1. Crewe C, An YA, Scherer PE. The ominous triad of adipose tissue dysfunction: inflammation, fibrosis, and impaired angiogenesis. J Clin Invest. 2017; 127:74–82. PMID:
28045400.

2. Lee MJ, Wu Y, Fried SK. Adipose tissue heterogeneity: implication of depot differences in adipose tissue for obesity complications. Mol Aspects Med. 2013; 34:1–11. PMID:
23068073.

3. Shabalina IG, Petrovic N, de Jong JM, Kalinovich AV, Cannon B, Nedergaard J. UCP1 in brite/beige adipose tissue mitochondria is functionally thermogenic. Cell Reports. 2013; 5:1196–1203. PMID:
24290753.

4. Yoneshiro T, Saito M. Activation and recruitment of brown adipose tissue as anti-obesity regimens in humans. Ann Med. 2015; 47:133–141. PMID:
24901355.

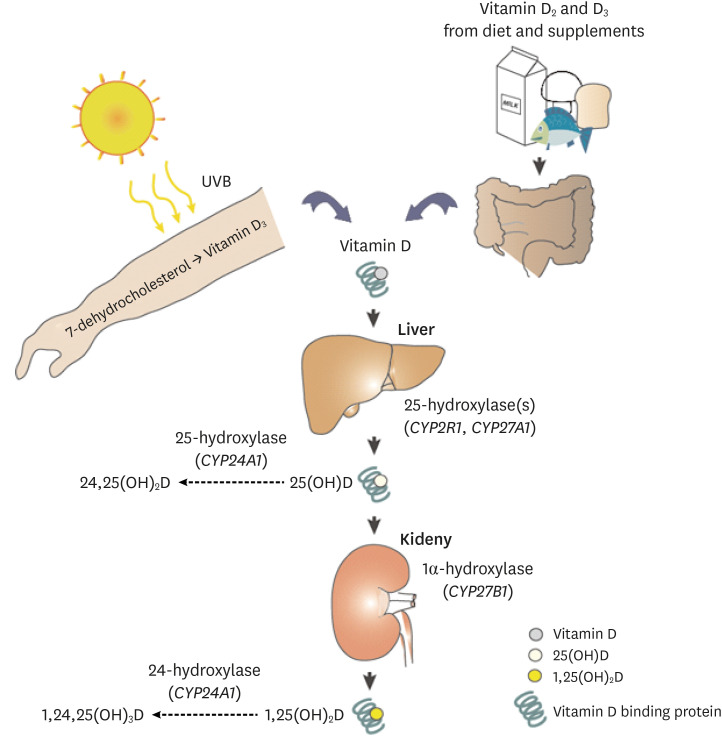
5. Umar M, Sastry KS, Chouchane AI. Role of vitamin D beyond the skeletal function: a review of the molecular and clinical studies. Int J Mol Sci. 2018; 19:1618.

6. Mutt SJ, Hyppönen E, Saarnio J, Järvelin MR, Herzig KH. Vitamin D and adipose tissue-more than storage. Front Physiol. 2014; 5:228. PMID:
25009502.

7. Thacher TD, Levine MA. CYP2R1 mutations causing vitamin D-deficiency rickets. J Steroid Biochem Mol Biol. 2017; 173:333–336. PMID:
27473561.
8. Bouillon R, Marcocci C, Carmeliet G, Bikle D, White JH, Dawson-Hughes B, Lips P, Munns CF, Lazaretti-Castro M, Giustina A, Bilezikian J. Skeletal and extraskeletal actions of vitamin D: current evidence and outstanding questions. Endocr Rev. 2019; 40:1109–1151. PMID:
30321335.

9. Fleet JC, DeSmet M, Johnson R, Li Y. Vitamin D and cancer: a review of molecular mechanisms. Biochem J. 2012; 441:61–76. PMID:
22168439.

10. Sun X, Zemel MB. Calcium and 1,25-dihydroxyvitamin D3 regulation of adipokine expression. Obesity (Silver Spring). 2007; 15:340–348. PMID:
17299106.

