1. Frassetto A, Breschi L, Turco G, Marchesi G, Di Lenarda R, Tay FR, Pashley DH, Cadenaro M. Mechanisms of degradation of the hybrid layer in adhesive dentistry and therapeutic agents to improve bond durability--A literature review. Dent Mater. 2016; 32:e41–e53. PMID:
26743967.

2. Anchieta RB, Machado LS, Sundfeld RH, Reis AF, Giannini M, Luersen MA, Janal M, Rocha EP, Coelho PG. Effect of partially demineralized dentin beneath the hybrid layer on dentin-adhesive interface micromechanics. J Biomech. 2015; 48:701–707. PMID:
25596632.
3. Toledano M, Osorio R, Osorio E, Fuentes V, Prati C, Garcìa-Godoy F. Sorption and solubility of resin-based restorative dental materials. J Dent. 2003; 31:43–50. PMID:
12615019.

4. Mazzoni A, Tjäderhane L, Checchi V, Di Lenarda R, Salo T, Tay FR, Pashley DH, Breschi L. Role of dentin MMPs in caries progression and bond stability. J Dent Res. 2015; 94:241–251. PMID:
25535202.

5. Osorio R, Yamauti M, Osorio E, Ruiz-Requena ME, Pashley D, Tay F, Toledano M. Effect of dentin etching and chlorhexidine application on metalloproteinase-mediated collagen degradation. Eur J Oral Sci. 2011; 119:79–85. PMID:
21244516.

6. Zhang SC, Kern M. The role of host-derived dentinal matrix metalloproteinases in reducing dentin bonding of resin adhesives. Int J Oral Sci. 2009; 1:163–176. PMID:
20690420.

7. Favetti M, Schroeder T, Montagner AF, Correa MB, Pereira-Cenci T, Cenci MS. Effectiveness of pre-treatment with chlorhexidine in restoration retention: a 36-month follow-up randomized clinical trial. J Dent. 2017; 60:44–49. PMID:
28237629.

8. Niu LN, Zhang W, Pashley DH, Breschi L, Mao J, Chen JH, Tay FR. Biomimetic remineralization of dentin. Dent Mater. 2014; 30:77–96. PMID:
23927881.

9. Almahdy A, Koller G, Sauro S, Bartsch JW, Sherriff M, Watson TF, Banerjee A. Effects of MMP inhibitors incorporated within dental adhesives. J Dent Res. 2012; 91:605–611. PMID:
22518030.

10. Epasinghe DJ, Yiu CK, Burrow MF, Hiraishi N, Tay FR. The inhibitory effect of proanthocyanidin on soluble and collagen-bound proteases. J Dent. 2013; 41:832–839. PMID:
23806340.

11. Santerre JP, Shajii L, Leung BW. Relation of dental composite formulations to their degradation and the release of hydrolyzed polymeric-resin-derived products. Crit Rev Oral Biol Med. 2001; 12:136–151. PMID:
11345524.

12. Lehmann N, Debret R, Roméas A, Magloire H, Degrange M, Bleicher F, Sommer P, Seux D. Self-etching increases matrix metalloproteinase expression in the dentin-pulp complex. J Dent Res. 2009; 88:77–82. PMID:
19131322.
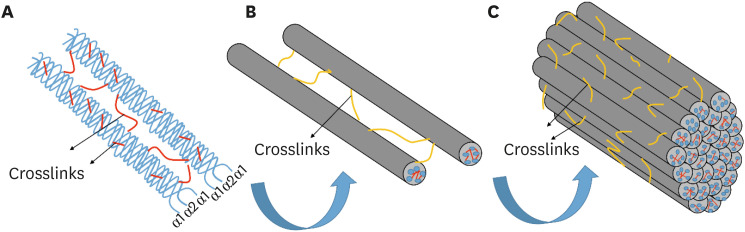
13. Perumal S, Antipova O, Orgel JP. Collagen fibril architecture, domain organization, and triple-helical conformation govern its proteolysis. Proc Natl Acad Sci U S A. 2008; 105:2824–2829. PMID:
18287018.

