This article has been
cited by other articles in ScienceCentral.
Abstract
Consumptive hypothyroidism is a rare paraneoplastic syndrome characterized by excessive inactivation of the thyroid hormones due to increased type 3 iodothyronine deiodinase activity of tumors. We report the case of severe consumptive hypothyroidism in a 1-month-old boy with infantile hepatic hemangiomas who presented with cardiac failure and cholestasis. Diffuse infiltration of hepatic hemangiomas was detected on abdominal imaging studies, and thyroid function screening test revealed severe hypothyroidism, which necessitated the administration of higher-than-usual doses of levothyroxine for the normalization of thyroid function. The patient was successfully treated with propranolol, prednisolone, and levothyroxine, and he showed normal thyroid function at 3 months of age and normal neurodevelopment at 9 months of age. This case highlights the importance of early recognition and prompt management of consumptive hypothyroidism in patients with infantile hepatic hemangiomas.
Go to :

Graphical Abstract
Go to :

Keywords: Hypothyroidism, Infantile Hepatic Hemangioma, Iodothyronine Deiodinase Type 3
INTRODUCTION
Infantile hemangiomas are the most common benign vascular tumors of infancy, and they occur in approximately 3%–5% of infants.
1 They commonly appear on the skin as solitary or multiple lesions, but they may also affect visceral organs such as the liver.
2 They undergo rapid proliferation in the first year of life and then undergo gradual spontaneous involution over several years.
23 Multifocal or diffuse forms of infantile hepatic hemangioma may be associated with serious complications such as high-output cardiac failure, respiratory distress, abdominal compartment syndrome, or hepatic failure.
4 Consumptive hypothyroidism, a rare type of hypothyroidism, is another complication of infantile hepatic hemangiomas.
5 Its mechanism involves increased tumoral expression of type 3 iodothyronine deiodinase (D3), which catalyzes inner-ring deiodination of thyroxine (T4) to reverse triiodothyronine (rT3) and triiodothyronine (T3) to 3,3′-diiodothyronine (T2), thereby inactivating the thyroid hormones.
5
Here, we report a case of consumptive hypothyroidism in a patient with infantile hepatic hemangiomas who presented with high-output cardiac failure and cholestasis and was successfully treated with a combination of propranolol, prednisolone, and levothyroxine.
Go to :

CASE DESCRIPTION
A 1-month-old boy was referred to a tertiary center with progressive abdominal distension in December 20, 2018. He was born by vaginal delivery with no perinatal problems at 38 + 1 weeks of gestation with a weight of 3.08 kg. He had normal neonatal screening test results and no family history of thyroid disorders. At presentation, he had normal growth with a height of 54.2 cm (25–50th percentile) and a weight of 4.3 kg (25th percentile). Physical examination revealed anemic conjunctivae, icteric sclerae, abdominal distension, and hepatomegaly, with the liver palpable 6 cm below the right costal margin. He had respiratory difficulties with grade 3 systolic murmurs at both upper sternal borders. No cutaneous lesions such as hemangiomas or petechiae were observed.