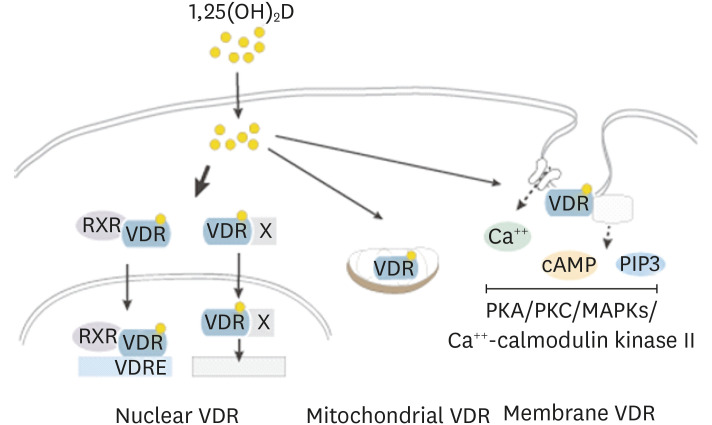
11. Hii CS, Ferrante A. The non-genomic actions of vitamin D. Nutrients. 2016; 8:135. PMID:
26950144.

12. Silvagno F, Consiglio M, Foglizzo V, Destefanis M, Pescarmona G. Mitochondrial translocation of vitamin D receptor is mediated by the permeability transition pore in human keratinocyte cell line. PLoS One. 2013; 8:e54716. PMID:
23349955.

13. Silvagno F, Pescarmona G. Spotlight on vitamin D receptor, lipid metabolism and mitochondria: Some preliminary emerging issues. Mol Cell Endocrinol. 2017; 450:24–31. PMID:
28414049.

14. Rosenstreich SJ, Rich C, Volwiler W. Deposition in and release of vitamin D
3 from body fat: evidence for a storage site in the rat. J Clin Invest. 1971; 50:679–687. PMID:
4322721.
15. Nimitphong H, Holick MF, Fried SK, Lee MJ. 25-hydroxyvitamin D
3 and 1,25-dihydroxyvitamin D
3 promote the differentiation of human subcutaneous preadipocytes. PLoS One. 2012; 7:e52171. PMID:
23272223.
16. Wamberg L, Christiansen T, Paulsen SK, Fisker S, Rask P, Rejnmark L, Richelsen B, Pedersen SB. Expression of vitamin D-metabolizing enzymes in human adipose tissue -- the effect of obesity and diet-induced weight loss. Int J Obes. 2013; 37:651–657.
17. Clemente-Postigo M, Muñoz-Garach A, Serrano M, Garrido-Sánchez L, Bernal-López MR, Fernández-García D, Moreno-Santos I, Garriga N, Castellano-Castillo D, Camargo A, Fernández-Real JM, Cardona F, Tinahones FJ, Macías-González M. Serum 25-hydroxyvitamin D and adipose tissue vitamin D receptor gene expression: relationship with obesity and type 2 diabetes. J Clin Endocrinol Metab. 2015; 100:E591–E595. PMID:
25706239.

18. Nguyen VT, Li X, Elli EF, Ayloo SM, Castellanos KJ, Fantuzzi G, Freels S, Braunschweig CL. Vitamin D, inflammation, and relations to insulin resistance in premenopausal women with morbid obesity. Obesity (Silver Spring). 2015; 23:1591–1597. PMID:
26148304.

19. Spalding KL, Arner E, Westermark PO, Bernard S, Buchholz BA, Bergmann O, Blomqvist L, Hoffstedt J, Näslund E, Britton T, Concha H, Hassan M, Rydén M, Frisén J, Arner P. Dynamics of fat cell turnover in humans. Nature. 2008; 453:783–787. PMID:
18454136.

20. Lee MJ, Wu Y, Fried SK. Adipose tissue remodeling in pathophysiology of obesity. Curr Opin Clin Nutr Metab Care. 2010; 13:371–376. PMID:
20531178.

21. Gustafson B, Hedjazifar S, Gogg S, Hammarstedt A, Smith U. Insulin resistance and impaired adipogenesis. Trends Endocrinol Metab. 2015; 26:193–200. PMID:
25703677.

