INTRODUCTION
Since Jatene et al.
1) reported two cases of anatomical correction for transposition of the great arteries (TGA), the arterial switch operation (ASO) has been the gold standard for its surgical correction.
2) A recent report considering the factors affecting the outcomes of ASO, including age at ASO, prematurity, the timing of balloon atrial septostomy, and meticulous perioperative care,
2) showed that the perioperative mortality of ASO was 2.2%.
3) Despite this, residual problems associated with a risk of reoperation have been increasingly recognized, such as right ventricular outflow tract obstruction,
4) coronary artery problems,
4)5) neo-aortic regurgitation (neo-AR),
5)6)7)8)9)10)11) and neo-aortic root dilatation (ARD) and neo-aortic annulus dilatation (AAD).
6)7)8)9)10)11)12)13) In particular, many studies have reported findings of ARD and AAD after ASO,
6)7)8)9)10)11)12)13)14)15) which may subsequently result in neo-aortic root replacement. However, the growth pattern of neo-aortic root has not been established, as there has been no multivariable analysis of the trend in z-scores of the neo-aortic root and annulus over time. The purpose of the present study is to identify the growth pattern of the neo-aortic structure after ASO, its associated factors using a multivariable random coefficients model, and predictors of ARD and AAD after ASO.
METHODS
This was a retrospective study conducted at Seoul Asan Medical Center, a single tertiary referral center in South Korea. We identified all patients who underwent ASO for TGA (with or without other structural anomalies) from 2006 to 2015. Patients with follow-up for less than 2 years were excluded. Medical records were reviewed to obtain the information on demographics as well as morphological and surgical details. This study was approved by the institutional review board of Asan Medical Center (approval number: 2019-1189), and the requirement for informed consent was waived owing to the retrospective nature of the study.
All echocardiographic records of the subjects were reviewed retrospectively by a single observer. A total of 909 echocardiograms were reviewed. Echocardiographic images were analyzed using TomTec software (Image Arena VA version 4.6; TomTec Imaging Systems, Unterschleißheim, Germany). If there was no recorded echocardiographic image, we did not include the relevant echocardiographic data in the retrospective review. Available images that had good quality were assessed before ASO until the latest follow-up.
The maximal systolic dimension of the neo-aorta was measured at the sinus of Valsalva (neo-aortic root), at the level of the valve hinge points (neo-aortic annulus), and the ridge between the sinus of Valsalva and ascending aorta (the neo-aortic sinotubular junction [STJ]). For the measurement of the neo-aortic dimension, the 2-dimensional parasternal long-axis view was used. However, if the parasternal long-axis view was inadequate, the subxiphoid view was used. The body surface area was calculated using Haycock's formula. Z-scores of the neo-aortic annulus and root (sinus of Valsalva) were derived based on the data of Cantinotti et al.
16) We calculated the z-scores of the pre-ASO native pulmonary artery annulus and sinus using the criteria of aortic annulus and root z-scores. The grade (0 to IV) of neo-AR was subjectively assessed using the length and width of the color Doppler jet of regurgitant flow using parasternal long-axis and apical 5-chamber views.
Significant ARD was defined as a neo-aortic sinus of Valsalva z-score of 2.5 or higher, while AAD and neo-aortic STJ dilatation were defined as a neo-aortic annulus and STJ z-score of 2.5 or higher. Significant neo-AR was defined as grade II or more. Aorto-pulmonary diameter mismatch was defined as native pulmonary valve annulus (mm)/native aortic valve annulus (mm) >1.5.