14. Fields GB. Interstitial collagen catabolism. J Biol Chem. 2013; 288:8785–8793. PMID:
23430258.

15. Bertassoni LE. Dentin on the nanoscale: hierarchical organization, mechanical behavior and bioinspired engineering. Dent Mater. 2017; 33:637–649. PMID:
28416222.

16. Bertassoni LE, Orgel JP, Antipova O, Swain MV. The dentin organic matrix - limitations of restorative dentistry hidden on the nanometer scale. Acta Biomater. 2012; 8:2419–2433. PMID:
22414619.

17. Bertassoni LE, Swain MV. Removal of dentin non-collagenous structures results in the unraveling of microfibril bundles in collagen type I. Connect Tissue Res. 2017; 58:414–423. PMID:
27657550.

18. Scheffel DL, Hebling J, Scheffel RH, Agee K, Turco G, de Souza Costa CA, Pashley D. Inactivation of matrix-bound matrix metalloproteinases by cross-linking agents in acid-etched dentin. Oper Dent. 2014; 39:152–158. PMID:
23786610.

19. Toledano M, Aguilera FS, Yamauti M, Ruiz-Requena ME, Osorio R.
In vitro load-induced dentin collagen-stabilization against MMPs degradation. J Mech Behav Biomed Mater. 2013; 27:10–18. PMID:
23834971.
20. Mazzoni A, Scaffa P, Carrilho M, Tjäderhane L, Di Lenarda R, Polimeni A, Tezvergil-Mutluay A, Tay FR, Pashley DH, Breschi L. Effects of etch-and-rinse and self-etch adhesives on dentin MMP-2 and MMP-9. J Dent Res. 2013; 92:82–86. PMID:
23128110.

21. Pessoa JI, Guimarães GN, Viola NV, da Silva WJ, de Souza AP, Tjäderhane L, Line SR, Marques MR.
In situ study of the gelatinase activity in demineralized dentin from rat molar teeth. Acta Histochem. 2013; 115:245–251. PMID:
22897943.
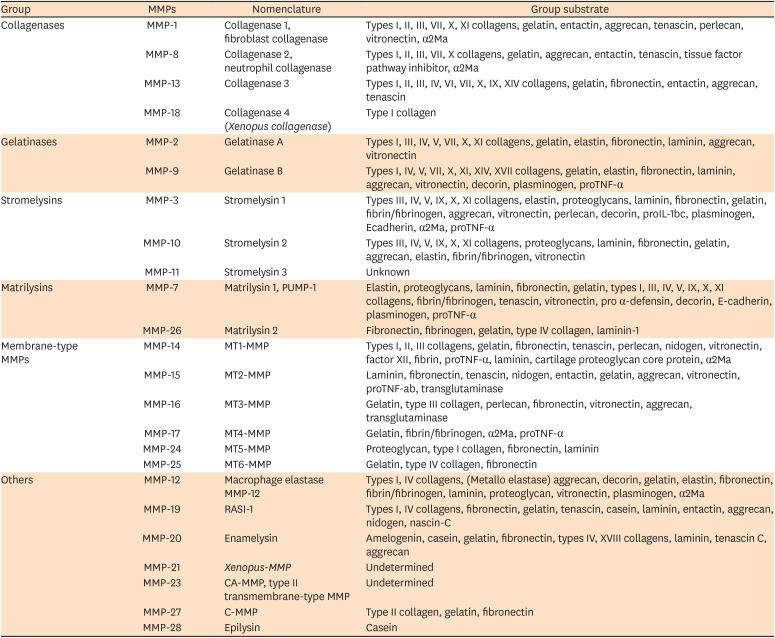
22. Hannas AR, Pereira JC, Granjeiro JM, Tjäderhane L. The role of matrix metalloproteinases in the oral environment. Acta Odontol Scand. 2007; 65:1–13. PMID:
17354089.