22. Lee MJ, Pickering RT, Shibad V, Wu Y, Karastergiou K, Jager M, Layne MD, Fried SK. Impaired glucocorticoid suppression of TGFβ signaling in human omental adipose tissues limits adipogenesis and may promote fibrosis. Diabetes. 2019; 68:587–597. PMID:
30530781.

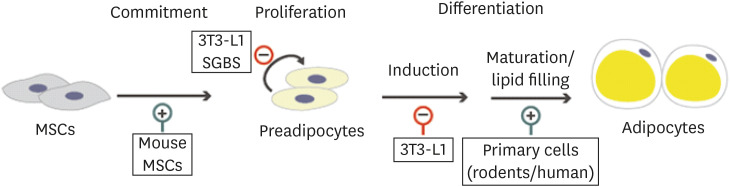
23. Lee MJ. Hormonal regulation of adipogenesis. Compr Physiol. 2017; 7:1151–1195. PMID:
28915322.

24. Blumberg JM, Tzameli I, Astapova I, Lam FS, Flier JS, Hollenberg AN. Complex role of the vitamin D receptor and its ligand in adipogenesis in 3T3-L1 cells. J Biol Chem. 2006; 281:11205–11213. PMID:
16467308.

25. Kong J, Li YC. Molecular mechanism of 1,25-dihydroxyvitamin D
3 inhibition of adipogenesis in 3T3-L1 cells. Am J Physiol Endocrinol Metab. 2006; 290:E916–E924. PMID:
16368784.
26. Narvaez CJ, Simmons KM, Brunton J, Salinero A, Chittur SV, Welsh JE. Induction of STEAP4 correlates with 1,25-dihydroxyvitamin D
3 stimulation of adipogenesis in mesenchymal progenitor cells derived from human adipose tissue. J Cell Physiol. 2013; 228:2024–2036. PMID:
23553608.
27. Felicidade I, Sartori D, Coort SL, Semprebon SC, Niwa AM, D'Epiro GF, Biazi BI, Marques LA, Evelo CT, Mantovani MS, Ribeiro LR. Role of 1α,25-dihydroxyvitamin D3 in adipogenesis of SGBS cells: new insights into human preadipocyte proliferation. Cell Physiol Biochem. 2018; 48:397–408.
28. Mahajan A, Stahl CH. Dihydroxy-cholecalciferol stimulates adipocytic differentiation of porcine mesenchymal stem cells. J Nutr Biochem. 2009; 20:512–520. PMID:
18789667.

29. Nobre JL, Lisboa PC, Carvalho JC, Martins MR, Vargas S, Barja-Fidalgo C, de Moura EG, de Oliveira E. Leptin blocks the inhibitory effect of vitamin D on adipogenesis and cell proliferation in 3T3-L1 adipocytes. Gen Comp Endocrinol. 2018; 266:1–8. PMID:
29339180.

30. Shi H, Norman AW, Okamura WH, Sen A, Zemel MB. 1α,25-Dihydroxyvitamin D
3 modulates human adipocyte metabolism via nongenomic action. FASEB J. 2001; 15:2751–2753. PMID:
11606486.
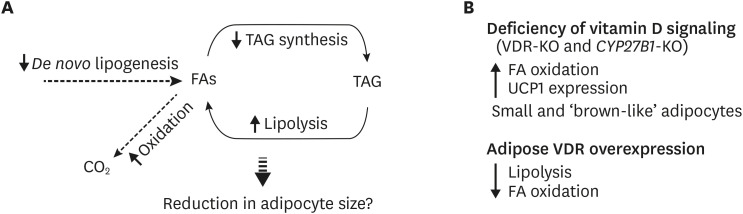
31. Wong KE, Szeto FL, Zhang W, Ye H, Kong J, Zhang Z, Sun XJ, Li YC. Involvement of the vitamin D receptor in energy metabolism: regulation of uncoupling proteins. Am J Physiol Endocrinol Metab. 2009; 296:E820–8. PMID:
19176352.

32. Narvaez CJ, Matthews D, Broun E, Chan M, Welsh J. Lean phenotype and resistance to diet-induced obesity in vitamin D receptor knockout mice correlates with induction of uncoupling protein-1 in white adipose tissue. Endocrinology. 2009; 150:651–661. PMID:
18845643.