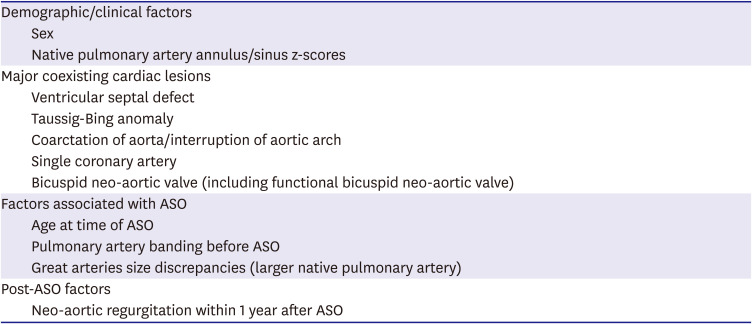
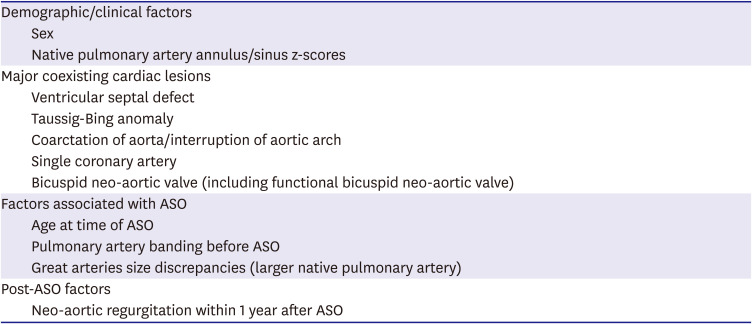
17) We selected potential risk factors from the literature for ARD and AAD, as listed in
Table 1.
Table 1
Potential risk factors for neo-aortic root and annulus dilatation after arterial switch operation in the present study
|
Demographic/clinical factors |
|
Sex |
|
Native pulmonary artery annulus/sinus z-scores |
|
Major coexisting cardiac lesions |
|
Ventricular septal defect |
|
Taussig-Bing anomaly |
|
Coarctation of aorta/interruption of aortic arch |
|
Single coronary artery |
|
Bicuspid neo-aortic valve (including functional bicuspid neo-aortic valve) |
|
Factors associated with ASO |
|
Age at time of ASO |
|
Pulmonary artery banding before ASO |
|
Great arteries size discrepancies (larger native pulmonary artery) |
|
Post-ASO factors |
|
Neo-aortic regurgitation within 1 year after ASO |

Demographic data were expressed as median with minimum and maximum values in parentheses, and statistical data were expressed as mean±standard deviation. To analyze repeated measures of the neo-aorta z-score and STJ/annulus ratio, a random coefficients model was used to confirm changes over time. To control for correlation among repeated measures from the same individual, the random coefficients model included time (at each measures), each variable, and the interactions between time and each variable as fixed effects and individual (random intercepts) and the interaction between individual and time (random slopes) as random effects to control for the correlation among repeated measures from same individual. Kaplan-Meier analysis was used to assess the probabilities that were independent of ARD, AAD, and neo-aortic STJ dilatation over time. The Cox proportional hazards model was used to identify risk factors associated with the development of ARD, AAD, and neo-aortic STJ dilatation. In the random coefficients and Cox proportional hazards model, univariate analysis identified the variables with p value <0.06, which were then entered in a stepwise fashion into a multivariable analysis. The interaction between time and variable was presented as time*variable in a random coefficients model. In this model, the effect of time (estimate value) implied the slope of the time-z-score graph, the estimated value of each variable (group) meant the difference of intercepts (individuals), and interaction with time was shown by the difference of the time effect (slope of the time-z-score graph) between groups. The hazard ratio (HR) and 95% confidence interval (CI) were presented for Cox proportional hazards model. Two-tailed probability values (p value) <0.05 were considered statistically significant.
RESULTS
In total, 163 patients who underwent ASO at our center were included in this study. Of them, 129 were male. Echocardiogram after ASO was performed 5.6 times per patient (range, 3–12). The median age at operation was 7 days and the median body weight at operation was 3.25 kg. The median postoperative follow-up duration was 6.61 years (range, 2.51–13.49).
