1. Leung DY, Boguniewicz M, Howell MD, Nomura I, Hamid QA. New insights into atopic dermatitis. J Clin Invest. 2004; 113(5):651–657. PMID:
14991059.

2. Schneider L, Tilles S, Lio P, Boguniewicz M, Beck L, LeBovidge J, et al. Atopic dermatitis: a practice parameter update 2012. J Allergy Clin Immunol. 2013; 131(2):295–299.e1. PMID:
23374261.
3. Thomsen SF. Atopic dermatitis: natural history, diagnosis, and treatment. ISRN Allergy. 2014; 2014:354250. PMID:
25006501.

4. Lee SY, Lee E, Park YM, Hong SJ. Microbiome in the gut-skin axis in atopic dermatitis. Allergy Asthma Immunol Res. 2018; 10(4):354–362. PMID:
29949831.

5. Abrahamsson TR, Jakobsson HE, Andersson AF, Björkstén B, Engstrand L, Jenmalm MC. Low diversity of the gut microbiota in infants with atopic eczema. J Allergy Clin Immunol. 2012; 129(2):434–440. PMID:
22153774.

6. Song H, Yoo Y, Hwang J, Na YC, Kim HS.
Faecalibacterium prausnitzii subspecies-level dysbiosis in the human gut microbiome underlying atopic dermatitis. J Allergy Clin Immunol. 2016; 137(3):852–860. PMID:
26431583.
7. Rather IA, Bajpai VK, Kumar S, Lim J, Paek WK, Park YH. Probiotics and atopic dermatitis: an overview. Front Microbiol. 2016; 7:507. PMID:
27148196.

8. Nonaka Y, Izumo T, Izumi F, Maekawa T, Shibata H, Nakano A, et al. Antiallergic effects of
Lactobacillus pentosus strain S-PT84 mediated by modulation of Th1/Th2 immunobalance and induction of IL-10 production. Int Arch Allergy Immunol. 2008; 145(3):249–257. PMID:
17914277.
9. Bae MJ, Kim HK, Lim S, Lee SY, Shin HS, Kim JE, et al.
Lactobacillus pentosus KF340 alleviates house dust mite-induced murine atopic dermatitis via the secretion of IL-10-producing splenic B10 cells. J Funct Foods. 2016; 26:258–267.
10. Kim J, Lee BS, Kim B, Na I, Lee J, Lee JY, et al. Identification of atopic dermatitis phenotypes with good responses to probiotics (
Lactobacillus plantarum CJLP133) in children. Benef Microbes. 2017; 8(5):755–761. PMID:
29035111.
11. Hanifin JM, Rajka G. Diagnostic features of atopic dermatitis. Acta Derm Venereol (Stockh). 1980; 60(92):S44–7.
12. Stadler JF. Severity scoring of atopic dermatitis: the SCORAD index. Consensus Report of the European Task Force on Atopic Dermatitis. Dermatology. 1993; 186(1):23–31. PMID:
8435513.
13. Garcia Bartels N, Scheufele R, Prosch F, Schink T, Proquitté H, Wauer RR, et al. Effect of standardized skin care regimens on neonatal skin barrier function in different body areas. Pediatr Dermatol. 2010; 27(1):1–8. PMID:
20199402.

14. Caporaso JG, Kuczynski J, Stombaugh J, Bittinger K, Bushman FD, Costello EK, et al. QIIME allows analysis of high-throughput community sequencing data. Nat Methods. 2010; 7(5):335–336. PMID:
20383131.

15. Ji GE. Probiotics in primary prevention of atopic dermatitis. Forum Nutr. 2009; 61:117–128. PMID:
19367116.

16. Wang IJ, Wang JY. Children with atopic dermatitis show clinical improvement after
Lactobacillus exposure. Clin Exp Allergy. 2015; 45(4):779–787. PMID:
25600169.
17. Niccoli AA, Artesi AL, Candio F, Ceccarelli S, Cozzali R, Ferraro L, et al. Preliminary results on clinical effects of probiotic
Lactobacillus salivarius LS01 in children affected by atopic dermatitis. J Clin Gastroenterol. 2014; 48(Suppl 1):S34–S36. PMID:
25291124.
18. Kim SO, Ah YM, Yu YM, Choi KH, Shin WG, Lee JY. Effects of probiotics for the treatment of atopic dermatitis: a meta-analysis of randomized controlled trials. Ann Allergy Asthma Immunol. 2014; 113(2):217–226. PMID:
24954372.