Laboratory examinations revealed elevated liver enzyme levels (aspartate transaminase [AST] level, 176 IU/mL; alanine transaminase [ALT] level, 53 IU/mL), hyperbilirubinemia (total bilirubin [TB] concentration, 19.7 mg/dL; direct bilirubin concentration, 1.9 mg/dL), and prolonged prothrombin time (19.0 seconds; international normalized ratio, 1.64). He also had respiratory acidosis (pH, 7.29; pCO
2, 57 mmHg; HCO
3
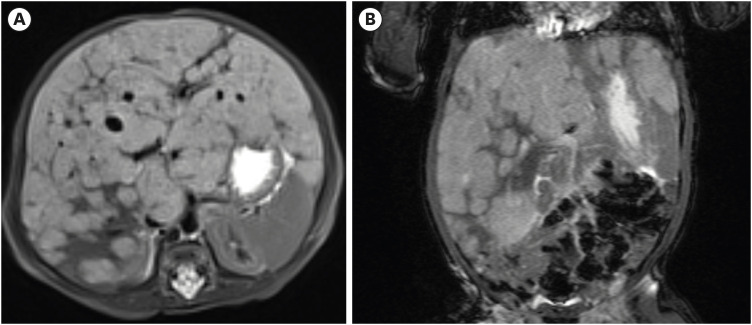
−, 27.4 mmol/L), hemolytic anemia (hemoglobin concentration, 8.6 g/dL; reticulocyte count, 5.2%; haptoglobin concentration, ˂ 7 mg/dL), and elevated brain natriuretic peptide level of 2,082 pg/mL (normal range, 0–100 pg/mL). Chest radiography showed cardiomegaly with bilateral pulmonary edema, and echocardiography suggested high-output cardiac failure with no intracardiac anomaly (ejection fraction, 77.4%; fractional shortening, 44%; left ventricular dimension at diastole, 24.8 mm; z-score, 1.9). Abdominal ultrasonography (US) revealed multiple hypoechoic nodular lesions in liver parenchyma with increased vascularity, which was confirmed using liver magnetic resonance imaging as diffuse hepatic hemangiomas (
Fig. 1). Brain US findings were normal with no intracranial involvement of the hemangioma.
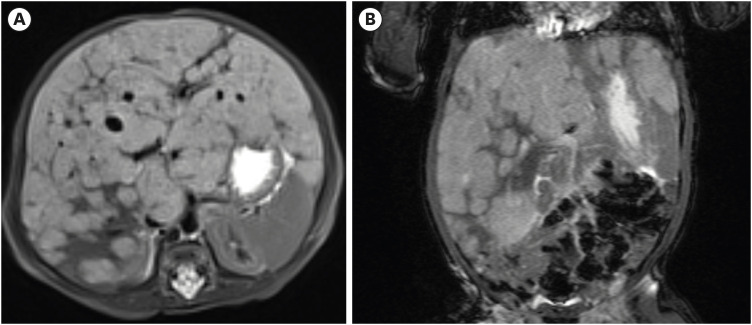 | Fig. 1 Liver magnetic resonance imaging findings at initial presentation showing multiple nodular lesions with T2 intermediate-high signal intensity and filling enhancement pattern in the liver parenchyma, (A) coronal view, (B) axial view. The images are published under agreement of the patient's parents.
|
Thyroid function screening test revealed hypothyroidism with elevated thyrotropin (thyroid-stimulating hormone; TSH) level (> 100 μIU/mL; normal range, 0.35–4.94 μIU/mL), low free T4 (fT4) level (0.59 ng/dL; normal range, 0.70–1.48 ng/dL), and low total T3 level (˂ 40 ng/dL; normal range, 64–152 ng/dL). Thyroid US showed a eutopic gland of normal size and echogenicity. He was treated with oral propranolol (1 mg/kg/day), prednisolone (2 mg/kg/day), levothyroxine (50 μg/day, 11 μg/kg/day), and diuretics for the diffuse form of infantile hepatic hemangiomas with high-output cardiac failure and severe hypothyroidism, and high-flow nasal cannula was used for respiratory support.