Of the 163 patients, 111 (68.1%) were diagnosed as having TGA with intact ventricular septum (including restrictive ventricular septal defect), 41 (25.1%) had TGA with ventricular septal defect (VSD), and 11 (6.7%) had Taussig-Bing (TB) anomaly. Before ASO, 94 patients underwent balloon atrial septostomy, and 4 underwent pulmonary artery banding (PAB) with or without shunt. In ASO, the trapdoor technique was used for coronary artery transfer in 148 (91.9%) patients, the non-trapdoor technique was used for coronary artery transfer in the remaining 13 (8.1%) patients (simple button in 10 patients and button and trapdoor in each coronary artery in 3 patients). The Lecompte maneuver was used in all patients. The detailed demographic and clinical characteristics are presented in
Table 2. Ten patients showed grade II or more neo-AR throughout follow-up and four patients presented grade II or more neo-AR within one year after ASO. During follow-up, ARD, AAD, and neo-aortic STJ dilatation developed in 97 (59.5%), 68 (41.7%), and 42 (25.8%) patients, respectively.
Table 2
Demographic and clinical characteristics of patients

|
Variables |
Values |
|
Patients characteristic |
(n=163) |
|
Sex |
|
|
|
Male |
129 (79.1) |
|
|
Female |
34 (20.9) |
|
Median Age at time of ASO (days) |
7 (0 to 361) |
|
Median body weight at time of ASO (kg) |
3.25 (1.44 to 7.20) |
|
Median postoperative follow-up duration (years) |
6.61 (2.51 to 13.49) |
|
Diagnosis |
(n=163) |
|
TGA with IVS |
111 (68.1) |
|
TGA with VSD |
41 (25.1) |
|
Taussig-Bing anomaly |
11 (6.7) |
|
Major coexisting cardiac lesions |
(n=163) |
|
VSD |
52 (31.9) |
|
Aortic arch anomaly |
18 (11.0) |
|
Bicuspid neo-aortic valve |
6 (3.7) |
|
Initial echocardiogram parameters |
|
|
Median native PA annulus z-score |
2.09 (−3.82 to 8.36) |
|
Median native PA sinus z-score |
0.77 (−4.46 to 4.37) |
|
Coronary artery |
(n=163) |
|
Usual pattern (1L, Cx; 2R) |
119 (73.0) |
|
LCx from RCA (1L; 2R, Cx) |
17 (10.4) |
|
RCA from LAD, isolated LCx (1L, R; 2Cx) |
3 (1.8) |
|
Inverted pattern (1R; 2L, Cx) |
4 (2.5) |
|
High take-off LCA |
1 (0.6) |
|
Single LCA (1L, Cx, R) |
3 (1.8) |
|
Single RCA (2L, Cx, R) |
16 (9.8) |
|
Intramural course |
3 (1.8) |
|
Great arteries size discrepancies |
(n=163) |
|
PA/Ao >1.5 |
16 (9.8) |
|
Previous intervention before ASO |
(n=163) |
|
Balloon atrial septostomy |
94 (57.7) |
|
Pulmonary artery banding |
4 (2.5) |
|
Coronary artery transfer technique |
(n=161) |
|
Trapdoor (including trapdoor for single coronary artery) |
148 (91.9) |
|
Non-trapdoor |
13 (8.1) |
|
|
Button |
10 (6.2) |
|
|
Combined (trapdoor and button in each coronary artery) |
3 (1.9) |
|
Lecompte maneuver |
161 (100.0) |

The random coefficients model for repeated measures of neo-aortic root z-scores showed that PAB prior to ASO and the coronary transfer artery technique had an interaction with time (
Supplementary Table 1). Since PAB was performed in only 4 patients, we only selected the non-trapdoor technique as a factor that interacted with time in the model for neo-aortic root z-scores. Univariate analysis, except interaction with time to determine the other independent variables for multivariate analysis is presented in
Supplementary Table 2. In the multivariate model, the neo-aortic root z-scores increased at a rate of 0.149/year in the trapdoor technique (p<0.001) and 0.311/year in the non-trapdoor technique (
Figure 1A and
Supplementary Table 3). The increase in neo-aortic root z-scores was significantly different (p=0.005) between the trapdoor and non-trapdoor groups (
Figure 1A and
Supplementary Table 3). In addition, VSD, TB anomaly, aortic arch anomaly, native pulmonary artery/aorta (PA/Ao) >1.5, and significant AR within 1 year did not influence change of neo-aortic root z-score over time.
Figure 1
Post-ASO change of neo-aorta z-scores and STJ/annulus ratio in TGA using multivariate random coefficients model.