33. Matthews DG, D'Angelo J, Drelich J, Welsh J. Adipose-specific VDR deletion alters body fat and enhances mammary epithelial density. J Steroid Biochem Mol Biol. 2016; 164:299–308. PMID:
26429395.

34. Wong KE, Kong J, Zhang W, Szeto FL, Ye H, Deb DK, Brady MJ, Li YC. Targeted expression of human vitamin D receptor in adipocytes decreases energy expenditure and induces obesity in mice. J Biol Chem. 2011; 286:33804–33810. PMID:
21840998.

35. Schutkowski A, Max D, Bönn M, Brandsch C, Grundmann SM, Hirche F, Staege MS, Stangl GI. Vitamin D does not play a functional role in adipose tissue development in rodent models. Mol Nutr Food Res. 2018; 62:62.

36. Belenchia AM, Jones KL, Will M, Beversdorf DQ, Vieira-Potter V, Rosenfeld CS, Peterson CA. Maternal vitamin D deficiency during pregnancy affects expression of adipogenic-regulating genes peroxisome proliferator-activated receptor gamma (PPARγ) and vitamin D receptor (VDR) in lean male mice offspring. Eur J Nutr. 2018; 57:723–730. PMID:
28004271.

37. Chang E, Kim Y. Vitamin D decreases adipocyte lipid storage and increases NAD-SIRT1 pathway in 3T3-L1 adipocytes. Nutrition. 2016; 32:702–708. PMID:
26899162.

38. Larrick BM, Kim KH, Donkin SS, Teegarden D. 1,25-Dihydroxyvitamin D regulates lipid metabolism and glucose utilization in differentiated 3T3-L1 adipocytes. Nutr Res. 2018; 58:72–83. PMID:
30340817.

39. Bhat M, Noolu B, Qadri SS, Ismail A. Vitamin D deficiency decreases adiposity in rats and causes altered expression of uncoupling proteins and steroid receptor coactivator3. J Steroid Biochem Mol Biol. 2014; 144 Pt B:304–312. PMID:
25132457.

40. Marcotorchino J, Gouranton E, Romier B, Tourniaire F, Astier J, Malezet C, Amiot MJ, Landrier JF. Vitamin D reduces the inflammatory response and restores glucose uptake in adipocytes. Mol Nutr Food Res. 2012; 56:1771–1782. PMID:
23065818.

41. Manna P, Jain SK. Vitamin D up-regulates glucose transporter 4 (GLUT4) translocation and glucose utilization mediated by cystathionine-γ-lyase (CSE) activation and H2S formation in 3T3L1 adipocytes. J Biol Chem. 2012; 287:42324–42332. PMID:
23074218.

42. Manna P, Achari AE, Jain SK. Vitamin D supplementation inhibits oxidative stress and upregulate SIRT1/AMPK/GLUT4 cascade in high glucose-treated 3T3L1 adipocytes and in adipose tissue of high fat diet-fed diabetic mice. Arch Biochem Biophys. 2017; 615:22–34. PMID:
28063949.

43. Sun X, Morris KL, Zemel MB. Role of calcitriol and cortisol on human adipocyte proliferation and oxidative and inflammatory stress: a microarray study. J Nutrigenet Nutrigenomics. 2008; 1:30–48. PMID:
19918113.

44. Lorente-Cebrián S, Eriksson A, Dunlop T, Mejhert N, Dahlman I, Aström G, Sjölin E, Wåhlén K, Carlberg C, Laurencikiene J, Hedén P, Arner P, Rydén M. Differential effects of 1α,25-dihydroxycholecalciferol on MCP-1 and adiponectin production in human white adipocytes. Eur J Nutr. 2012; 51:335–342. PMID:
21701898.