19. Boyle RJ, Bath-Hextall FJ, Leonardi-Bee J, Murrell DF, Tang ML. Probiotics for treating eczema. Cochrane Database Syst Rev. 2008; 8(4):CD006135.

20. Huang R, Ning H, Shen M, Li J, Zhang J, Chen X. Probiotics for the treatment of atopic dermatitis in children: a systematic review and meta-analysis of randomized controlled trials. Front Cell Infect Microbiol. 2017; 7:392. PMID:
28932705.

21. Shimosato T, Tomida K, Otani H. Effect of Lactobacillus pentosus ONRIC b0240 on intestinal IgA production in mice fed differing levels of protein. J Agric Food Chem. 2011; 59(6):2646–2651. PMID:
21361374.
22. Shimizu K, Sato H, Suga Y, Yamahira S, Toba M, Hamuro K, et al. The effects of
Lactobacillus pentosus strain b240 and appropriate physical training on salivary secretory IgA levels in elderly adults with low physical fitness: a randomized, double-blind, placebo-controlled trial. J Clin Biochem Nutr. 2014; 54(1):61–66. PMID:
24426193.
23. Kotani Y, Kunisawa J, Suzuki Y, Sato I, Saito T, Toba M, et al. Role of
Lactobacillus pentosus Strain b240 and the Toll-like receptor 2 axis in Peyer's patch dendritic cell-mediated immunoglobulin A enhancement. PLoS One. 2014; 9(3):e91857. PMID:
24632732.
24. Chang YS, Trivedi MK, Jha A, Lin YF, Dimaano L, García-Romero MT. Synbiotics for prevention and treatment of atopic dermatitis: a meta-analysis of randomized clinical trials. JAMA Pediatr. 2016; 170(3):236–242. PMID:
26810481.
25. Dang D, Zhou W, Lun ZJ, Mu X, Wang DX, Wu H. Meta-analysis of probiotics and/or prebiotics for the prevention of eczema. J Int Med Res. 2013; 41(5):1426–1436. PMID:
23908398.

26. Rosenfeldt V, Benfeldt E, Nielsen SD, Michaelsen KF, Jeppesen DL, Valerius NH, et al. Effect of probiotic
Lactobacillus strains in children with atopic dermatitis. J Allergy Clin Immunol. 2003; 111(2):389–395. PMID:
12589361.
27. Gerasimov SV, Vasjuta VV, Myhovych OO, Bondarchuk LI. Probiotic supplement reduces atopic dermatitis in preschool children: a randomized, double-blind, placebo-controlled, clinical trial. Am J Clin Dermatol. 2010; 11(5):351–361. PMID:
20642296.
28. Gensollen T, Blumberg RS. Correlation between early-life regulation of the immune system by microbiota and allergy development. J Allergy Clin Immunol. 2017; 139(4):1084–1091. PMID:
28390575.

29. Meneghin F, Fabiano V, Mameli C, Zuccotti GV. Probiotics and atopic dermatitis in children. Pharmaceuticals (Basel). 2012; 5(7):727–744. PMID:
24281709.

30. Arrieta MC, Stiemsma LT, Amenyogbe N, Brown EM, Finlay B. The intestinal microbiome in early life: health and disease. Front Immunol. 2014; 5:427. PMID:
25250028.

31. Claesson MJ, Cusack S, O'Sullivan O, Greene-Diniz R, de Weerd H, Flannery E, et al. Composition, variability, and temporal stability of the intestinal microbiota of the elderly. Proc Natl Acad Sci U S A. 2011; 108(Suppl 1):4586–4591. PMID:
20571116.