Neo-aortic root z-scores increased over time after ASO at a rate of 0.149/year in the trapdoor group and 0.311/year in the non-trapdoor group (A). Neo-aortic annulus and STJ z-scores increased over time at a rate of 0.067/year (B) and 0.309/year (C) respectively. The STJ/annulus ratio also increased over time after ASO (0.021/year) (D). The interaction between PAB prior to ASO and time was excluded in multivariate random coefficients model for neo-aortic root and annulus z-scores because the number of patients in the PAB group was significantly small (n=4).
ASO = arterial switch operation; PAB = pulmonary artery banding; STJ = sinotubular junction; TGA = transposition of the great arteries.


In the random coefficients model for repeated measures of neo-aortic annulus z-scores, PAB prior to ASO had an interaction with time (
Supplementary Table 1); we excluded this interaction from the multivariate model because the number of patients in the PAB group was small. Finally, neo-aortic annulus z-scores increased at a rate of 0.067/year (p<0.001) (
Figure 1B and
Supplementary Table 3), which was significantly slower than the increase in neo-aortic root z-scores. In the random coefficients model for neo-aortic STJ z-scores and the STJ/annulus ratio, no factor interacted with time (
Supplementary Table 1). In the multivariate random coefficients model, the STJ z-score and STJ/annulus ratio increased at the rate of 0.309/year (p<0.001) and 0.021/year (p<0.001), respectively (
Figure 1C and D,
Supplementary Table 3).Kaplan-Meier analysis revealed that the probabilities of freedom from ARD at 1, 5, and 10 years after ASO were 69.3%, 46.0%, and 33.4%, respectively, while those from AAD and STJ dilatation were 76.7%, 60.3%, and 53.9% and 94.5%, 78.1%, and 65.4%, respectively (
Figure 2). The probabilities of freedom from neo-aortic structure dilatation were significantly different (p<0.001).
Figure 2
Kaplan-Meier graph for probabilities of freedom from ARD, AAD, and neo-aortic STJ dilatation.
The probabilities of freedom from ARD (dotted line) at 1, 5, and 10 years after operation were 69.3%, 46.0%, and 33.4% and the probabilities of freedom from AAD (line) and neo-aortic STJ dilatation (large dotted line) at 1, 5, and 10 years after operation were 76.7%, 60.3%, and 53.9% and 94.5%, 78.1%, and 65.4%, respectively. The probabilities of freedom from neo-aortic structure dilatation are significantly different.
AAD = neo-aortic annulus dilatation; ARD = neo-aortic root dilatation; ASO = arterial switch operation; post-Op = postoperative; STJ = sinotubular junction.


In a multivariate analysis using the Cox proportional hazards model, the risk factors identified as predictors of ARD were TB anomaly (HR, 2.329; 95% CI, 1.069–5.076; p=0.033), PAB (HR, 6.717; 95% CI, 2.185–20.656; p=0.001), native pulmonary artery sinus z-score (HR, 1.203; 95% CI, 1.030–1.404; p
=0.019), and neo-AR within 1 year after ASO (HR, 3.067; 95% CI, 1.043–9.022; p=0.042) (
Table 3). However, only 4 patients underwent PAB, and 4 patients had developed neo-AR within 1 year postoperatively. The risk factors for development of AAD were native pulmonary artery annulus z-score (HR, 1.211; 95% CI, 1.044–1.404; p=0.012) and neo-AR within 1 year (HR, 5.112; 95% CI, 1.625–16.082; p=0.005) (
Table 3). The predictors of neo-aortic STJ dilatation were PAB (HR, 4.868; 95% CI, 1.448–16.372; p=0.011), neo-AR within 1 year (HR, 6.879; 95% CI, 2.046–23.132; p=0.002), and non-trapdoor technique (HR, 2.520; 95% CI, 1.062–5.980; p= 0.036) (
Table 3). Three patients underwent neo-aortic valve replacement without root plasty during follow-up and only 1 patient underwent neo-aortic root reduction surgery concomitant with right ventricular outflow tract relief because of ARD and right ventricular outflow tract obstruction 1.6 months after ASO.
