INTRODUCTION
Restoring discolored tooth structures, especially in the anterior area, is challenging for most clinicians. In restorative dentistry, achieving a natural tooth-like restoration is an important factor influencing patients' satisfaction and treatment success [
1]. Over the last few decades, the increased demand of patients for highly esthetic restorations (natural-looking restorations) has resulted in the development of all-ceramic restorations. Their popularity is attributed to their superior esthetic properties, biocompatibility, and longevity, as well as the conservative nature of the procedure [
2]; however, all-ceramic restorations are brittle. Advancements have been made to reinforce these materials with crystalline phases to improve their physical and mechanical properties [
3].
Lithium disilicate glass ceramics, such as the IPS e.max Press, have generated considerable interest. The addition of 70% lithium disilicate crystals as the crystalline phase results in adequate flexural strength (350–450 MPa), better integration with the tooth structure through the bonding mechanism, and superior esthetic properties. It is recommended to be used with anatomical contouring as a monolithic restoration due to its translucency and the availability of various shades [
3].
The esthetic appearance of ceramic restorations is influenced by several factors, such as the thickness and translucency of the ceramic [
4], the luting agent [
5], the color of the underlying tooth structure [
4], and the type of ceramic [
6]. The thickness of the ceramic material is an important factor for successful shade reproduction.
In clinical circumstances, the thickness of the dentin and the enamel differs among individuals; therefore, the fabrication of a ceramic restoration similar to a natural tooth depends on the combination of core and veneer thicknesses, which have been reported to influence the final color of the ceramic restoration [
78].
The translucency of the ceramic, which has been emphasized as another factor relevant for maintaining good esthetics, is significantly influenced by the type of material and its thickness [
9]. Translucency is defined as the extent to which light is diffused in a material that partially allows light transmittance in response to irradiance, and attention should be paid to this parameter. Translucency of a ceramic means that the underlying substrate has a significant influence on the final color [
10].
The Commission Internationale de l’Eclairage (CIE) L*a*b* color system is widely used to evaluate differences in color between dental restorations and teeth because of its validity, feasibility, and simplicity. The CIEL*a*b* system evaluates the degree of perceptible color change based on 3 parameters: L* (lightness, in which 100 represents white and 0 represents black), a* (red–green chromatic coordinate) and b* (blue–yellow chromatic coordinate). ΔE is the total color change and a value of 3.3 or more is considered to be clinically unacceptable [
11]. The aim of this
in vitro study was to evaluate the ability of lithium disilicate ceramics to reproduce the A2 shade and to mask A4 substrates.
MATERIALS AND METHODS
Twenty-four disks were fabricated from a lithium disilicate ceramic (IPS e.max Press, shade A2; Ivoclar Vivadent AG, Schaan, Liechtenstein), including 9 monolayer discs with high translucency (HT) at thicknesses of 0.5, 0.7, and 1 mm (groups 1–3), 9 monolayer discs with low translucency (LT) at thicknesses of 0.5, 0.7, and 1 mm (groups 4–6), and 6 bilayer discs with medium opacity (MO) at a thickness of 1 mm in 2 combinations (0.3-mm core; 0.7-mm veneer) and (0.5-mm core; 0.5-mm veneer) (groups 7–8). The group description is presented in
Table 1.
