1. Arcaya MC, Arcaya AL, Subramanian SV. Inequalities in health: definitions, concepts, and theories. Glob Health Action. 2015; 8:27106. PMID:
26112142.

2. Murray CJ, Gakidou EE, Frenk J. Health inequalities and social group differences: what should we measure? Bull World Health Organ. 1999; 77:537–543. PMID:
10444876.
3. Braveman P, Tarimo E. Social inequalities in health within countries: not only an issue for affluent nations. Soc Sci Med. 2002; 54:1621–1635. PMID:
12113445.

4. Sen A. Why health equity? Health Econ. 2002; 11:659–666. PMID:
12457367.

5. Kim S, Song JH, Oh YM, Park SM. Disparities in the utilisation of preventive health services by the employment status: an analysis of 2007-2012 South Korean national survey. PLoS One. 2018; 13:e0207737. PMID:
30586360.

6. Kim KR, Kim MK, Shin YJ. Household food security status and its characteristics in Korea. Health Soc Welf Rev. 2009; 29:268–292.
7. Lee SH, Joh HK, Kim S, Oh SW, Lee CM, Kwon H. Income disparities in the use of health screening services among university students in Korea: a cross-sectional study of 2479 participants in a university. Medicine (Baltimore). 2016; 95:e3681. PMID:
27196475.
8. Lee H, Kim BH. Physical activity disparities by socioeconomic status among metabolic syndrome patients: The Fifth Korea National Health and Nutrition Examination Survey. J Exerc Rehabil. 2016; 12:10–14. PMID:
26933654.

9. Zhang Q, Wang Y. Using concentration index to study changes in socio-economic inequality of overweight among US adolescents between 1971 and 2002. Int J Epidemiol. 2007; 36:916–925. PMID:
17470489.

10. Kim S, Hwang J. Assessment of trends in socioeconomic inequalities in cancer screening services in Korea, 1998-2012. Int J Equity Health. 2016; 15:30. PMID:
26912345.

11. Hwang J, Lee EY, Lee CG. Measuring socioeconomic inequalities in obesity among Korean adults, 1998-2015. Int J Environ Res Public Health. 2019; 16:1617.

12. Korea Health Promotion Institute [Internet]. Seoul: Korea Health Promotion Institute;c2020. cited 2020 August 2. Available from:
https://khealth.or.kr/kps.
13. Korea Health Promotion Institute. Health Plan [Internet]. Seoul: Korea Health Promotion Institute;2020. cited 2020 August 02. Available from:
https://www.khealth.or.kr/healthplan.
14. Choi EJ. Developing Strategies for the National Health Plan 2020. Sejong: Korea Institute for Health and Social Affairs;2016.
15. Kweon S, Kim Y, Jang MJ, Kim Y, Kim K, Choi S, Chun C, Khang YH, Oh K. Data resource profile: the Korea National Health and Nutrition Examination Survey (KNHANES). Int J Epidemiol. 2014; 43:69–77. PMID:
24585853.

16. Korea Centers for Disease Control and Prevention. Korea National Health and Nutrition Examination Survey Selection of Target People [Internet]. Cheongju: Korea Centers for Disease Control and Prevention;2020. cited 2020 August 10. Available from:
https://knhanes.cdc.go.kr/knhanes/sub02/sub02_01.do.
17. World Health Organization. Definition of terms. In: Western Pacific Country Health Information Profiles: 2011 Revision. Manila: World Health Organization Western Pacific Region;2011.
18. Rural Development Administration (KR). Food Composition Table. 5th rev. ed. Suwon: Rural Development Administration;1996.
19. Rural Development Administration (KR). Food Composition Table. 6th rev. ed. Suwon: Rural Development Administration;2001.
20. Rural Development Administration (KR). Food Composition Table. 7th rev. ed. Suwon: Rural Development Administration;2006.
21. Rural Development Administration (KR). Standard Food Composition Table. 8th rev. ed. Suwon: Rural development Administration;2012.
22. Ministry of Health and Welfare (KR). The Korean Nutrition Society. Dietary Reference Intakes for Koreans 2015. Seoul: The Korean Nutrition Society;2015.
23. Pearcy JN, Keppel KG. A summary measure of health disparity. Public Health Rep. 2002; 117:273–280. PMID:
12432138.