Table 3
Cox regression analysis for AAD, ARD, and STJ dilatation

|
AAD |
ARD |
Neo-aortic STJ dilatation |
|
HR (95% CI) |
p value |
HR (95% CI) |
p value |
HR (95% CI) |
p value |
|
Univariate |
|
|
|
|
|
|
|
Female |
0.691 (0.369–1.294) |
0.248 |
0.651 (0.380–1.117) |
0.119 |
0.571 (0.239–1.362) |
0.207 |
|
VSD |
1.881 (1.159–3.053) |
0.011 |
1.608 (1.063–2.434) |
0.025 |
1.381 (0.740–2.576) |
0.311 |
|
TB anomaly |
4.057 (1.992–8.264) |
<0.001 |
4.628 (2.417–8.861) |
<0.001 |
2.627 (1.028–6.708) |
0.044 |
|
CoA/IAA |
3.100 (1.711–5.616) |
<0.001 |
1.733 (0.965–3.113) |
0.066 |
1.833 (0.814–4.130) |
0.144 |
|
ASO after 7 days |
1.705 (1.017–2.856) |
0.043 |
1.652 (1.081–2.525) |
0.020 |
1.717 (0.890–3.313) |
0.107 |
|
Pre-ASO PAB |
1.262 (0.306–5.196) |
0.747 |
10.241 (3.592–29.199) |
<0.001 |
4.264 (1.293–14.065) |
0.017 |
|
Single CA |
1.146 (0.547–2.400) |
0.719 |
0.863 (0.448–1.664) |
0.661 |
0.619 (0.191–2.088) |
0.425 |
|
BAV |
0.726 (0.178–2.967) |
0.655 |
1.188 (0.436–3.238) |
0.737 |
2.923 (0.895–9.542) |
0.076 |
|
Native PA/Ao >1.5 |
2.503 (1.304–4.805) |
0.006 |
1.785 (0.950–3.353) |
0.072 |
1.098 (0.394–3.080) |
0.859 |
|
Native PA structure z-score |
1.244 (1.110–1.393) |
<0.001 |
1.288 (1.113–1.489) |
0.001 |
1.184 (0.989–1.418) |
0.066 |
|
Neo-AR within 1 year |
9.250 (3.226–26.525) |
<0.001 |
5.125 (1.826–14.383) |
0.002 |
6.681 (2.025–22.046) |
0.002 |
|
Non-trap door Technique |
1.436 (0.656–3.147) |
0.365 |
1.772 (0.917–3.424) |
0.089 |
2.645 (1.174–5.962) |
0.019 |
|
Multivariate |
|
|
|
|
|
|
|
VSD |
1.017 (0.523–1.976) |
0.961 |
1.062 (0.620–1.818) |
0.828 |
- |
- |
|
TB anomaly |
1.789 (0.711–4.500) |
0.217 |
2.329 (1.069–5.076) |
0.033 |
1.871 (0.690–5.080) |
0.219 |
|
CoA/IAA |
1.759 (0.716–4.318) |
0.218 |
- |
- |
- |
- |
|
ASO after 7 days |
1.372 (0.783–2.403) |
0.291 |
1.364 (0.821–2.266) |
0.230 |
- |
- |
|
Pre-ASO PAB |
- |
- |
6.717 (2.185–20.656) |
0.001 |
4.868 (1.448–16.372) |
0.011 |
|
Native PA/Ao >1.5 |
0.557 (0.199–1.558) |
0.264 |
- |
- |
- |
- |
|
Native PA structure z-score |
1.211 (1.044–1.404) |
0.012 |
1.203 (1.030–1.404) |
0.019 |
- |
- |
|
Neo-AR within 1 year |
5.112 (1.625–16.082) |
0.005 |
3.067 (1.043–9.022) |
0.042 |
6.879 (2.046–23.132) |
0.002 |
|
Non-trap door Technique |
- |
- |
- |
- |
2.520 (1.062–5.980) |
0.036 |

DISCUSSION
In the present study, we showed that the growth of the neo-aorta after ASO is greater than somatic growth during childhood. In our study, the multivariate random coefficients model showed that the growth pattern of the neo-aortic root z-score was affected by the coronary artery transfer technique. A significant increase in neo-aortic z-scores was observed in the non-trapdoor group compared to the trapdoor group. PAB prior to ASO also affected the growth pattern of neo-aortic root and annulus z-scores. However, we could not verify this association because the number of patients in the PAB group was significantly small. We have previously reported the superiority of the trapdoor technique in terms of neo-AR
18) compared to a previous report which mainly used traditional button technique.