Table 1
Descriptive analysis and Tukey post hoc comparisons of ΔE values of the study groups in comparison to the A4 substrate and the A2 VITA shade tab (n = 3)

|
Group |
Translucency |
Thickness |
Structure |
A4 substrate |
A2 VITA shade tab |
|
Mean ± SD |
Mean ± SD |
|
1 |
HT |
0.5 mm |
Monolayer |
8.98 ± 0.53 |
3.31 ± 0.27A
|
|
2 |
HT |
0.7 mm |
Monolayer |
8.20 ± 0.10a
|
3.69 ± 015B
|
|
3 |
HT |
1 mm |
Monolayer |
8.12 ± 0.29b
|
4.88 ± 0.19ABC
|
|
4 |
LT |
0.5 mm |
Monolayer |
9.96 ± 0.25abc
|
1.09 ± 0.10ABCD
|
|
5 |
LT |
0.7 mm |
Monolayer |
8.63 ± 0.49 |
0.76 ± 0.04ABCEF
|
|
6 |
LT |
1 mm |
Monolayer |
8.12 ± 0.84c
|
1.38 ± 0.30ABCF
|
|
7 |
MO |
0.3 mm core/0.7 mm veneer |
Bilayer |
9.45 ± 0.69 |
2.93 ± 0.18BCDEF
|
|
8 |
MO |
0.5 mm core/0.5 mm veneer |
Bilayer |
8.62 ± 0.39c
|
3.29 ± 0.12CDEF
|
Preparation of specimen
The specimens were fabricated using the lost wax and heat-pressed techniques. To fabricate the monolayer specimens (groups 1–6), discs of A2 shade of HT and LT ceramics were used. The wax patterns were invested with a proprietary IPS e.max Press powder (IPS e.max Press powder and liquid; Ivocolar Vivadent AG), and pressed using a Programat EP 3000 furnace (Ivoclar Vivadent AG). The pressed disc was then bench-cooled and subsequently divested. The specimens were treated with 1% hydrofluoric acid IPS ceramic etching gel (1% hydrofluoric acid, Ivoclar Vivadent AG) for 60 seconds, followed by rinsing and air drying.
For the fabrication of bilayer specimens (groups 7–8), MO ceramic discs with the A2 shade were used. The first layer was pressed in 2 thicknesses (0.3 or 0.5 mm) in the same way described for LT and HT groups. The ceramic discs were then covered with veneering ceramic IPS e.max Ceram (color A2). The firing and layering procedures proceeded according to the manufacturer's instructions, and the final thickness of each specimen was adjusted to 1 mm.
The specimens were polished with 250-, 400-, and 600-grit silicon carbide abrasive papers under running water. The accuracy of the final thickness was verified to be within 0.05 mm using a digital caliper (Mitutoyo Corp, Kawasaki, Japan) (accuracy of 0.01 mm). A thin layer of glaze material was applied to 1 side of each specimen, and glaze firing was performed at 403°C for 1 minute, followed by drying for 6 minutes. The temperature was then raised to 770°C and the specimens were kept under vacuum for 1.5 minutes. All specimens were cleaned with distilled water, air-dried, and stored in separate screw-top vials at room temperature before color measurements.
For the control CIE L*a*b* measurements, an A2 shade tab (VITA classical A1-D4 shade guide; VITA Zahnfabrik, Bad Säckingen, Germany) was selected for a shade guide. The CIE L*a*b* values of this shade tab were calculated at the center of its middle third using the method described below (L* = 74.8, a* = 0.7, b* = 20.0).
Preparation of substrate
Dark dentin substrate was simulated with a 4-mm-thick IPS e.max Press ceramic (8 mm in diameter, shade A4) according to the manufacturer's instructions.
Color measurements
The CIE L*a*b* color coordinates were measured with a reflectance spectrometer (SP60, X-Rite, Grand Rapids, MI, USA) equipped with a standard D-65 illuminant. The equipment was calibrated using the standards provided before each measurement. Two readings were performed at locations close to the center of each disc and the mean was calculated. During the measurements, the ceramic discs were superimposed on the A4 substrate, and the resultant complex was positioned on a black background.
The ΔE (total color change) was obtained by comparing the complex with either the A4 substrate or an A2 shade tab using the following formula: ΔE = [(ΔL)2 + (Δa)2+ (Δb)2]1/2
Data analysis
The data were statistically analyzed using SPSS version 16 software (SPSS Inc., Chicago, IL, USA). One-way analysis of variance (ANOVA) was used to determine the significance of differences in color among different groups. Multiple comparisons were performed using the post hoc Tukey honest significant difference test. The Fisher test was used to evaluate color differences using thresholds for imperceptible (ΔE < 1.0), perceptible (1.0 < ΔE < 3.3), and clinically unacceptable (ΔE > 3.3) differences. The level of statistical significance was set at p < 0.05.
