1. Hueter C. Klnik der gelenkkrankheiten mit einschluss der orthopaedie: auf anatomisch-physiologischen grundlagen nach klinischen beobachtungen fr Arzte und studirende bearbeitet. Leipzig: Vogel;1870.
2. Huo MH, Parvizi J, Gilbert NF. What's new in hip arthroplasty. J Bone Joint Surg Am. 2006; 88(9):2100–2113. PMID:
16951129.

3. Meermans G, Konan S, Das R, Volpin A, Haddad FS. The direct anterior approach in total hip arthroplasty: a systematic review of the literature. Bone Joint J. 2017; 99-B(6):732–740. PMID:
28566391.
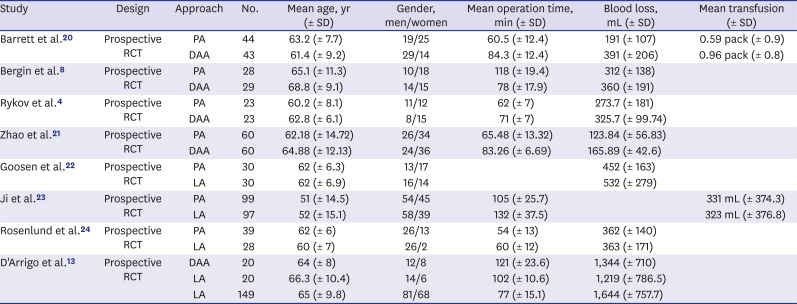
4. Rykov K, Reininga IH, Sietsma MS, Knobben BA, Ten Have BL. Posterolateral vs direct anterior approach in total hip arthroplasty (POLADA Trial): a randomized controlled trial to assess differences in serum markers. J Arthroplasty. 2017; 32(12):3652–3658.e1. PMID:
28780222.

5. Husted H, Jensen CM, Solgaard S, Kehlet H. Reduced length of stay following hip and knee arthroplasty in Denmark 2000–2009: from research to implementation. Arch Orthop Trauma Surg. 2012; 132(1):101–104. PMID:
21947286.

6. Woolson ST. In the absence of evidence--why bother? A literature review of minimally invasive total hip replacement surgery. Instr Course Lect. 2006; 55:189–193. PMID:
16958453.
7. Cheng T, Feng JG, Liu T, Zhang XL. Minimally invasive total hip arthroplasty: a systematic review. Int Orthop. 2009; 33(6):1473–1481. PMID:
19277652.

8. Bergin PF, Doppelt JD, Kephart CJ, Benke MT, Graeter JH, Holmes AS, et al. Comparison of minimally invasive direct anterior versus posterior total hip arthroplasty based on inflammation and muscle damage markers. J Bone Joint Surg Am. 2011; 93(15):1392–1398. PMID:
21915544.

9. Bremer AK, Kalberer F, Pfirrmann CW, Dora C. Soft-tissue changes in hip abductor muscles and tendons after total hip replacement: comparison between the direct anterior and the transgluteal approaches. J Bone Joint Surg Br. 2011; 93(7):886–889. PMID:
21705558.
10. Yoo JI, Cha YH, Kim KJ, Kim HY, Choy WS, Hwang SC. Gait analysis after total hip arthroplasty using direct anterior approach versus anterolateral approach: a systematic review and meta-analysis. BMC Musculoskelet Disord. 2019; 20(1):63. PMID:
30736783.

11. Mayr E, Nogler M, Benedetti MG, Kessler O, Reinthaler A, Krismer M, et al. A prospective randomized assessment of earlier functional recovery in THA patients treated by minimally invasive direct anterior approach: a gait analysis study. Clin Biomech (Bristol, Avon). 2009; 24(10):812–818.

12. Connolly KP, Kamath AF. Direct anterior total hip arthroplasty: Comparative outcomes and contemporary results. World J Orthop. 2016; 7(2):94–101. PMID:
26925380.

13. D'Arrigo C, Speranza A, Monaco E, Carcangiu A, Ferretti A. Learning curve in tissue sparing total hip replacement: comparison between different approaches. J Orthop Traumatol. 2009; 10(1):47–54. PMID:
19384637.
14. Yue C, Kang P, Pei F. Comparison of direct anterior and lateral approaches in total hip arthroplasty: a systematic review and meta-analysis (PRISMA). Medicine (Baltimore). 2015; 94(50):e2126. PMID:
26683920.
15. Hutton B, Salanti G, Caldwell DM, Chaimani A, Schmid CH, Cameron C, et al. The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: checklist and explanations. Ann Intern Med. 2015; 162(11):777–784. PMID:
26030634.

16. Beaudet K. The cochrane collaboration and meta-analysis of clinical data. Am Orthopt J. 2010; 60(1):6–8. PMID:
21061877.

17. Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003; 327(7414):557–560. PMID:
12958120.