23. Krizkova A, Zitka O, Adam V, Kizek R, Masarik M, Stiborova M, Eckschager T, Chavis GJ. Assays for determination of matrix metalloproteinases and their activity. Trends Analyt Chem. 2011; 30:1819–1832.

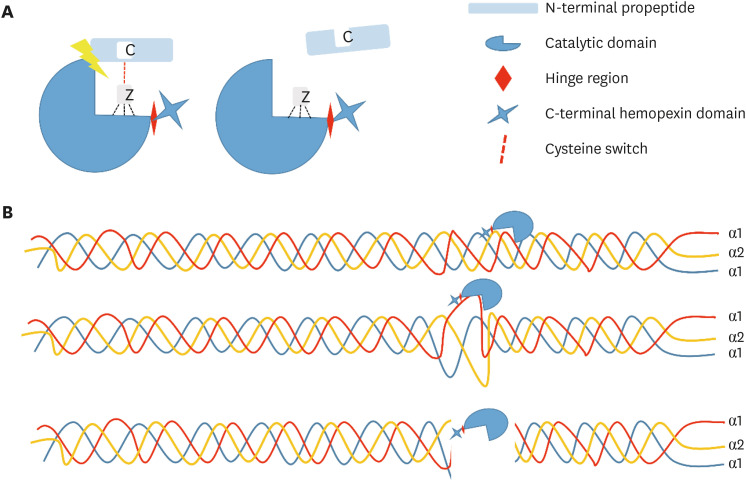
24. Cieplak P, Strongin AY. Matrix metalloproteinases - From the cleavage data to the prediction tools and beyond. Biochim Biophys Acta Mol Cell Res. 2017; 1864:1952–1963. PMID:
28347746.

25. Jacobsen JA, Major Jourden JL, Miller MT, Cohen SM. To bind zinc or not to bind zinc: an examination of innovative approaches to improved metalloproteinase inhibition. Biochim Biophys Acta. 2010; 1803:72–94. PMID:
19712708.

26. Xu X, Chen Z, Wang Y, Bonewald L, Steffensen B. Inhibition of MMP-2 gelatinolysis by targeting exodomain-substrate interactions. Biochem J. 2007; 406:147–155. PMID:
17516913.

27. Page-McCaw A, Ewald AJ, Werb Z. Matrix metalloproteinases and the regulation of tissue remodelling. Nat Rev Mol Cell Biol. 2007; 8:221–233. PMID:
17318226.

28. Mazzoni A, Breschi L, Carrilho M, Nascimento FD, Orsini G, Ruggeri A Jr, Gobbi P, Manzoli L, Tay FR, Pashley DH, Tjäderhane L. A review of the nature, role, and function of dentin non-collagenous proteins. Part II: enzymes, serum proteins, and growth factors. Endod Topics. 2009; 21:19–40.

29. Bedran-Russo AK, Pauli GF, Chen SN, McAlpine J, Castellan CS, Phansalkar RS, Aguiar TR, Vidal CM, Napotilano JG, Nam JW, Leme AA. Dentin biomodification: strategies, renewable resources and clinical applications. Dent Mater. 2014; 30:62–76. PMID:
24309436.

30. Sabatini C, Pashley DH. Mechanisms regulating the degradation of dentin matrices by endogenous dentin proteases and their role in dental adhesion. A review. Am J Dent. 2014; 27:203–214. PMID:
25831604.
31. Scheffel DL, Hebling J, Scheffel RH, Agee KA, Cadenaro M, Turco G, Breschi L, Mazzoni A, de Souza Costa CA, Pashley DH. Stabilization of dentin matrix after cross-linking treatments,
in vitro
. Dent Mater. 2014; 30:227–233. PMID:
24332989.
32. Tezvergil-Mutluay A, Agee KA, Hoshika T, Carrilho M, Breschi L, Tjäderhane L, Nishitani Y, Carvalho RM, Looney S, Tay FR, Pashley DH. The requirement of zinc and calcium ions for functional MMP activity in demineralized dentin matrices. Dent Mater. 2010; 26:1059–1067. PMID:
20688380.