RESULTS
Table 1 presents the mean and standard deviation of ΔE values of different groups in comparison to the A4 substrate and the A2 VITA shade tab. When the complex was compared to the A4 substrate, 1-way ANOVA revealed significant differences among all groups (
p < 0.05); however, the ΔE values were in the non- acceptable range. The lowest and highest values of ΔE were found in group 3 (8.12 ± 0.29) and group 4 (9.96 ± 0.25), respectively. Pairwise comparisons are shown in
Table 1.
When the complex was compared to the A2 shade tab, 1-way ANOVA revealed significant differences among all groups (
p < 0.05) except for groups 2 (3.69 ± 0.15) and 3 (4.88 ± 0.19); moreover, the ΔE values were in the clinically acceptable range. The lowest and highest values of ΔE were found in group 5 (0.76 ± 0.04) and group 3 (4.88 ± 0.19), respectively. Pairwise comparisons are shown in
Table 1.
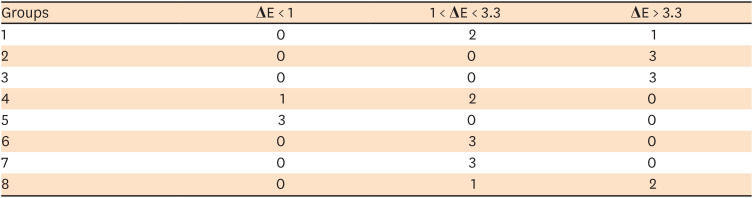
To describe the ΔE values of the study groups according to the thresholds for imperceptibility, perceptibility, and acceptability, the mean ΔE values of the specimens were tested (
Table 2). In groups 1 and 4, most of the specimens (
n = 2, respectively) showed acceptable differences. In groups 2 and 3, all specimens showed perceptible differences. In group 5, all specimens showed imperceptible differences. In groups 6 and 7, all specimens showed acceptable differences. In group 8, most of the specimens showed imperceptible differences.
Table 2
ΔE values of the study groups according to imperceptibility, perceptibility, and acceptability thresholds
|
Groups |
ΔE < 1 |
1 < ΔE < 3.3 |
ΔE > 3.3 |
|
1 |
0 |
2 |
1 |
|
2 |
0 |
0 |
3 |
|
3 |
0 |
0 |
3 |
|
4 |
1 |
2 |
0 |
|
5 |
3 |
0 |
0 |
|
6 |
0 |
3 |
0 |
|
7 |
0 |
3 |
0 |
|
8 |
0 |
1 |
2 |
DISCUSSION
Restoring discolored tooth structures, especially in the anterior region, is a challenge for dental clinicians. The choice of dental ceramic materials is an important factor contributing to the final color, and lithium disilicate glass-ceramics have a needle-like crystal structure that offers excellent appropriate optical properties. Many studies have reported that the masking ability and shade reproduction of ceramics can be affected by factors such as thickness and translucency. Thus, in the current study, the ability of lithium disilicate ceramics to reproduce the A2 shade and to mask A4 substrates was evaluated. Different combinations of thickness and translucency affected the ability of ceramic restorations to mask A4 substrates and to reproduce the A2 shade tab.
The current study simulated a clinical situation, since ceramics can vary in thickness and translucency in clinical settings. It is well known that clinical shade matches are difficult to achieve, especially on a dark substructure. Thus, the A4 substrate was used as background to simulate the underlying dark tooth structure.