45. Wamberg L, Cullberg KB, Rejnmark L, Richelsen B, Pedersen SB. Investigations of the anti-inflammatory effects of vitamin D in adipose tissue: results from an
in vitro study and a randomized controlled trial. Horm Metab Res. 2013; 45:456–462. PMID:
23322512.
46. Ding C, Wilding JP, Bing C. 1,25-Dihydroxyvitamin D
3 protects against macrophage-induced activation of NFκB and MAPK signalling and chemokine release in human adipocytes. PLoS One. 2013; 8:e61707. PMID:
23637889.
47. Gao D, Trayhurn P, Bing C. 1,25-Dihydroxyvitamin D3 inhibits the cytokine-induced secretion of MCP-1 and reduces monocyte recruitment by human preadipocytes. Int J Obes. 2013; 37:357–365.
48. Karkeni E, Marcotorchino J, Tourniaire F, Astier J, Peiretti F, Darmon P, Landrier JF. Vitamin D limits chemokine expression in adipocytes and macrophage migration
in vitro and in male mice. Endocrinology. 2015; 156:1782–1793. PMID:
25730105.
49. Kaneko I, Sabir MS, Dussik CM, Whitfield GK, Karrys A, Hsieh JC, Haussler MR, Meyer MB, Pike JW, Jurutka PW. 1,25-Dihydroxyvitamin D regulates expression of the tryptophan hydroxylase 2 and leptin genes: implication for behavioral influences of vitamin D. FASEB J. 2015; 29:4023–4035. PMID:
26071405.

50. Kong J, Chen Y, Zhu G, Zhao Q, Li YC. 1,25-Dihydroxyvitamin D
3 upregulates leptin expression in mouse adipose tissue. J Endocrinol. 2013; 216:265–271. PMID:
23160964.
51. Sun J, Kong J, Duan Y, Szeto FL, Liao A, Madara JL, Li YC. Increased NF-κB activity in fibroblasts lacking the vitamin D receptor. Am J Physiol Endocrinol Metab. 2006; 291:E315–22. PMID:
16507601.

52. Zhang Y, Leung DY, Richers BN, Liu Y, Remigio LK, Riches DW, Goleva E. Vitamin D inhibits monocyte/macrophage proinflammatory cytokine production by targeting MAPK phosphatase-1. J Immunol. 2012; 188:2127–2135. PMID:
22301548.

53. Chun RF, Lauridsen AL, Suon L, Zella LA, Pike JW, Modlin RL, Martineau AR, Wilkinson RJ, Adams J, Hewison M. Vitamin D-binding protein directs monocyte responses to 25-hydroxy- and 1,25-dihydroxyvitamin D. J Clin Endocrinol Metab. 2010; 95:3368–3376. PMID:
20427486.

54. Christakos S, Dhawan P, Ajibade D, Benn BS, Feng J, Joshi SS. Mechanisms involved in vitamin D mediated intestinal calcium absorption and in non-classical actions of vitamin D. J Steroid Biochem Mol Biol. 2010; 121:183–187. PMID:
20214989.

55. Jamka M, Woźniewicz M, Walkowiak J, Bogdański P, Jeszka J, Stelmach-Mardas M. The effect of vitamin D supplementation on selected inflammatory biomarkers in obese and overweight subjects: a systematic review with meta-analysis. Eur J Nutr. 2016; 55:2163–2176. PMID:
26538075.

56. Dinca M, Serban MC, Sahebkar A, Mikhailidis DP, Toth PP, Martin SS, Blaha MJ, Blüher M, Gurban C, Penson P, Michos ED, Hernandez AV, Jones SR, Banach M. Lipid Blood Pressure Meta-analysis Collaboration LBPMC Group. Does vitamin D supplementation alter plasma adipokines concentrations? A systematic review and meta-analysis of randomized controlled trials. Pharmacol Res. 2016; 107:360–371. PMID:
27038530.

57. Hajimohammadi M, Shab-Bidar S, Neyestani TR. Vitamin D and serum leptin: a systematic review and meta-analysis of observational studies and randomized controlled trials. Eur J Clin Nutr. 2017; 71:1144–1153. PMID:
27966571.

58. Yu Y, Tian L, Xiao Y, Huang G, Zhang M. Effect of vitamin D supplementation on some inflammatory biomarkers in type 2 diabetes mellitus subjects: a systematic review and meta-analysis of randomized controlled trials. Ann Nutr Metab. 2018; 73:62–73. PMID:
29945132.

59. Romagnoli E, Pepe J, Piemonte S, Cipriani C, Minisola S. Management of endocrine disease: value and limitations of assessing vitamin D nutritional status and advised levels of vitamin D supplementation. Eur J Endocrinol. 2013; 169:R59–69. PMID:
23847326.