24. O'Donnell O, Van Doorslaer E, Wagstaff A, Lindelow M. Analyzing Health Equity Using Household Survey Data: a Guide to Techniques and Their Implementation. Washington, D.C.: The World Bank;2007.
25. Clarke PM, Gerdtham UG, Johannesson M, Bingefors K, Smith L. On the measurement of relative and absolute income-related health inequality. Soc Sci Med. 2002; 55:1923–1928. PMID:
12406461.

26. O'Donnell O, O'Neill S, Van Ourti T, Walsh B. conindex: Estimation of concentration indices. Stata J. 2016; 16:112–138. PMID:
27053927.
27. Kim MY, Oh KK, Lim MK, Yun EH, Kang YH. The association of socioeconomic and psychosocial factors with obesity in a rural community. Korean J Obes. 2012; 21:18–28.

28. Korea Centers for Disease Control and Prevention. Korea Health Statistics 2018: Korea National Health and Nutrition Examination Survey (KNHANES VII-3). . Cheongju: Korea Centers for Disease Control and Prevention;2019.
29. Lee WJ, Kim HC, Oh SM, Choi DP, Cho J, Suh I. Factors associated with a low-sodium diet: the Fourth Korean National Health and Nutrition Examination Survey. Epidemiol Health. 2013; 35:e2013005. PMID:
23807908.

30. Lee KW, Song WO, Cho MS. Dietary quality differs by consumption of meals prepared at home vs. outside in Korean adults. Nutr Res Pract. 2016; 10:294–304. PMID:
27247726.

31. Wagstaff A. The bounds of the concentration index when the variable of interest is binary, with an application to immunization inequality. Health Econ. 2005; 14:429–432. PMID:
15495147.

32. Xu Y, Zhu S, Zhang T, Wang D, Hu J, Gao J, Zhou Z. Explaining income-related inequalities in dietary knowledge: evidence from the China Health and Nutrition Survey. Int J Environ Res Public Health. 2020; 17:532.

33. Yazdi-Feyzabadi V, Rashidian A, Amini Rarani M. Socio-economic inequality in unhealthy snacks consumption among adolescent students in Iran: a concentration index decomposition analysis. Public Health Nutr. 2019; 22:2179–2188. PMID:
31199208.

34. Mostafavi F, Moradi G, Azadi N, Esmaeilnasab N, Chamary M. The association of unhealthy diet with socioeconomic inequality in children: a study in Kurdistan. West of Iran. Health Scope. 2019; 8:e58336.

35. Shan Z, Li Y, Baden MY, Bhupathiraju SN, Wang DD, Sun Q, Rexrode KM, Rimm EB, Qi L, Willett WC, Manson JE, Qi Q, Hu FB. Association between healthy eating patterns and risk of cardiovascular disease. JAMA Intern Med. 2020; 180:1090–1100. PMID:
32539102.

36. Hu EA, Steffen LM, Coresh J, Appel LJ, Rebholz CM. Adherence to the Healthy Eating Index-2015 and other dietary patterns may reduce risk of cardiovascular disease, cardiovascular mortality, and all-cause mortality. J Nutr. 2020; 150:312–321. PMID:
31529069.

 = the variance in the fractional rank
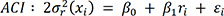
= the variance in the fractional rank = the mean level of nutrition status in the population
= the mean level of nutrition status in the population




 PDF
PDF Citation
Citation Print
Print



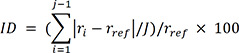 (Equation 1)
(Equation 1)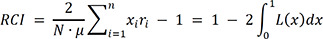 (Equation 2)
(Equation 2)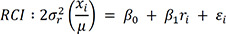
 (Equation 3)
(Equation 3)
 XML Download
XML Download