18. Gleser LJ, Olkin I. Stochastically dependent effect sizes. In : Cooper H, Hedges LV, Valentine JC, editors. The Handbook of Research Synthesis and Meta-Analysis. 2nd ed. New York, NY: Russell Sage Foundation;2009. p. 357–376.
20. Barrett WP, Turner SE, Leopold JP. Prospective randomized study of direct anterior vs postero-lateral approach for total hip arthroplasty. J Arthroplasty. 2013; 28(9):1634–1638. PMID:
23523485.

21. Zhao HY, Kang PD, Xia YY, Shi XJ, Nie Y, Pei FX. Comparison of early functional recovery after total hip arthroplasty using a direct anterior or posterolateral approach: a randomized controlled trial. J Arthroplasty. 2017; 32(11):3421–3428. PMID:
28662957.

22. Goosen JH, Kollen BJ, Castelein RM, Kuipers BM, Verheyen CC. Minimally invasive versus classic procedures in total hip arthroplasty: a double-blind randomized controlled trial. Clin Orthop Relat Res. 2011; 469(1):200–208. PMID:
20352383.

23. Ji HM, Kim KC, Lee YK, Ha YC, Koo KH. Dislocation after total hip arthroplasty: a randomized clinical trial of a posterior approach and a modified lateral approach. J Arthroplasty. 2012; 27(3):378–385. PMID:
21802253.

24. Rosenlund S, Broeng L, Holsgaard-Larsen A, Jensen C, Overgaard S. Patient-reported outcome after total hip arthroplasty: comparison between lateral and posterior approach. Acta Orthop. 2017; 88(3):239–247. PMID:
28464754.

25. Amlie E, Havelin LI, Furnes O, Baste V, Nordsletten L, Hovik O, et al. Worse patient-reported outcome after lateral approach than after anterior and posterolateral approach in primary hip arthroplasty. A cross-sectional questionnaire study of 1,476 patients 1-3 years after surgery. Acta Orthop. 2014; 85(5):463–469. PMID:
24954494.
26. Wayne N, Stoewe R. Primary total hip arthroplasty: a comparison of the lateral Hardinge approach to an anterior mini-invasive approach. Orthop Rev (Pavia). 2009; 1(2):e27. PMID:
21808689.

27. Mardones R, Pagnano MW, Nemanich JP, Trousdale RT. The Frank Stinchfield Award: muscle damage after total hip arthroplasty done with the two-incision and mini-posterior techniques. Clin Orthop Relat Res. 2005; 441(441):63–67. PMID:
16330985.

28. Meneghini RM, Pagnano MW, Trousdale RT, Hozack WJ. Muscle damage during MIS total hip arthroplasty: Smith-Petersen versus posterior approach. Clin Orthop Relat Res. 2006; 453(453):293–298. PMID:
17006366.
29. van Oldenrijk J, Hoogland PV, Tuijthof GJ, Corveleijn R, Noordenbos TW, Schafroth MU. Soft tissue damage after minimally invasive THA. Acta Orthop. 2010; 81(6):696–702. PMID:
21110702.

30. Frye BM, Berend KR, Lombardi AV Jr, Morris MJ, Adams JB. Do sex and BMI predict or does stem design prevent muscle damage in anterior supine minimally invasive THA? Clin Orthop Relat Res. 2015; 473(2):632–638. PMID:
25337974.

31. Ogonda L, Wilson R, Archbold P, Lawlor M, Humphreys P, O'Brien S, et al. A minimal-incision technique in total hip arthroplasty does not improve early postoperative outcomes. A prospective, randomized, controlled trial. J Bone Joint Surg Am. 2005; 87(4):701–710. PMID:
15805196.
32. Bhandari M, Matta JM, Dodgin D, Clark C, Kregor P, Bradley G, et al. Outcomes following the single-incision anterior approach to total hip arthroplasty: a multicenter observational study. Orthop Clin North Am. 2009; 40(3):329–342. PMID:
19576400.
33. Alecci V, Valente M, Crucil M, Minerva M, Pellegrino CM, Sabbadini DD. Comparison of primary total hip replacements performed with a direct anterior approach versus the standard lateral approach: perioperative findings. J Orthop Traumatol. 2011; 12(3):123–129. PMID:
21748384.

34. Oinuma K, Eingartner C, Saito Y, Shiratsuchi H. Total hip arthroplasty by a minimally invasive, direct anterior approach. Oper Orthop Traumatol. 2007; 19(3):310–326. PMID:
17728988.
35. Spaans AJ, van den Hout JA, Bolder SB. High complication rate in the early experience of minimally invasive total hip arthroplasty by the direct anterior approach. Acta Orthop. 2012; 83(4):342–346. PMID:
22880711.

36. Woolson ST, Pouliot MA, Huddleston JI. Primary total hip arthroplasty using an anterior approach and a fracture table: short-term results from a community hospital. J Arthroplasty. 2009; 24(7):999–1005. PMID:
19493651.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download