60. Ross AC, Manson JE, Abrams SA, Aloia JF, Brannon PM, Clinton SK, Durazo-Arvizu RA, Gallagher JC, Gallo RL, Jones G, Kovacs CS, Mayne ST, Rosen CJ, Shapses SA. The 2011 report on dietary reference intakes for calcium and vitamin D from the Institute of Medicine: what clinicians need to know. J Clin Endocrinol Metab. 2011; 96:53–58. PMID:
21118827.

61. Cosman F, de Beur SJ, LeBoff MS, Lewiecki EM, Tanner B, Randall S, Lindsay R. National Osteoporosis Foundation. Clinician's guide to prevention and treatment of osteoporosis. Osteoporos Int. 2014; 25:2359–2381. PMID:
25182228.

62. Dawson-Hughes B, Mithal A, Bonjour JP, Boonen S, Burckhardt P, Fuleihan GE, Josse RG, Lips P, Morales-Torres J, Yoshimura N. IOF position statement: vitamin D recommendations for older adults. Osteoporos Int. 2010; 21:1151–1154. PMID:
20422154.

63. Lenders CM, Feldman HA, Von Scheven E, Merewood A, Sweeney C, Wilson DM, Lee PD, Abrams SH, Gitelman SE, Wertz MS, Klish WJ, Taylor GA, Chen TC, Holick MF. Elizabeth Glaser Pediatric Research Network Obesity Study Group. Relation of body fat indexes to vitamin D status and deficiency among obese adolescents. Am J Clin Nutr. 2009; 90:459–467. PMID:
19640956.
64. Looker AC, Pfeiffer CM, Lacher DA, Schleicher RL, Picciano MF, Yetley EA. Serum 25-hydroxyvitamin D status of the US population: 1988-1994 compared with 2000-2004. Am J Clin Nutr. 2008; 88:1519–1527. PMID:
19064511.

65. Valiña-Tóth AL, Lai Z, Yoo W, Abou-Samra A, Gadegbeku CA, Flack JM. Relationship of vitamin D and parathyroid hormone with obesity and body composition in African Americans. Clin Endocrinol (Oxf). 2010; 72:595–603. PMID:
19656160.

66. Wortsman J, Matsuoka LY, Chen TC, Lu Z, Holick MF. Decreased bioavailability of vitamin D in obesity. Am J Clin Nutr. 2000; 72:690–693. PMID:
10966885.

67. Drincic AT, Armas LA, Van Diest EE, Heaney RP. Volumetric dilution, rather than sequestration best explains the low vitamin D status of obesity. Obesity (Silver Spring). 2012; 20:1444–1448. PMID:
22262154.

68. Pathak K, Soares MJ, Calton EK, Zhao Y, Hallett J. Vitamin D supplementation and body weight status: a systematic review and meta-analysis of randomized controlled trials. Obes Rev. 2014; 15:528–537. PMID:
24528624.

69. Chandler PD, Wang L, Zhang X, Sesso HD, Moorthy MV, Obi O, Lewis J, Prince RL, Danik JS, Manson JE, LeBoff MS, Song Y. Effect of vitamin D supplementation alone or with calcium on adiposity measures: a systematic review and meta-analysis of randomized controlled trials. Nutr Rev. 2015; 73:577–593. PMID:
26180255.

70. Caan B, Neuhouser M, Aragaki A, Lewis CB, Jackson R, LeBoff MS, Margolis KL, Powell L, Uwaifo G, Whitlock E, Wylie-Rosett J, LaCroix A. Calcium plus vitamin D supplementation and the risk of postmenopausal weight gain. Arch Intern Med. 2007; 167:893–902. PMID:
17502530.

71. Tuomainen TP, Virtanen JK, Voutilainen S, Nurmi T, Mursu J, de Mello VD, Schwab U, Hakumäki M, Pulkki K, Uusitupa M. Glucose metabolism effects of vitamin D in prediabetes: the VitDmet randomized placebo-controlled supplementation study. J Diabetes Res. 2015; 2015:672653. PMID:
26106626.

