1. Schilder H. Filling root canals in three dimensions. 1967. J Endod. 2006; 32:281–290. PMID:
16554195.
2. Ørstavik D. Materials used for root canal obturation: technical, biological and clinical testing. Endod Topics. 2005; 12:25–38.
3. Grossman L. Endodontic practice. 10th ed. Philadelphia (PA): Henry Kimpton Publishers;1981.
4. Manappallil JJ. Basic dental materials. 4th ed. New Delhi: Jaypee Brothers Medical Publishers;2015.
5. Berman LH, Hargreaves K, Cohen S. Cohen's pathways of the pulp expert consult. 10th ed. Maryland Heights (MO): Mosby Elsevier;2010.
6. Garrido AD, Lia RC, França SC, da Silva JF, Astolfi-Filho S, Sousa-Neto MD. Laboratory evaluation of the physicochemical properties of a new root canal sealer based on
Copaifera multijuga oil-resin. Int Endod J. 2010; 43:283–291. PMID:
20487447.
7. Lee JK, Kwak SW, Ha JH, Lee W, Kim HC. Physicochemical properties of epoxy resin-based and bioceramic-based root canal sealers. Bioinorg Chem Appl. 2017; 2017:2582849. PMID:
28210204.

8. Poggio C, Arciola CR, Dagna A, Colombo M, Bianchi S, Visai L. Solubility of root canal sealers: a comparative study. Int J Artif Organs. 2010; 33:676–681. PMID:
20963731.

9. McMichen FR, Pearson G, Rahbaran S, Gulabivala K. A comparative study of selected physical properties of five root-canal sealers. Int Endod J. 2003; 36:629–635. PMID:
12950578.

10. Schweikl H, Schmalz G, Federlin M. Mutagenicity of the root canal sealer AHPlus in the Ames test. Clin Oral Investig. 1998; 2:125–129.

11. Azar NG, Heidari M, Bahrami ZS, Shokri F.
In vitro cytotoxicity of a new epoxy resin root canal sealer. J Endod. 2000; 26:462–465. PMID:
11199780.
12. Cohen BI, Pagnillo MK, Musikant BL, Deutsch AS. An
in vitro study of the cytotoxicity of two root canal sealers. J Endod. 2000; 26:228–229. PMID:
11199724.
13. Sousa CJ, Montes CR, Pascon EA, Loyola AM, Versiani MA. Comparison of the intraosseous biocompatibility of AH Plus, EndoREZ, and Epiphany root canal sealers. J Endod. 2006; 32:656–662. PMID:
16793475.

14. Roggendorf MJ, Ebert J, Petschelt A, Frankenberger R. Influence of moisture on the apical seal of root canal fillings with five different types of sealer. J Endod. 2007; 33:31–33. PMID:
17185125.

15. Camilleri J, Montesin FE, Brady K, Sweeney R, Curtis RV, Ford TR. The constitution of mineral trioxide aggregate. Dent Mater. 2005; 21:297–303. PMID:
15766576.

16. Asgary S, Parirokh M, Eghbal MJ, Stowe S, Brink F. A qualitative X-ray analysis of white and grey mineral trioxide aggregate using compositional imaging. J Mater Sci Mater Med. 2006; 17:187–191. PMID:
16502252.

17. Parirokh M, Torabinejad M. Mineral trioxide aggregate: a comprehensive literature review--Part I: chemical, physical, and antibacterial properties. J Endod. 2010; 36:16–27. PMID:
20003930.

18. Lee SJ, Monsef M, Torabinejad M. Sealing ability of a mineral trioxide aggregate for repair of lateral root perforations. J Endod. 1993; 19:541–544. PMID:
8151240.

19. Darvell BW, Wu RC. “MTA”-an Hydraulic Silicate Cement: review update and setting reaction. Dent Mater. 2011; 27:407–422. PMID:
21353694.

20. Donnermeyer D, Bürklein S, Dammaschke T, Schäfer E. Endodontic sealers based on calcium silicates: a systematic review. Odontology. 2019; 107:421–436. PMID:
30554288.