33. Mei ML, Li QL, Chu CH, Yiu CK, Lo EC. The inhibitory effects of silver diamine fluoride at different concentrations on matrix metalloproteinases. Dent Mater. 2012; 28:903–908. PMID:
22578660.

34. Tezvergil-Mutluay A, Mutluay M, Seseogullari-Dirihan R, Agee KA, Key WO, Scheffel DL, Breschi L, Mazzoni A, Tjäderhane L, Nishitani Y, Tay FR, Pashley DH. Effect of phosphoric acid on the degradation of human dentin matrix. J Dent Res. 2013; 92:87–91. PMID:
23103634.

35. Seseogullari-Dirihan R, Mutluay MM, Pashley DH, Tezvergil-Mutluay A. Is the inactivation of dentin proteases by crosslinkers reversible? Dent Mater. 2017; 33:e62–e68. PMID:
27745773.

36. Fields GB. New strategies for targeting matrix metalloproteinases. Matrix Biol. 2015; 44-46:239–246. PMID:
25595836.

37. Breschi L, Mazzoni A, Ruggeri A, Cadenaro M, Di Lenarda R, De Stefano Dorigo E. Dental adhesion review: aging and stability of the bonded interface. Dent Mater. 2008; 24:90–101. PMID:
17442386.

38. Hass V, de Paula AM, Parreiras S, Gutiérrez MF, Luque-Martinez I, de Paris Matos T, Bandeca MC, Loguercio AD, Yao X, Wang Y, Reis A. Degradation of dentin-bonded interfaces treated with collagen cross-linking agents in a cariogenic oral environment: an
in situ study. J Dent. 2016; 49:60–67. PMID:
27106766.
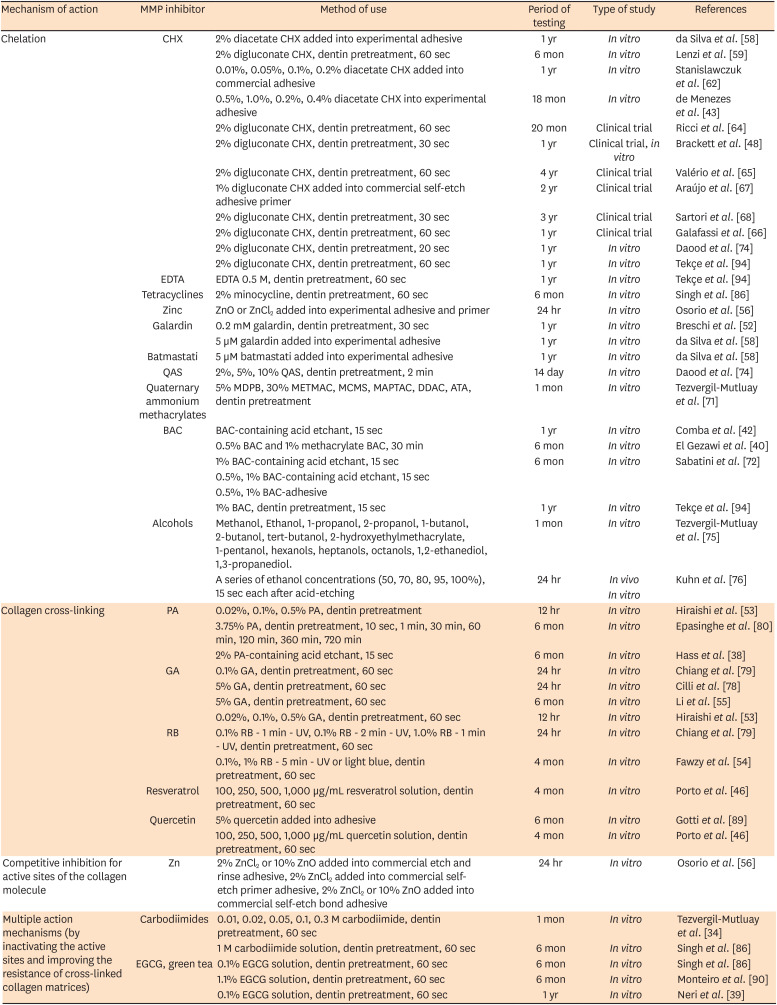
39. Neri JR, Yamauti M, da Silveira FD, Mendonça JS, de Carvalho RM, Santiago SL. Influence of dentin biomodification with epigallocatechin-3-gallate on the bond strength of self-etch adhesive: twelve-month results. Int J Adhes Adhes. 2016; 71:81–86.