72. Mitchell DM, Leder BZ, Cagliero E, Mendoza N, Henao MP, Hayden DL, Finkelstein JS, Burnett-Bowie SA. Insulin secretion and sensitivity in healthy adults with low vitamin D are not affected by high-dose ergocalciferol administration: a randomized controlled trial. Am J Clin Nutr. 2015; 102:385–392. PMID:
26156733.

73. Cassity EP, Redzic M, Teager CR, Thomas DT. The effect of body composition and BMI on 25(OH)D response in vitamin D-supplemented athletes. Eur J Sport Sci. 2016; 16:773–779. PMID:
26698109.

74. Sadiya A, Ahmed SM, Carlsson M, Tesfa Y, George M, Ali SH, Siddieg HH, Abusnana S. Vitamin D
3 supplementation and body composition in persons with obesity and type 2 diabetes in the UAE: A randomized controlled double-blinded clinical trial. Clin Nutr. 2016; 35:77–82. PMID:
25892603.
75. Mousa A, Naderpoor N, de Courten MP, Teede H, Kellow N, Walker K, Scragg R, de Courten B. Vitamin D supplementation has no effect on insulin sensitivity or secretion in vitamin D-deficient, overweight or obese adults: a randomized placebo-controlled trial. Am J Clin Nutr. 2017; 105:1372–1381. PMID:
28490514.

76. Karefylakis C, Särnblad S, Ariander A, Ehlersson G, Rask E, Rask P. Effect of vitamin D supplementation on body composition and cardiorespiratory fitness in overweight men-a randomized controlled trial. Endocrine. 2018; 61:388–397. PMID:
29978375.

77. Vimaleswaran KS, Berry DJ, Lu C, Tikkanen E, Pilz S, Hiraki LT, Cooper JD, Dastani Z, Li R, Houston DK, Wood AR, Michaëlsson K, Vandenput L, Zgaga L, Yerges-Armstrong LM, McCarthy MI, Dupuis J, Kaakinen M, Kleber ME, Jameson K, Arden N, Raitakari O, Viikari J, Lohman KK, Ferrucci L, Melhus H, Ingelsson E, Byberg L, Lind L, Lorentzon M, Salomaa V, Campbell H, Dunlop M, Mitchell BD, Herzig KH, Pouta A, Hartikainen AL, Streeten EA, Theodoratou E, Jula A, Wareham NJ, Ohlsson C, Frayling TM, Kritchevsky SB, Spector TD, Richards JB, Lehtimäki T, Ouwehand WH, Kraft P, Cooper C, März W, Power C, Loos RJ, Wang TJ, Järvelin MR, Whittaker JC, Hingorani AD, Hyppönen E. Causal relationship between obesity and vitamin D status: bi-directional Mendelian randomization analysis of multiple cohorts. PLoS Med. 2013; 10:e1001383. PMID:
23393431.

78. Jamka M, Woźniewicz M, Jeszka J, Mardas M, Bogdański P, Stelmach-Mardas M. The effect of vitamin D supplementation on insulin and glucose metabolism in overweight and obese individuals: systematic review with meta-analysis. Sci Rep. 2015; 5:16142. PMID:
26543018.

79. Rejnmark L, Bislev LS, Cashman KD, Eiríksdottir G, Gaksch M, Grübler M, Grimnes G, Gudnason V, Lips P, Pilz S, van Schoor NM, Kiely M, Jorde R. Non-skeletal health effects of vitamin D supplementation: a systematic review on findings from meta-analyses summarizing trial data. PLoS One. 2017; 12:e0180512. PMID:
28686645.

80. Mirhosseini N, Vatanparast H, Mazidi M, Kimball SM. The effect of improved serum 25-hydroxyvitamin D status on glycemic control in diabetic patients: a meta-analysis. J Clin Endocrinol Metab. 2017; 102:3097–3110. PMID:
28957454.

81. Asemi Z, Foroozanfard F, Hashemi T, Bahmani F, Jamilian M, Esmaillzadeh A. Calcium plus vitamin D supplementation affects glucose metabolism and lipid concentrations in overweight and obese vitamin D deficient women with polycystic ovary syndrome. Clin Nutr. 2015; 34:586–592. PMID:
25300649.





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download