21. Donnermeyer D, Dornseifer P, Schäfer E, Dammaschke T. The push-out bond strength of calcium silicate-based endodontic sealers. Head Face Med. 2018; 14:13. PMID:
30126425.

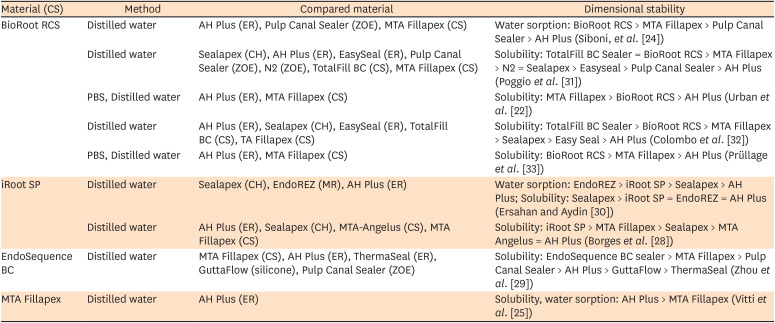
22. Urban K, Neuhaus J, Donnermeyer D, Schäfer E, Dammaschke T. Solubility and pH value of 3 different root canal sealers: a long-term investigation. J Endod. 2018; 44:1736–1740. PMID:
30243663.

23. Asawaworarit W, Yachor P, Kijsamanmith K, Vongsavan N. Comparison of the apical sealing ability of calcium silicate-based sealer and resin-based sealer using the fluid-filtration technique. Med Princ Pract. 2016; 25:561–565. PMID:
27599002.

24. Siboni F, Taddei P, Zamparini F, Prati C, Gandolfi MG. Properties of BioRoot RCS, a tricalcium silicate endodontic sealer modified with povidone and polycarboxylate. Int Endod J. 2017; 50(Suppl 2):e120–e136. PMID:
28881478.

25. Vitti RP, Prati C, Silva EJ, Sinhoreti MA, Zanchi CH, de Souza e Silva MG, Ogliari FA, Piva E, Gandolfi MG. Physical properties of MTA Fillapex sealer. J Endod. 2013; 39:915–918. PMID:
23791263.

26. International Organization of Standardization. International Standard ISO 6876. Specification for dental root canal sealing materials. 3rd ed. Geneva: International Organization of Standardization;2012.
27. Kebudi Benezra M, Schembri Wismayer P, Camilleri J. Influence of environment on testing of hydraulic sealers. Sci Rep. 2017; 7:17927. PMID:
29263328.

28. Borges RP, Sousa-Neto MD, Versiani MA, Rached-Júnior FA, De-Deus G, Miranda CE, Pécora JD. Changes in the surface of four calcium silicate-containing endodontic materials and an epoxy resin-based sealer after a solubility test. Int Endod J. 2012; 45:419–428. PMID:
22150403.

29. Zhou HM, Shen Y, Zheng W, Li L, Zheng YF, Haapasalo M. Physical properties of 5 root canal sealers. J Endod. 2013; 39:1281–1286. PMID:
24041392.

30. Ersahan S, Aydin C. Solubility and apical sealing characteristics of a new calcium silicate-based root canal sealer in comparison to calcium hydroxide-, methacrylate resin- and epoxy resin-based sealers. Acta Odontol Scand. 2013; 71:857–862. PMID:
23088627.

31. Poggio C, Dagna A, Ceci M, Meravini MV, Colombo M, Pietrocola G. Solubility and pH of bioceramic root canal sealers: a comparative study. J Clin Exp Dent. 2017; 9:e1189–e1194. PMID:
29167707.

32. Colombo M, Poggio C, Dagna A, Meravini MV, Riva P, Trovati F, Pietrocola G. Biological and physico-chemical properties of new root canal sealers. J Clin Exp Dent. 2018; 10:e120–e126. PMID:
29670728.