40. El Gezawi M, Haridy R, Abo Elazm E, Al-Harbi F, Zouch M, Kaisarly D. Microtensile bond strength, 4-point bending and nanoleakage of resin-dentin interfaces: effects of two matrix metalloproteinase inhibitors. J Mech Behav Biomed Mater. 2018; 78:206–213. PMID:
29172125.

41. Siqueira FS, Hilgemberg B, Araujo LC, Hass V, Bandeca MC, Reis A, Gomes JC, Cardenas AF, Loguercio AD. Effect of phosphoric acid containing MMP-inactivator on the properties of resin bonding to eroded dentin. J Adhes Dent. 2019; 21:149–158. PMID:
30949628.
42. Comba A, Maravic T, Valente L, Girlando M, Cunha SR, Checchi V, Salgarello S, Tay FR, Scotti N, Breschi L, Mazzoni A. Effect of benzalkonium chloride on dentin bond strength and endogenous enzymatic activity. J Dent. 2019; 85:25–32. PMID:
30998949.

43. de Menezes LR, da Silva EO, Maurat da Rocha LV, Ferreira Barbosa I, Rodrigues Tavares M. The use of clays for chlorhexidine controlled release as a new perspective for longer durability of dentin adhesion. J Mater Sci Mater Med. 2019; 30:132. PMID:
31786679.

44. Simmer FS, da Silva EM, Bezerra RD, Miranda ME, Noronha Filho JD, Amaral CM. Bond stability of conventional adhesive system with MMP inhibitors to superficial and deep dentin. J Mech Behav Biomed Mater. 2019; 100:103402. PMID:
31493688.

45. Islam SM, Hiraishi N, Nassar M, Sono R, Otsuki M, Takatsura T, Yiu C, Tagami J.
In vitro effect of hesperidin on root dentin collagen and de/re-mineralization. Dent Mater J. 2012; 31:362–367. PMID:
22673464.
46. Porto IC, Nascimento TG, Oliveira JM, Freitas PH, Haimeur A, França R. Use of polyphenols as a strategy to prevent bond degradation in the dentin-resin interface. Eur J Oral Sci. 2018; 126:146–158. PMID:
29380895.

47. Huang B, Cvitkovitch DG, Santerre JP, Finer Y. Biodegradation of resin-dentin interfaces is dependent on the restorative material, mode of adhesion, esterase or MMP inhibition. Dent Mater. 2018; 34:1253–1262. PMID:
29789163.

48. Brackett MG, Li N, Brackett WW, Sword RJ, Qi YP, Niu LN, Pucci CR, Dib A, Pashley DH, Tay FR. The critical barrier to progress in dentine bonding with the etch-and-rinse technique. J Dent. 2011; 39:238–248. PMID:
21215788.

49. Montagner AF, Sarkis-Onofre R, Pereira-Cenci T, Cenci MS. MMP inhibitors on dentin stability: a systematic review and meta-analysis. J Dent Res. 2014; 93:733–743. PMID:
24935066.
50. Tjäderhane L, Nascimento FD, Breschi L, Mazzoni A, Tersariol IL, Geraldeli S, Tezvergil-Mutluay A, Carrilho MR, Carvalho RM, Tay FR, Pashley DH. Optimizing dentin bond durability: control of collagen degradation by matrix metalloproteinases and cysteine cathepsins. Dent Mater. 2013; 29:116–135. PMID:
22901826.