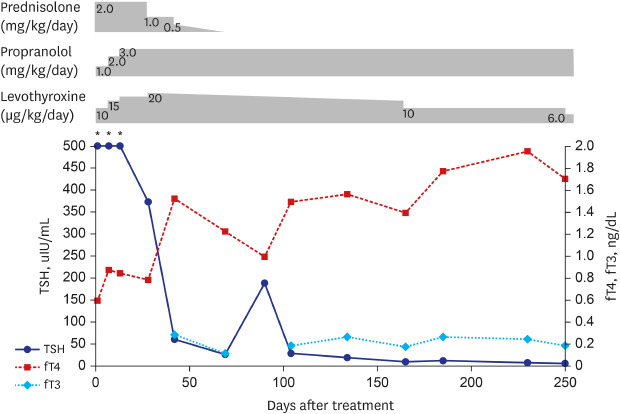
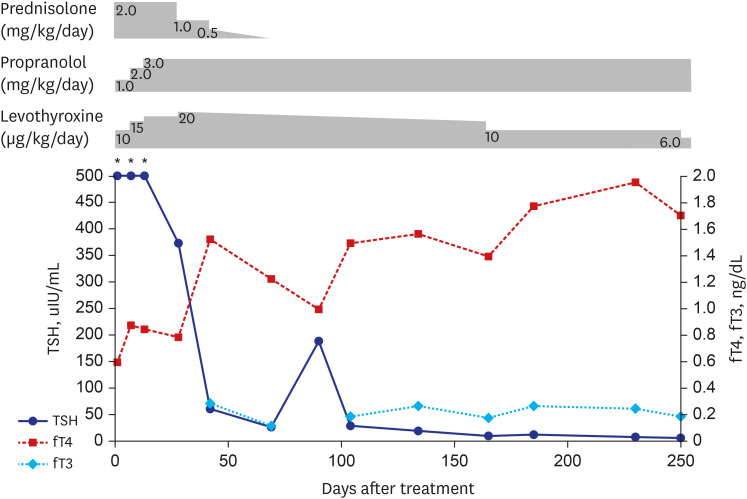
With medical treatment, he showed gradual improvements in clinical status and laboratory profile. He was weaned off the high-flow nasal cannula after 2 weeks of treatment, and his abdominal circumference remained stable. His blood and liver function test results also improved (hemoglobin concentration, 12.0 g/dL; AST level, 50 IU/mL; ALT level, 26 IU/mL; TB concentration, 6.2 mg/dL). The levothyroxine dose was then adjusted according to the thyroid function test results (
Fig. 2). He was discharged with propranolol (3 mg/kg/day), prednisolone (2 mg/kg/day), and levothyroxine (50 μg/day, 17 μg/kg/day) at 2 months of age (after 3 weeks of treatment).
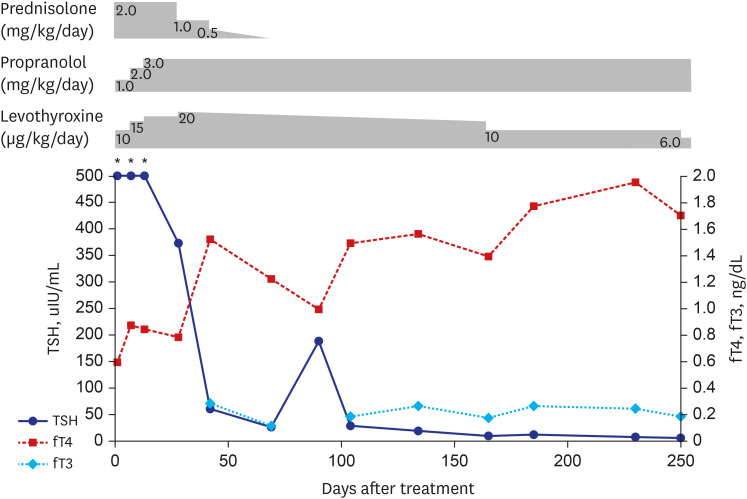 | Fig. 2
Changes in thyroid function over time according to treatment course.
TSH = thyroid-stimulating hormone, fT4 = free thyroxine, fT3 = free triiodothyronine.
*Initial thyroid function test showed TSH level over 500 μIU/mL.

|
At 4 months of age, abdominal US showed a reduction in the size of the hepatic hemangiomas. Oral prednisolone was gradually tapered off over 3 months, while propranolol was continued. His fT4 level normalized by 3 months of age (1.52 ng/dL) with a normal free T3 (fT3) level of 0.28 ng/dL (normal range, 0.19–0.32 ng/dL), while his TSH level normalized at 7 months of age (4.67 μIU/mL). The levothyroxine dose was increased to 112.5 μg/day (20 μg/kg/day) by 4 months of age, and following regression of the hemangiomas, it was gradually reduced to 50 μg/day (7 μg/kg/day) by 7 months of age (
Fig. 2). Treatment was well tolerated without documented adverse effects. He showed normal growth (height, 70 cm; weight, 8.1 kg; 10–25th percentile) and neurodevelopment at 9 months of age.