33. Prüllage RK, Urban K, Schäfer E, Dammaschke T. Material properties of a tricalcium silicate-containing, a mineral trioxide aggregate-containing, and an epoxy resin-based root canal sealer. J Endod. 2016; 42:1784–1788. PMID:
27769676.

34. Wu MK, De Gee AJ, Wesselink PR, Moorer WR. Fluid transport and bacterial penetration along root canal fillings. Int Endod J. 1993; 26:203–208. PMID:
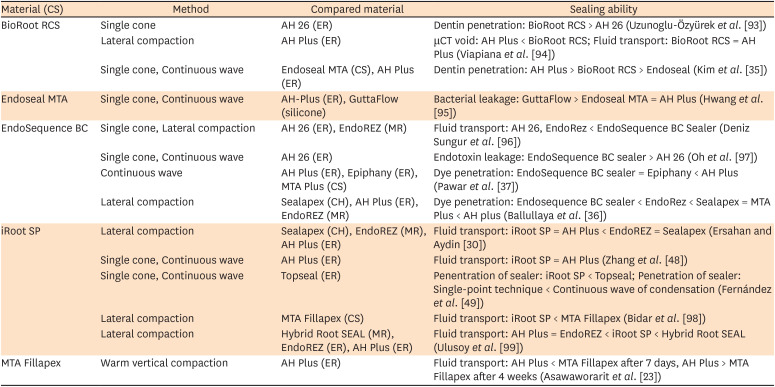
8225638.

35. Kim Y, Kim BS, Kim YM, Lee D, Kim SY. The penetration ability of calcium silicate root canal sealers into dentinal tubules compared to conventional resin-based sealer: a confocal laser scanning microscopy study. Materials (Basel). 2019; 12:E531. PMID:
30754612.

36. Ballullaya SV, Vinay V, Thumu J, Devalla S, Bollu IP, Balla S. Stereomicroscopic dye leakage measurement of six different root canal sealers. J Clin Diagn Res. 2017; 11:ZC65–ZC68. PMID:
28764296.

37. Pawar SS, Pujar MA, Makandar SD. Evaluation of the apical sealing ability of bioceramic sealer, AH plus & epiphany: an
in vitro study. J Conserv Dent. 2014; 17:579–582. PMID:
25506149.
38. Jafari F, Jafari S. Importance and methodologies of endodontic microleakage studies: a systematic review. J Clin Exp Dent. 2017; 9:e812–e819. PMID:
28638561.

39. Atmeh AR, Chong EZ, Richard G, Festy F, Watson TF. Dentin-cement interfacial interaction: calcium silicates and polyalkenoates. J Dent Res. 2012; 91:454–459. PMID:
22436906.
40. Jeong JW, DeGraft-Johnson A, Dorn SO, Di Fiore PM. Dentinal tubule penetration of a calcium silicate-based root canal sealer with different obturation methods. J Endod. 2017; 43:633–637. PMID:
28216267.

41. Holland R, de Souza V, Nery MJ, Otoboni Filho JA, Bernabé PF, Dezan Júnior E. Reaction of rat connective tissue to implanted dentin tubes filled with mineral trioxide aggregate or calcium hydroxide. J Endod. 1999; 25:161–166. PMID:
10321179.

42. Gandolfi MG, Prati C. MTA and F-doped MTA cements used as sealers with warm gutta-percha. Long-term study of sealing ability. Int Endod J. 2010; 43:889–901. PMID:
20618878.

43. Iacono F, Gandolfi MG, Huffman B, Sword J, Agee K, Siboni F, Tay F, Prati C, Pashley D. Push-out strength of modified Portland cements and resins. Am J Dent. 2010; 23:43–46. PMID:
20437727.
44. Weller RN, Tay KC, Garrett LV, Mai S, Primus CM, Gutmann JL, Pashley DH, Tay FR. Microscopic appearance and apical seal of root canals filled with gutta-percha and ProRoot Endo Sealer after immersion in a phosphate-containing fluid. Int Endod J. 2008; 41:977–986. PMID:
19133087.