51. Moon PC, Weaver J, Brooks CN. Review of matrix metalloproteinases' effect on the hybrid dentin bond layer stability and chlorhexidine clinical use to prevent bond failure. Open Dent J. 2010; 4:147–152. PMID:
21339893.

52. Breschi L, Martin P, Mazzoni A, Nato F, Carrilho M, Tjäderhane L, Visintini E, Cadenaro M, Tay FR, De Stefano Dorigo E, Pashley DH. Use of a specific MMP-inhibitor (galardin) for preservation of hybrid layer. Dent Mater. 2010; 26:571–578. PMID:
20299089.

53. Hiraishi N, Sono R, Sofiqul I, Yiu C, Nakamura H, Otsuki M, Takatsuka T, Tagami J.
In vitro evaluation of plant-derived agents to preserve dentin collagen. Dent Mater. 2013; 29:1048–1054. PMID:
23942145.
54. Fawzy AS, Nitisusanta LI, Iqbal K, Daood U, Neo J. Riboflavin as a dentin crosslinking agent: ultraviolet A versus blue light. Dent Mater. 2012; 28:1284–1291. PMID:
23031483.

55. Li J, Chen B, Hong N, Wu S, Li Y. Effect of baicalein on matrix metalloproteinases and durability of resin-dentin bonding. Oper Dent. 2018; 43:426–436. PMID:
29513641.

56. Osorio R, Yamauti M, Osorio E, Román JS, Toledano M. Zinc-doped dentin adhesive for collagen protection at the hybrid layer. Eur J Oral Sci. 2011; 119:401–410. PMID:
21896058.

57. Almahdy A, Koller G, Festy F, Bartsch JW, Watson TF, Banerjee A. An MMP-inhibitor modified adhesive primer enhances bond durability to carious dentin. Dent Mater. 2015; 31:594–602. PMID:
25804191.

58. da Silva EM, de Sá Rodrigues CU, de Oliveira Matos MP, de Carvalho TR, dos Santos GB, Amaral CM. Experimental etch-and-rinse adhesive systems containing MMP-inhibitors: physicochemical characterization and resin-dentin bonding stability. J Dent. 2015; 43:1491–1497. PMID:
26456899.

59. Lenzi T, Tedesco TK, Soares FZ, Loguercio AD, Rocha RO. Chlorhexidine application for bond strength preservation in artificially-created caries-affected primary dentin. Int J Adhes Adhes. 2014; 54:51–56.

60. Carrilho MR, Tay FR, Donnelly AM, Agee KA, Tjäderhane L, Mazzoni A, Breschi L, Foulger S, Pashley DH. Host-derived loss of dentin matrix stiffness associated with solubilization of collagen. J Biomed Mater Res B Appl Biomater. 2009; 90:373–380. PMID:
19090493.

61. Blackburn RS, Harvey A, Kettle LL, Manian AP, Payne JD, Russell SJ. Sorption of chlorhexidine on cellulose: mechanism of binding and molecular recognition. J Phys Chem B. 2007; 111:8775–8784. PMID:
17602516.

62. Stanislawczuk R, Pereira F, Muñoz MA, Luque I, Farago PV, Reis A, Loguercio AD. Effects of chlorhexidine-containing adhesives on the durability of resin-dentine interfaces. J Dent. 2014; 42:39–47. PMID:
24252801.

63. Priyadarshini BM, Selvan ST, Lu TB, Xie H, Neo J, Fawzy AS. Chlorhexidine nanocapsule drug delivery approach to the resin-dentin interface. J Dent Res. 2016; 95:1065–1072. PMID:
27422859.

64. Ricci HA, Sanabe ME, de Souza Costa CA, Pashley DH, Hebling J. Chlorhexidine increases the longevity of
in vivo resin-dentin bonds. Eur J Oral Sci. 2010; 118:411–416. PMID:
20662916.
65. Valério RA, Galo R, Galafassi D, Corona SA, Borsatto MC. Four-year clinical prospective follow-up of resin composite restoration after selective caries removal using Er:YAG laser. Clin Oral Investig. 2019.