32. Nylund L, Nermes M, Isolauri E, Salminen S, de Vos WM, Satokari R. Severity of atopic disease inversely correlates with intestinal microbiota diversity and butyrate-producing bacteria. Allergy. 2015; 70(2):241–244. PMID:
25413686.

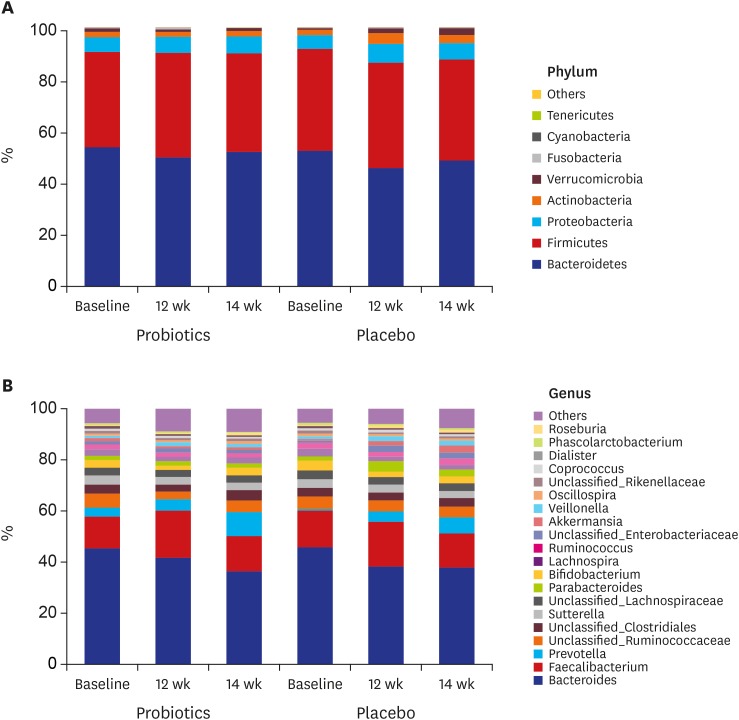
33. Fang Z, Lu W, Zhao J, Zhang H, Qian L, Wang Q, et al. Probiotics modulate the gut microbiota composition and immune responses in patients with atopic dermatitis: a pilot study. Eur J Nutr. 2019.

34. Sistek D, Kelly R, Wickens K, Stanley T, Fitzharris P, Crane J. Is the effect of probiotics on atopic dermatitis confined to food sensitized children? Clin Exp Allergy. 2006; 36(5):629–633. PMID:
16650048.

35. Viljanen M, Savilahti E, Haahtela T, Juntunen-Backman K, Korpela R, Poussa T, et al. Probiotics in the treatment of atopic eczema/dermatitis syndrome in infants: a double-blind placebo-controlled trial. Allergy. 2005; 60(4):494–500. PMID:
15727582.

36. van der Aa LB, Heymans HS, van Aalderen WM, Sillevis Smitt JH, Knol J, Ben Amor K, et al. Effect of a new synbiotic mixture on atopic dermatitis in infants: a randomized-controlled trial. Clin Exp Allergy. 2010; 40(5):795–804. PMID:
20184604.

37. Grüber C, Wendt M, Sulser C, Lau S, Kulig M, Wahn U, et al. Randomized, placebo-controlled trial of
Lactobacillus rhamnosus GG as treatment of atopic dermatitis in infancy. Allergy. 2007; 62(11):1270–1276. PMID:
17919141.
38. Fölster-Holst R, Müller F, Schnopp N, Abeck D, Kreiselmaier I, Lenz T, et al. Prospective, randomized controlled trial on
Lactobacillus rhamnosus in infants with moderate to severe atopic dermatitis. Br J Dermatol. 2006; 155(6):1256–1261. PMID:
17107398.
39. Won TJ, Kim B, Lee Y, Bang JS, Oh ES, Yoo JS, et al. Therapeutic potential of
Lactobacillus plantarum CJLP133 for house-dust mite-induced dermatitis in NC/Nga mice. Cell Immunol. 2012; 277(1-2):49–57. PMID:
22726349.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download