45. Neelakantan P, Subbarao C, Subbarao CV, De-Deus G, Zehnder M. The impact of root dentine conditioning on sealing ability and push-out bond strength of an epoxy resin root canal sealer. Int Endod J. 2011; 44:491–498. PMID:
21255047.

46. Lee YL, Lin FH, Wang WH, Ritchie HH, Lan WH, Lin CP. Effects of EDTA on the hydration mechanism of mineral trioxide aggregate. J Dent Res. 2007; 86:534–538. PMID:
17525353.

47. Wu MK, Bud MG, Wesselink PR. The quality of single cone and laterally compacted gutta-percha fillings in small and curved root canals as evidenced by bidirectional radiographs and fluid transport measurements. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009; 108:946–951. PMID:
19875314.

48. Zhang W, Li Z, Peng B. Assessment of a new root canal sealer's apical sealing ability. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009; 107:e79–e82. PMID:
19464650.

49. Fernández R, Restrepo JS, Aristizábal DC, Álvarez LG. Evaluation of the filling ability of artificial lateral canals using calcium silicate-based and epoxy resin-based endodontic sealers and two gutta-percha filling techniques. Int Endod J. 2016; 49:365–373. PMID:
25827199.

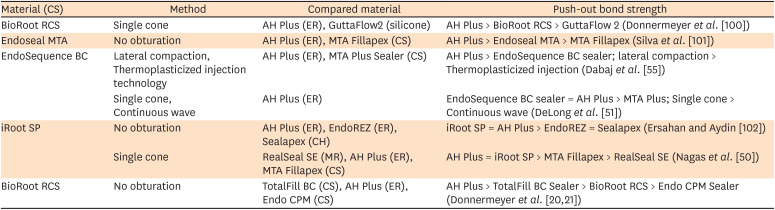
50. Nagas E, Cehreli Z, Uyanik MO, Durmaz V. Bond strength of a calcium silicate-based sealer tested in bulk or with different main core materials. Braz Oral Res. 2014; 28:S1806-83242014000100256.

51. DeLong C, He J, Woodmansey KF. The effect of obturation technique on the push-out bond strength of calcium silicate sealers. J Endod. 2015; 41:385–388. PMID:
25576202.

52. Reyes-Carmona JF, Felippe MS, Felippe WT. The biomineralization ability of mineral trioxide aggregate and Portland cement on dentin enhances the push-out strength. J Endod. 2010; 36:286–291. PMID:
20113792.

53. Camilleri J. Sealers and warm gutta-percha obturation techniques. J Endod. 2015; 41:72–78. PMID:
25115660.

54. Viapiana R, Guerreiro-Tanomaru JM, Tanomaru-Filho M, Camilleri J. Investigation of the effect of sealer use on the heat generated at the external root surface during root canal obturation using warm vertical compaction technique with System B heat source. J Endod. 2014; 40:555–561. PMID:
24666911.
55. Dabaj P, Kalender A, Unverdi Eldeniz A. Push-out bond strength and SEM evaluation in roots filled with two different techniques using new and conventional sealers. Materials (Basel). 2018; 11:E1620. PMID:
30189631.

56. Qu W, Bai W, Liang YH, Gao XJ. Influence of warm vertical compaction technique on physical properties of root canal sealers. J Endod. 2016; 42:1829–1833. PMID:
27776877.

57. Zhang W, Li Z, Peng B.
Ex vivo cytotoxicity of a new calcium silicate-based canal filling material. Int Endod J. 2010; 43:769–774. PMID:
20546044.
58. Chang SW, Lee SY, Kang SK, Kum KY, Kim EC.
In vitro biocompatibility, inflammatory response, and osteogenic potential of 4 root canal sealers: Sealapex, Sankin apatite root sealer, MTA Fillapex, and iRoot SP root canal sealer. J Endod. 2014; 40:1642–1648. PMID:
25260738.
59. Eldeniz AU, Shehata M, Högg C, Reichl FX. DNA double-strand breaks caused by new and contemporary endodontic sealers. Int Endod J. 2016; 49:1141–1151. PMID:
26574345.