19) The present study also suggested that this technique might be beneficial in neo-aortic root overgrowth after ASO. To our knowledge, this is the first study investigating the factors affecting their growth pattern.
There was scant literature to report the relation between coronary transfer technique and neo-aortic root growth pattern over time after ASO. Only 1 study from the Netherlands reported coronary transfer technique did not affect the neo-aortic growth with simple linear mixed model.
13)
Several studies analyzed the change in z-scores or indexed sizes of the neo-aortic structure after ASO. As for the change in z-score of the neo-aortic annulus, previous studies reported no significant change after ASO,
6)7)8)11)13) although 2 studies have reported an increase in neo-aortic STJ z-score during follow-up.
12)14) However, many studies reported that z-scores or indexed values of neo-aortic root after ASO increased over time,
6)7)8)11)13)14) even if a few reported no change.
12)15) Moreover, the reported growth patterns of neo-aortic root were not consistent across previous studies. One study reported an increase only until 10 years after ASO,
11) and another study reported that, after a rapid increase in the first year after ASO and proportional growth in childhood, neo-aortic dimensions continued to increase throughout adulthood without stabilization.
13)
Our study supports the idea that there is an increased progressive dilatation of the neo-aortic root that is disproportional to somatic growth in childhood. However, the rate of progression of the neo-aortic root z-score after ASO was as high as 0.149/year in the trapdoor group and 0.311/year in the non-trapdoor group, which is remarkably higher than that of the prior study (0.05/year).
11) Neo-aortic annulus and STJ z-scores were also increased over time at a rate of 0.067/year and 0.309/year, respectively. The mean neo-aortic STJ z-score initially decreased, which suggested a smaller STJ size than that observed in the normal population, but it increased significantly over time after ASO.
In this study, the predictors of change in neo-aortic root z-scores and neo-ARD were different. We assumed that patients who already showed neo-ARD immediately after ASO (probably, most patients had increased native pulmonary sinus z-scores even before ASO) caused this difference. More than one-third patients with neo-ARD already showed a neo-aortic root z-score of greater than 2.5 at the initial postoperative echocardiography, the beginning point of the random coefficients model. The z-score of several patients, especially patients with PAB, who already showed neo-ARD immediately after ASO did not significantly increase during post-ASO follow-up. Moreover, some patients who did not have TB anomaly or a history of PAB showed continuous increase in neo-aortic sinus z-scores, but their z-scores did not reach 2.5 until the time of study or follow-up loss. The discrepancies in the neo-aortic annulus and STJ were also explained in a similar manner. Thus, we presumed that the results from the random coefficients model mainly represented the influence of postoperative periods and most factors identified in the Cox proportional hazards model suggested native pulmonary dilatation in pre-ASO periods.
In our study, the previously reported factors, including male sex,
13) complex TGA anatomy,
13) bicuspid neo-aortic valve,
15) preoperative aorta-to-pulmonary artery ratio,
15) and early development of neo-AR,
15) were not related to the growth of neo-aortic root. However, early development of neo-AR, a previously reported risk factor for overgrowth
15) and a predictor of neo-ARD, neo-AAD, and neo-aortic STJ dilatation in the Cox regression analysis in this study, tended to interact with time in the random coefficients model for neo-aortic root z-scores, although this interaction was not significant (p=0.075). Only 4 patients developed more than grade 2 neo-AR within 1 year. Larger studies with more cases of neo-AR within 1 year and longer follow-up are needed to clarify the association between early onset of neo-AR and change in neo-aortic root z-scores.