Ethics statement
This study was approved by the Institutional Review Board of the Seoul National University Hospital (No. 1908-093-105) with waiver of informed consent. The images are published under agreement of the patient's parents.
Go to :

DISCUSSION
In this case report, we described a patient with hepatic hemangioma in early infancy who had severe consumptive hypothyroidism, and following early detection and prompt management, was successfully treated with levothyroxine, propranolol, and prednisolone.
Consumptive hypothyroidism is a rare form of hypothyroidism that was first reported in an infant with massive hepatic hemangiomas by Huang et al.
5 High activity levels of D3, which catalyzes the conversion of T4 to rT3 and T3 to T2, were identified in the hemangioma specimen. D3, a selenoenzyme that is a physiological inactivator of thyroid hormones, is normally found in the brain and placenta, and it prevents the inappropriate activation of thyroid hormones.
6 Severe hypothyroidism can occur when the rate of peripheral thyroid hormone inactivation by tumoral D3 exceeds the thyroid hormone synthesis rate.
7
The severe hypothyroidism in this patient with hepatic hemangioma was comparable to the consumptive hypothyroidism described in earlier reports.
5 Congenital hypothyroidism can be excluded on the basis of normal neonatal screening test and thyroid US results. Although, we could not measure the rT3 level (this is unavailable in Korea) or tissue D3 activity (due to the risk of bleeding from biopsy), the requirement of higher-than-usual dose of levothyroxine for the normalization of thyroid function and gradual dose reduction to the usual dose after tumor regression support the diagnosis of consumptive hypothyroidism.
Because the clinical symptoms and signs of hypothyroidism can be subtle or masked due to other complications of hepatic hemangioma, it is important to maintain a high index of suspicion. Our patient did not show any signs or symptoms of hypothyroidism; however, severe hypothyroidism was detected on thyroid function screening test. Thyroid hormone is essential for brain development in infancy, and delayed treatment of hypothyroidism may result in poor neurodevelopmental outcomes. Because there is a correlation between tumoral D3 activity and tumor burden, thyroid function should be assessed in patients with large or diffuse forms of hemangioma in the first year of life when hemangiomas can further proliferate.
58
Management of consumptive hypothyroidism consists of 2 parts, namely tumor-targeted therapy and thyroid hormone replacement.
9 Because some hemangiomas involute spontaneously, careful observation can be an option. However, as in this case, patients with life-threatening conditions such as cardiac failure or severe hypothyroidism need prompt medical treatment.
3 There are several reports of successful treatment of hemangiomas using propranolol, corticosteroids, interferon alpha, vincristine, and cyclophosphamide.
1011 Thyroid hormone replacement with levothyroxine alone or combined with liothyronine has been used to treat consumptive hypothyroidism.
101112 In this case, treatment with propranolol and short-term systemic steroids resulted in regression of tumors and improvements in clinical symptoms with no significant adverse effects. Furthermore, rapid increase in the levothyroxine dose can effectively normalize fT4 and fT3 levels at 3 months of age without liothyronine use.
Long-term neurodevelopmental outcomes of early detection and aggressive management of consumptive hypothyroidism with thyroid hormone replacement appear to be promising.
9 Because hemangiomas undergo involution over time, most patients can be weaned off thyroid hormone replacement. Thyroid function tests should be performed at short intervals and the test results monitored for dose titration to avoid iatrogenic hyperthyroidism.
7
In this report, we described the case of a patient with infantile hepatic hemangioma complicated with high-output cardiac failure, cholestasis, coagulopathy, and consumptive hypothyroidism who was successfully managed with propranolol, prednisolone, and levothyroxine. Because most patients do not show clinical symptoms and signs of hypothyroidism, screening for hypothyroidism is of utmost importance in patients with infantile hepatic hemangiomas.
Go to :





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download