60. Jung S, Libricht V, Sielker S, Hanisch MR, Schäfer E, Dammaschke T. Evaluation of the biocompatibility of root canal sealers on human periodontal ligament cells
ex vivo
. Odontology. 2019; 107:54–63. PMID:
30039235.
61. Taraslia V, Anastasiadou E, Lignou C, Keratiotis G, Agrafioti A, Kontakiotis EG. Assessment of cell viability in four novel endodontic sealers. Eur J Dent. 2018; 12:287–291. PMID:
29988252.

62. Ames JM, Loushine RJ, Babb BR, Bryan TE, Lockwood PE, Sui M, Roberts S, Weller RN, Pashley DH, Tay FR. Contemporary methacrylate resin-based root canal sealers exhibit different degrees of
ex vivo cytotoxicity when cured in their self-cured mode. J Endod. 2009; 35:225–228. PMID:
19166778.
63. Collado-González M, García-Bernal D, Oñate-Sánchez RE, Ortolani-Seltenerich PS, Lozano A, Forner L, Llena C, Rodríguez-Lozano FJ. Biocompatibility of three new calcium silicate-based endodontic sealers on human periodontal ligament stem cells. Int Endod J. 2017; 50:875–884. PMID:
27666949.

64. Kebudi Benezra M, Schembri Wismayer P, Camilleri J. Interfacial characteristics and cytocompatibility of hydraulic sealer cements. J Endod. 2018; 44:1007–1017. PMID:
29398087.

65. Zhou HM, Du TF, Shen Y, Wang ZJ, Zheng YF, Haapasalo M.
In vitro cytotoxicity of calcium silicate-containing endodontic sealers. J Endod. 2015; 41:56–61. PMID:
25442721.
66. Poggio C, Riva P, Chiesa M, Colombo M, Pietrocola G. Comparative cytotoxicity evaluation of eight root canal sealers. J Clin Exp Dent. 2017; 9:e574–e578. PMID:
28469826.

67. da Silva EJ, Zaia AA, Peters OA. Cytocompatibility of calcium silicate-based sealers in a three-dimensional cell culture model. Clin Oral Investig. 2017; 21:1531–1536.

68. Portella FF, Collares FM, Dos Santos LA, dos Santos BP, Camassola M, Leitune VC, Samuel SM. Glycerol salicylate-based containing α-tricalcium phosphate as a bioactive root canal sealer. J Biomed Mater Res B Appl Biomater. 2015; 103:1663–1669. PMID:
25611332.

69. Loushine BA, Bryan TE, Looney SW, Gillen BM, Loushine RJ, Weller RN, Pashley DH, Tay FR. Setting properties and cytotoxicity evaluation of a premixed bioceramic root canal sealer. J Endod. 2011; 37:673–677. PMID:
21496669.

70. Lee BN, Hong JU, Kim SM, Jang JH, Chang HS, Hwang YC, Hwang IN, Oh WM. Anti-inflammatory and osteogenic effects of calcium silicate-based root canal sealers. J Endod. 2019; 45:73–78. PMID:
30558800.

71. Zhang H, Shen Y, Ruse ND, Haapasalo M. Antibacterial activity of endodontic sealers by modified direct contact test against
Enterococcus faecalis
. J Endod. 2009; 35:1051–1055. PMID:
19567333.
72. Sjögren U, Figdor D, Persson S, Sundqvist G. Influence of infection at the time of root filling on the outcome of endodontic treatment of teeth with apical periodontitis. Int Endod J. 1997; 30:297–306. PMID:
9477818.

73. Stuart CH, Schwartz SA, Beeson TJ, Owatz CB.
Enterococcus faecalis: its role in root canal treatment failure and current concepts in retreatment. J Endod. 2006; 32:93–98. PMID:
16427453.
74. Desai S, Chandler N. Calcium hydroxide-based root canal sealers: a review. J Endod. 2009; 35:475–480. PMID:
19345790.