History of PAB was a predictor of neo-ARD. At first glance, this looks like a contradiction compared with the affecting factor of the growth pattern of neo-aortic root and annulus over time. However, our analysis showed that this result was related to the large initial z-score of neo-aortic root in the PAB group. It is noted that ARD was observed from the first postoperative echocardiogram in the patients with PAB prior to ASO, although in this group the neo-aortic root grows in proportion to somatic growth. This finding was consistent with that reported by Sievers et al.
20) and Hourihan et al.
6) Sievers et al.
20) have reported that PAB may have a role in progressive native pulmonary root dilatation and growth potential of the neo-aortic root after ASO is normal. Hourihan and colleagues also reported that the native pulmonary artery root, which would later become the neo-aortic root, dilated even before ASO in patients who had a history of PAB in TGA, which probably resulted from increased wall tension proximal to the band.
6)
The risk factors for ARD in this study were similar to those demonstrated in the previous studies.
7)8)9)11) The risk factors for the development of AAD in previous studies have remained unclear. One study of 124 patients found that VSD and TB anomaly were the risk factors of AAD,
8) while another study of 39 young adult patients found that only neo-AR was a risk factor.
9) In our study, we found that native pulmonary annulus z-score and neo-AR within 1 year were the predictors of AAD by multivariate analysis. PAB prior to ASO was not a risk factor in previous studies
6)8) as well as in our study. It is unclear why the growth pattern was different between the native pulmonary annulus and sinus in patients who underwent PAB. Native pulmonary annulus before ASO could be enlarged in TB anomaly or VSD group because of the increased pulmonary flow. We suspect that native pulmonary annulus z-score is a more important predictor of development of AAD after ASO. Predictors for the development of neo-aortic STJ dilatation have not been well reported; one study reported that neo-aortic STJ dilatation was associated with the development of neo-AR.
18) In our study, PAB, early onset of neo-AR, and coronary artery transfer technique were predictors for the development of neo-aortic STJ dilatation.
The last topic to be addressed is whether neo-aortic dilatation is serious enough to require neo-aortic root surgery in patients with ASO. Schwartz et al.
11) reported that there was no significant change in neo-aortic root z-scores 10 years after ASO, and this suggests that ARD, AAD, and STJ dilatation were tolerable and may not be associated with acute aortic dissection or increased mortality.
11)21) Nevertheless, more recent studies including ours reported no evidence of stabilization of neo-aortic root size at 15–20 years postoperatively,
8) and the aortic root and annulus even continuously grew in adulthood.
13) van der Palen et al.
13) reported that 3% of patients with d-TGA after ASO underwent the operation because of ARD with or without neo-AR with a median follow-up of 12 years. These findings suggest that patients who undergo ASO for TGA need more meticulous examination of the neo-aortic root and annulus in echocardiography and follow-up, because they could be at high risk for aortic root surgery in adulthood.
This is a retrospective study, and the follow-up echocardiograms were incomplete. The post-operative follow-up period was somewhat shorter than recent studies of the growth of neo-aorta after ASO.
13) Some independent factors, such as PAB and early onset of neo-AR, were present in a significantly small number of patients (4 patients each). Thus, we had to exclude PAB in the multivariate random coefficient model, although PAB had an interaction with time. Co-Vu et al.
8) pointed that medications or blood pressure might also potentially affect the measurements during serial evaluations. In the present study, there was no consideration of medication or blood pressure.
In conclusion, the growth of neo-aortic root, annulus, and STJ after ASO was greater compared to somatic growth during childhood. The data analysis, based on the multivariate random coefficients model, showed that the coronary artery transfer technique affects the growth pattern of the neo-aortic root and some of the known risk factors (VSD, TB anomaly, arch anomaly, native PA/Ao >1.5, and significant AR within 1 year) of ARD did not affect the change of the neo-aortic root z-score over time. PAB before ASO, which is another known risk factor, had the effect of alleviating the change of the neo-aortic root and annulus z-score over time after ASO. We conclude that, despite the absence of previously known risk factors of ARD, the patients who underwent ASO are still at high risk of ARD and may need aortic root surgery in adulthood, and thus require strict vigilance.








 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download