66. Galafassi D, Scatena C, Galo R, Curylofo-Zotti FA, Corona SA, Borsatto MC. Clinical evaluation of composite restorations in Er:YAG laser-prepared cavities re-wetting with chlorhexidine. Clin Oral Investig. 2017; 21:1231–1241.

67. Araújo MS, Souza LC, Apolonio FM, Barros LO, Reis A, Loguercio AD, Saboia VP. Two-year clinical evaluation of chlorhexidine incorporation in two-step self-etch adhesive. J Dent. 2015; 43:140–148. PMID:
25046536.

68. Sartori N, Stolf SC, Silva SB, Lopes GC, Carrilho M. Influence of chlorhexidine digluconate on the clinical performance of adhesive restorations: a 3-year follow-up. J Dent. 2013; 41:1188–1195. PMID:
24076103.

69. Tu G, Xu W, Huang H, Li S. Progress in the development of matrix metalloproteinase inhibitors. Curr Med Chem. 2008; 15:1388–1395. PMID:
18537616.

70. Imbery TA, Kennedy M, Janus C, Moon PC. Evaluating EDTA as a substitute for phosphoric acid-etching of enamel and dentin. Gen Dent. 2012; 60:e55–e61. PMID:
22414518.
71. Tezvergil-Mutluay A, Agee KA, Uchiyama T, Imazato S, Mutluay MM, Cadenaro M, Breschi L, Nishitani Y, Tay FR, Pashley DH. The inhibitory effects of quaternary ammonium methacrylates on soluble and matrix-bound MMPs. J Dent Res. 2011; 90:535–540. PMID:
21212315.

72. Sabatini C, Kim JH, Ortiz Alias P.
In vitro evaluation of benzalkonium chloride in the preservation of adhesive interfaces. Oper Dent. 2014; 39:283–290. PMID:
23937402.
73. Daood U, Yiu CK, Burrow MF, Niu LN, Tay FR. Effect of a novel quaternary ammonium silane on dentin protease activities. J Dent. 2017; 58:19–27. PMID:
28064012.

74. Daood D, Yiu CK, Burrow MF, Niu LN, Tay FR. Effect of a novel quaternary ammonium silane cavity disinfectant on durability of resin-dentine bond. J Dent. 2017; 60:77–86. PMID:
28315376.

75. Tezvergil-Mutluay A, Agee KA, Hoshika T, Uchiyama T, Tjäderhane L, Breschi L, Mazzoni A, Thompson JM, McCracken CE, Looney SW, Tay FR, Pashley DH. Inhibition of MMPs by alcohols. Dent Mater. 2011; 27:926–933. PMID:
21676453.

76. Kuhn E, Farhat P, Teitelbaum AP, Mena-Serrano A, Loguercio AD, Reis A, Pashley DH. Ethanol-wet bonding technique: clinical versus laboratory findings. Dent Mater. 2015; 31:1030–1037. PMID:
26113426.

77. Liu Y, Chen M, Yao X, Xu C, Zhang Y, Wang Y. Enhancement in dentin collagen's biological stability after proanthocyanidins treatment in clinically relevant time periods. Dent Mater. 2013; 29:485–492. PMID:
23434233.

78. Cilli R, Prakki A, de Araújo PA, Pereira JC. Influence of glutaraldehyde priming on bond strength of an experimental adhesive system applied to wet and dry dentine. J Dent. 2009; 37:212–218. PMID:
19124185.

79. Chiang YS, Chen YL, Chuang SF, Wu CM, Wei PJ, Han CF, Lin JC, Chang HT. Riboflavin-ultraviolet-A-induced collagen cross-linking treatments in improving dentin bonding. Dent Mater. 2013; 29:682–692. PMID:
23582694.