75. Jafari F, Jafari S. Composition and physicochemical properties of calcium silicate based sealers: a review article. J Clin Exp Dent. 2017; 9:e1249–e1255. PMID:
29167717.

76. Cai M, Abbott P, Castro Salgado J. Hydroxyl ion diffusion through radicular dentine when calcium hydroxide is used under different conditions. Materials (Basel). 2018; 11:E152. PMID:
29342093.
77. Candeiro GT, Moura-Netto C, D'Almeida-Couto RS, Azambuja-Júnior N, Marques MM, Cai S, Gavini G. Cytotoxicity, genotoxicity and antibacterial effectiveness of a bioceramic endodontic sealer. Int Endod J. 2016; 49:858–864. PMID:
26281002.

78. Arias-Moliz MT, Camilleri J. The effect of the final irrigant on the antimicrobial activity of root canal sealers. J Dent. 2016; 52:30–36. PMID:
27377571.

79. Wang Z, Shen Y, Haapasalo M. Dentin extends the antibacterial effect of endodontic sealers against
Enterococcus faecalis biofilms. J Endod. 2014; 40:505–508. PMID:
24666900.
80. Alsubait S, Albader S, Alajlan N, Alkhunaini N, Niazy A, Almahdy A. Comparison of the antibacterial activity of calcium silicate- and epoxy resin-based endodontic sealers against
Enterococcus faecalis biofilms: a confocal laser-scanning microscopy analysis. Odontology. 2019; 107:513–520. PMID:
30927150.
81. Nirupama DN, Nainan MT, Ramaswamy R, Muralidharan S, Usha HH, Sharma R, Gupta S.
In vitro evaluation of the antimicrobial efficacy of four endodontic biomaterials against
Enterococcus faecalis, Candida albicans, and
Staphylococcus aureus
. Int J Biomater. 2014; 2014:383756. PMID:
25371678.
82. Shin JH, Lee DY, Lee SH. Comparison of antimicrobial activity of traditional and new developed root sealers against pathogens related root canal. J Dent Sci. 2018; 13:54–59. PMID:
30895095.

83. Willershausen I, Callaway A, Briseño B, Willershausen B.
In vitro analysis of the cytotoxicity and the antimicrobial effect of four endodontic sealers. Head Face Med. 2011; 7:15. PMID:
21831282.

84. Kokubo T, Takadama H. How useful is SBF in predicting
in vivo bone bioactivity? Biomaterials. 2006; 27:2907–2915. PMID:
16448693.
85. Zhang W, Li Z, Peng B. Effects of iRoot SP on mineralization-related genes expression in MG63 cells. J Endod. 2010; 36:1978–1982. PMID:
21092816.

86. Camps J, Jeanneau C, El Ayachi I, Laurent P, About I. Bioactivity of a calcium silicate-based endodontic cement (BioRoot RCS): interactions with human periodontal ligament cells
in vitro
. J Endod. 2015; 41:1469–1473. PMID:
26001857.
87. Güven EP, Taşlı PN, Yalvac ME, Sofiev N, Kayahan MB, Sahin F.
In vitro comparison of induction capacity and biomineralization ability of mineral trioxide aggregate and a bioceramic root canal sealer. Int Endod J. 2013; 46:1173–1182. PMID:
23617276.
88. Loison-Robert LS, Tassin M, Bonte E, Berbar T, Isaac J, Berdal A, Simon S, Fournier BP.
In vitro effects of two silicate-based materials, Biodentine and BioRoot RCS, on dental pulp stem cells in models of reactionary and reparative dentinogenesis. PLoS One. 2018; 13:e0190014. PMID:
29370163.
89. Dimitrova-Nakov S, Uzunoglu E, Ardila-Osorio H, Baudry A, Richard G, Kellermann O, Goldberg M.
In vitro bioactivity of Bioroot™ RCS, via A4 mouse pulpal stem cells. Dent Mater. 2015; 31:1290–1297. PMID:
26364144.
90. Yoo YJ, Baek SH, Kum KY, Shon WJ, Woo KM, Lee W. Dynamic intratubular biomineralization following root canal obturation with pozzolan-based mineral trioxide aggregate sealer cement. Scanning. 2016; 38:50–56. PMID:
26179659.