To interpret the results for color differences, a ΔE reference threshold is necessary. In light of differences among individuals in terms of the ability to recognize color differences, the following intervals have been suggested: ΔE < 1, undetectable by the human eye; 1 < ΔE < 3.3, detectable by expert individuals but clinically acceptable; and ΔE > 3.3, detectable by patients and unskilled observers and clinically unacceptable [
12]. Accordingly, the present study used the acceptability threshold of ΔE = 3.3 to evaluate color differences and found that, in this respect, the minimum ceramic thickness needed to reproduce the A2 shade was 0.5 mm. In addition, the ceramic thickness needed to mask the underlying structure ranged from 0.5 to 1 mm.
Based on the manufacturer's claims, a high opaque (HO) ceramic with a thickness of 1.2 mm is capable of masking the silver color of amalgam. The results of the present study showed that all evaluated ceramic groups showed acceptable values for masking a simulated tooth with a discolored A4 substrate (ΔE > 3.3). Therefore, for dark dentin substrates, the clinicians could be advised to use any of the investigated combinations to mask the underlying structure.
Translucent ceramics are more commonly used to fabricate anterior restorations than opaque ceramics. In the present study, IPS e.max Press ceramic ingots with different degrees of translucency (
i.e., HT, LT, and MO) were used. We found that all the tested ingots at different thicknesses (0.5, 0.7, and 1 mm) were capable of masking the underlying A4 substrate. In other words, the substrate was similarly affected by the HT and LT materials, which aligns with the study by Dede
et al. [
13]. In contrast, Skyllouriotis
et al. [
14], Basso
et al. [
15], and Pires
et al. [
6] reported that LT lithium disilicate materials showed better masking ability than HT ceramics. The difference between these studies and the current experiment can be attributed to this fact that all translucency values were statistically compared using a dark substrate, but translucency was not statistically evaluated as a dependent variable.
The optical properties of various components of veneering materials, along with their thickness, appear to be the main factors shaping the ability of ceramics to mask underlying tooth structures [
16]. However, increasing the thickness of a material that does not have an opacifier in its composition does not lead to a significant difference in its masking ability. Of note, the LT and HT ceramics are the most translucent IPS e.max materials, and the manufacturer does not provide additional information about the composition of these materials.
It has been suggested that the thickness of a ceramic should be at least 2 mm in order to mask the effect of the underlying discolored tooth or the abutment color on the final color of the restoration [
17]. However, we found that IPS e.max Press ceramics with a lower thickness (0.5–1 mm) could mask the A4 substrate. This finding is important because, in many clinical cases, it is difficult to achieve a 2-mm axial reduction without compromising the strength of the remaining tooth structure. It should be kept in mind that the possibility of achieving maximum esthetics with limited tooth preparation is a critical factor [
18].
Matching the final color of restoration to its corresponding shade tab is another challenge when considering the material to use for restorative treatment, especially in the anterior region. The results showed that all combinations were capable of masking the underlying A4 substrate (ΔE = 8.63). In addition, an LT group (0.7 mm) exhibited the least color difference, corresponding to the best A2 VITA shade reproduction among all the groups. However, it is worth noting that the MO ingots showed ΔE values in the clinically acceptable range (< 3.3).
Similarly, Pande and Kolarkar [
19] reported that the best shade reproduction of LT IPS e.max was found in MO and high-opacity groups. In their study, the shade reproduction of MO ceramics was also good, but less than those of the LT groups. Nonetheless, it is evident that the fabrication of bilayer veneers is more difficult and time-consuming; therefore, LT ingots can be chosen instead of multilayered ceramics.
The difference in shade reproduction between different ingots could be attributed to their structure; Lithium disilicate consists of many small interlocking plate-like crystals that are randomly oriented. This ceramic is highly translucent due to the optical compatibility between the glassy matrix and the crystalline phase, which minimizes the internal scattering of light as it passes through it. Zirconium oxide and other oxides are added as opacifiers, and differences in the percentage of these opacifiers in the ingots could lead to variation in their shade reproduction ability [
16].
Based on the results of the current study, it can be suggested that clinicians should use LT ceramics with 0.5- and 0.7-mm thickness to avoid excessive tooth reduction, as recommended by the manufacturer.