80. Epasinghe D, Yiu C, Burrow M. Effect of proanthocyanidin incorporation into dental adhesive on durability of resin–dentin bond. Int J Adhes Adhes. 2015; 63:145–151.

81. Bedran-Russo AK, Pashley DH, Agee K, Drummond JL, Miescke KJ. Changes in stiffness of demineralized dentin following application of collagen crosslinkers. J Biomed Mater Res B Appl Biomater. 2008; 86B:330–334.
82. Osorio R, Yamauti M, Osorio E, Ruiz-Requena ME, Pashley DH, Tay FR, Toledano M. Zinc reduces collagen degradation in demineralized human dentin explants. J Dent. 2011; 39:148–153. PMID:
21108986.

83. Osorio R, Osorio E, Medina-Castillo AL, Toledano M. Polymer nanocarriers for dentin adhesion. J Dent Res. 2014; 93:1258–1263. PMID:
25227634.

84. Santamaria S, Nuti E, Cercignani G, La Regina G, Silvestri R, Supuran CT, Rossello A. Kinetic characterization of 4,4′-biphenylsulfonamides as selective non-zinc binding MMP inhibitors. J Enzyme Inhib Med Chem. 2015; 30:947–954. PMID:
25694065.

85. Tezvergil-Mutluay A, Mutluay MM, Agee KA, Seseogullari-Dirihan R, Hoshika T, Cadenaro M, Breschi L, Vallittu P, Tay FR, Pashley DH. Carbodiimide cross-linking inactivates soluble and matrix-bound MMPs,
in vitro
. J Dent Res. 2012; 91:192–196. PMID:
22058118.
86. Singh P, Nagpal R, Singh UP. Effect of dentin biomodifiers on the immediate and long-term bond strengths of a simplified etch and rinse adhesive to dentin. Restor Dent Endod. 2017; 42:188–199. PMID:
28808635.

87. Castellan CS, Pereira PN, Grande RH, Bedran-Russo AK. Mechanical characterization of proanthocyanidin-dentin matrix interaction. Dent Mater. 2010; 26:968–973. PMID:
20650510.

88. Chuang CH, Yeh CL, Yeh SL, Lin ES, Wang LY, Wang YH. Quercetin metabolites inhibit MMP-2 expression in A549 lung cancer cells by PPAR-γ associated mechanisms. J Nutr Biochem. 2016; 33:45–53. PMID:
27260467.

89. Gotti VB, Feitosa VP, Sauro S, Correr-Sobrinho L, Leal FB, Stansbury JW, Correr AB. Effect of antioxidants on the dentin interface bond stability of adhesives exposed to hydrolytic degradation. J Adhes Dent. 2015; 17:35–44. PMID:
25625137.
90. Monteiro TM, Basting RT, Turssi CP, França FG, Amaral FL. Influence of natural and synthetic metalloproteinase inhibitors on bonding durability of an etch-and-rinse adhesive to dentin. Int J Adhes Adhes. 2013; 47:83–88.

91. Liu Y, Tjäderhane L, Breschi L, Mazzoni A, Li N, Mao J, Pashley DH, Tay FR. Limitations in bonding to dentin and experimental strategies to prevent bond degradation. J Dent Res. 2011; 90:953–968. PMID:
21220360.

92. Fugolin AP, Dobson A, Mbiya W, Navarro O, Ferracane JL, Pfeifer CS. Use of (meth)acrylamides as alternative monomers in dental adhesive systems. Dent Mater. 2019; 35:686–696. PMID:
30826074.

93. Fugolin AP, Dobson A, Ferracane JL, Pfeifer CS. Effect of residual solvent on performance of acrylamide-containing dental materials. Dent Mater. 2019; 35:1378–1387. PMID:
31378307.

94. Tekçe N, Tuncer S, Demirci M, Balci S. Do matrix metalloproteinase inhibitors improve the bond durability of universal dental adhesives? Scanning. 2016; 38:535–544. PMID:
26763084.





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download