91. Nawal RR, Parande M, Sehgal R, Naik A, Rao NR. A comparative evaluation of antimicrobial efficacy and flow properties for Epiphany, Guttaflow and AH-Plus sealer. Int Endod J. 2011; 44:307–313. PMID:
21219358.

92. Al-Haddad A, Che Ab Aziz ZA. Bioceramic-based root canal sealers: a review. Int J Biomater. 2016; 2016:9753210. PMID:
27242904.

93. Uzunoglu-Özyürek E, Erdoğan Ö, Aktemur Türker S. Effect of calcium hydroxide dressing on the dentinal tubule penetration of 2 different root canal sealers: a confocal laser scanning microscopic study. J Endod. 2018; 44:1018–1023. PMID:
29680722.

94. Viapiana R, Moinzadeh AT, Camilleri L, Wesselink PR, Tanomaru Filho M, Camilleri J. Porosity and sealing ability of root fillings with gutta-percha and BioRoot RCS or AH Plus sealers. Evaluation by three
ex vivo methods. Int Endod J. 2016; 49:774–782. PMID:
26199130.
95. Hwang JH, Chung J, Na HS, Park E, Kwak S, Kim HC. Comparison of bacterial leakage resistance of various root canal filling materials and methods: confocal laser-scanning microscope study. Scanning. 2015; 37:422–428. PMID:
26114421.

96. Deniz Sungur D, Moinzadeh AT, Wesselink PR, Çalt Tarhan S, Özok AR. Sealing efficacy of a single-cone root filling after post space preparation. Clin Oral Investig. 2016; 20:1071–1077.

97. Oh S, Cho SI, Perinpanayagam H, You J, Hong SH, Yoo YJ, Chang SW, Shon WJ, Yoo JS, Baek SH, Kum KY. Novel calcium zirconate silicate cement biomineralize and seal root canals. Materials (Basel). 2018; 11:E588. PMID:
29641475.

98. Bidar M, Sadeghalhoseini N, Forghani M, Attaran N. Effect of the smear layer on apical seals produced by two calcium silicate-based endodontic sealers. J Oral Sci. 2014; 56:215–219. PMID:
25231148.

99. Ulusoy OI, Nayir Y, Celik K, Yaman SD. Apical microleakage of different root canal sealers after use of maleic acid and EDTA as final irrigants. Braz Oral Res. 2014; 28:S1806-83242014000100257.

100. Donnermeyer D, Vahdat-Pajouh N, Schäfer E, Dammaschke T. Influence of the final irrigation solution on the push-out bond strength of calcium silicate-based, epoxy resin-based and silicone-based endodontic sealers. Odontology. 2019; 107:231–236. PMID:
30276580.

101. Silva EJ, Carvalho NK, Prado MC, Zanon M, Senna PM, Souza EM, De-Deus G. Push-out bond strength of injectable Pozzolan-based root canal sealer. J Endod. 2016; 42:1656–1659. PMID:
27641946.

102. Ersahan S, Aydin C. Dislocation resistance of iRoot SP, a calcium silicate-based sealer, from radicular dentine. J Endod. 2010; 36:2000–2002. PMID:
21092821.

103. Alsubait SA, Al Ajlan R, Mitwalli H, Aburaisi N, Mahmood A, Muthurangan M, Almadhri R, Alfayez M, Anil S. Cytotoxicity of different concentrations of three root canal sealers on human mesenchymal stem cells. Biomolecules. 2018; 8:E68. PMID:
30071665.

104. Lim ES, Park YB, Kwon YS, Shon WJ, Lee KW, Min KS. Physical properties and biocompatibility of an injectable calcium-silicate-based root canal sealer:
in vitro and
in vivo study. BMC Oral Health. 2015; 15:129. PMID:
26490372.





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download