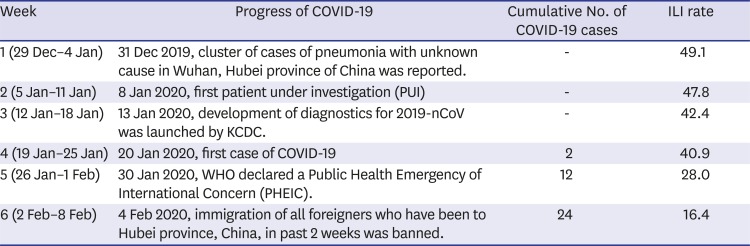
Since a cluster of cases of pneumonia with unknown cause in Wuhan, China was reported on 31 December 2019, the first case of COVID-19 was confirmed on 20 January 2020 in Korea.
67 After the first confirmed case, level of risk perception regarding SARS-CoV-2 infection raised among Korean population. Facing a movement of population and family gathering during Lunar New Year's holiday (24-27 January 2020), KCDC promoted to practice hand hygiene and mask wearing in persons who have respiratory symptoms such as cough.
7 Government raised the national infectious disease alert level to Orange on 27 Jan 2020. Influenza-like illness rate decreased steeply from 40.9 in week 4 to 16.4 in week 6 (
Table 2).
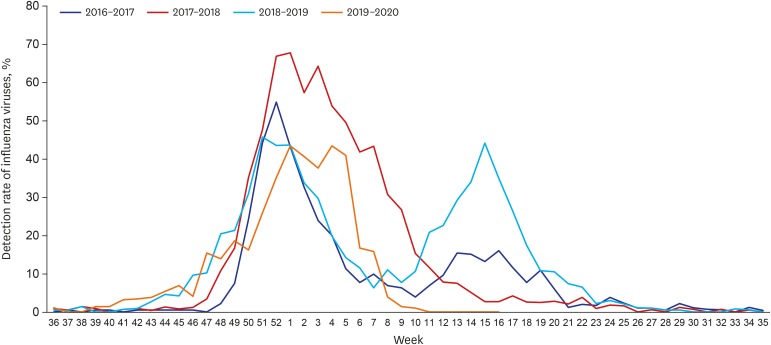
8 During 2019-2020 season, detection rate of influenza viruses by Korea Influenza and Respiratory Viruses Surveillance System was also lower than those of previous three influenza seasons (
Fig. 2).
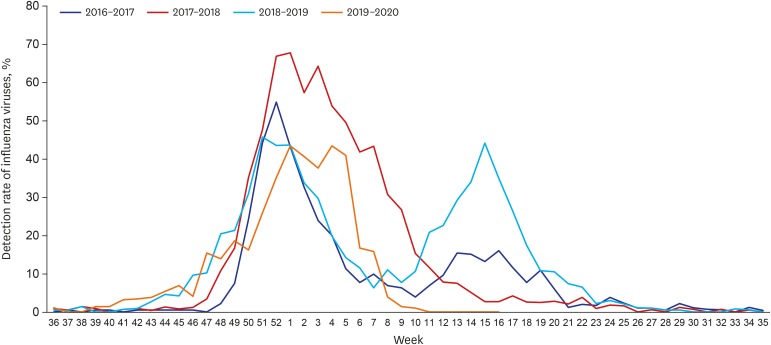 | Fig. 2
Detection rate of influenza viruses by KINRESS during 2016-2020 season as of 18 Apr 2020.16 Data of the week 53, 2016 (46.8%) was not shown in the figure.
KINRESS = Korea Influenza and Respiratory Viruses Surveillance System.

|
Table 2
Progress of COVID-19 and influenza-like illness rate from week 1 to week 6, 202067815
|
Week |
Progress of COVID-19 |
Cumulative No. of COVID-19 cases |
ILI rate |
|
1 (29 Dec–4 Jan) |
31 Dec 2019, cluster of cases of pneumonia with unknown cause in Wuhan, Hubei province of China was reported. |
- |
49.1 |
|
2 (5 Jan–11 Jan) |
8 Jan 2020, first patient under investigation (PUI) |
- |
47.8 |
|
3 (12 Jan–18 Jan) |
13 Jan 2020, development of diagnostics for 2019-nCoV was launched by KCDC. |
- |
42.4 |
|
4 (19 Jan–25 Jan) |
20 Jan 2020, first case of COVID-19 |
2 |
40.9 |
|
5 (26 Jan–1 Feb) |
30 Jan 2020, WHO declared a Public Health Emergency of International Concern (PHEIC). |
12 |
28.0 |
|
6 (2 Feb–8 Feb) |
4 Feb 2020, immigration of all foreigners who have been to Hubei province, China, in past 2 weeks was banned. |
24 |
16.4 |

In Hong Kong, 44% reduction in influenza transmission in the community was estimated in early February, 2020, after the implementation of social distancing and changes in population behaviors to control the spread of COVID-19.
9 Personal protective measures as well as workplace social distancing such as stay home from work when sick and teleworking contribute to reduction of transmission of influenza viruses and decrease the level of epidemic peak of influenza. Workplace social distancing measures showed a reduction of 23% in the cumulative influenza attack rate in the population in a previous systematic review.
10
Social distancing measures with high feasibility and high acceptability should be implemented even if SARS-CoV-2 vaccines are developed in the future. Establishment of guideline for workplace social distancing might be considered. It would contribute to reduce influenza viral transmission and overall disease burden of influenza. Above all, social distancing will contribute to control influenza in vaccine mismatch year.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download