1. Condado JA, Vélez-Gimón M. Catheter-based approach to mitral regurgitation. J Interv Cardiol. 2003; 16:523–534. PMID:
14632950.

2. Condado JA, Acquatella H, Rodriguez L, Whitlow P, Vélez-Gimo M, St Goar FG. Percutaneous edge-to-edge mitral valve repair: 2-year follow-up in the first human case. Catheter Cardiovasc Interv. 2006; 67:323–325. PMID:
16419054.

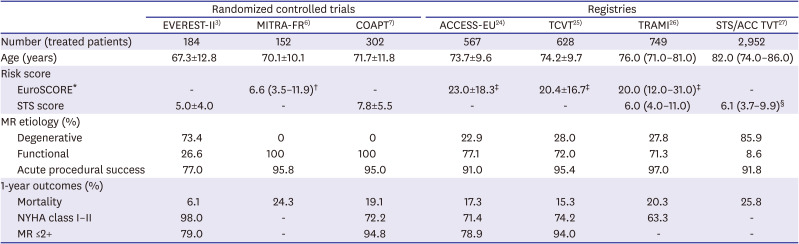
3. Feldman T, Foster E, Glower DD, et al. Percutaneous repair or surgery for mitral regurgitation. N Engl J Med. 2011; 364:1395–1406. PMID:
21463154.

4. Lim DS, Reynolds MR, Feldman T, et al. Improved functional status and quality of life in prohibitive surgical risk patients with degenerative mitral regurgitation after transcatheter mitral valve repair. J Am Coll Cardiol. 2014; 64:182–192. PMID:
24184254.

5. Glower DD, Kar S, Trento A, et al. Percutaneous mitral valve repair for mitral regurgitation in high-risk patients: results of the EVEREST II study. J Am Coll Cardiol. 2014; 64:172–181. PMID:
25011722.
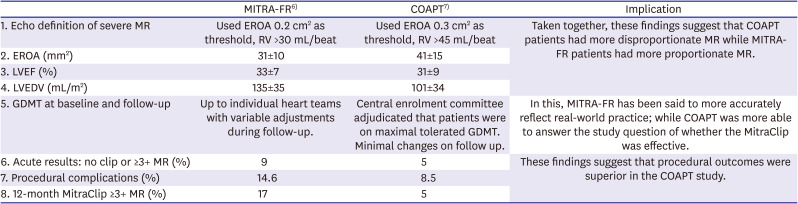
6. Obadia JF, Messika-Zeitoun D, Leurent G, et al. Percutaneous repair or medical treatment for secondary mitral regurgitation. N Engl J Med. 2018; 379:2297–2306. PMID:
30145927.

7. Stone GW, Lindenfeld J, Abraham WT, et al. Transcatheter mitral-valve repair in patients with heart failure. N Engl J Med. 2018; 379:2307–2318. PMID:
30280640.

8. Feldman T, Kar S, Rinaldi M, et al. Percutaneous mitral repair with the MitraClip system: safety and midterm durability in the initial EVEREST (Endovascular Valve Edge-to-Edge REpair Study) cohort. J Am Coll Cardiol. 2009; 54:686–694. PMID:
19679246.
9. Feldman T, Wasserman HS, Herrmann HC, et al. Percutaneous mitral valve repair using the edge-to-edge technique: six-month results of the EVEREST Phase I Clinical Trial. J Am Coll Cardiol. 2005; 46:2134–2140. PMID:
16325053.
10. Rogers JH, Franzen O. Percutaneous edge-to-edge MitraClip therapy in the management of mitral regurgitation. Eur Heart J. 2011; 32:2350–2357. PMID:
21606080.

11. Feldman T, Fernandes E, Levisay JP. Transcatheter mitral valve repair/replacement for primary mitral regurgitation. Ann Cardiothorac Surg. 2018; 7:755–763. PMID:
30598889.

12. Nishimura RA, Otto CM, Bonow RO, et al. 2014 AHA/ACC guideline for the management of patients with valvular heart disease: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014; 63:2438–2488. PMID:
24603192.
13. Nishimura RA, Otto CM, Bonow RO, et al. 2014 AHA/ACC guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014; 129:e521–643. PMID:
24589853.

14. Stone GW, Weissman NJ, Mack MJ. COAPT Investigators. Transcatheter mitral-valve repair in patients with heart failure. Reply. N Engl J Med. 2019; 380:1980–1981. PMID:
31091394.
15. Obadia JF, Armoiry X, Iung B, et al. The MITRA-FR study: design and rationale of a randomised study of percutaneous mitral valve repair compared with optimal medical management alone for severe secondary mitral regurgitation. EuroIntervention. 2015; 10:1354–1360. PMID:
25798568.

16. Vahanian A, Alfieri O, Andreotti F, et al. Guidelines on the management of valvular heart disease (version 2012): the Joint Task Force on the Management of Valvular Heart Disease of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS). Eur J Cardiothorac Surg. 2012; 42:S1–44. PMID:
22922698.
17. Baumgartner H, Falk V, Bax JJ, et al. 2017 ESC/EACTS guidelines for the management of valvular heart disease. Eur Heart J. 2017; 38:2739–2791. PMID:
28886619.
18. Mack MJ, Abraham WT, Lindenfeld J, et al. Cardiovascular outcomes assessment of the MitraClip in patients with heart failure and secondary mitral regurgitation: design and rationale of the COAPT trial. Am Heart J. 2018; 205:1–11. PMID:
30134187.

19. Grayburn PA, Sannino A, Packer M. Proportionate and disproportionate functional mitral regurgitation: a new conceptual framework that reconciles the results of the MITRA-FR and COAPT trials. JACC Cardiovasc Imaging. 2019; 12:353–362. PMID:
30553663.
20. Grayburn PA, Carabello B, Hung J, et al. Defining “severe” secondary mitral regurgitation: emphasizing an integrated approach. J Am Coll Cardiol. 2014; 64:2792–2801. PMID:
25541133.
21. Zoghbi WA, Enriquez-Sarano M, Foster E, et al. Recommendations for evaluation of the severity of native valvular regurgitation with two-dimensional and Doppler echocardiography. J Am Soc Echocardiogr. 2003; 16:777–802. PMID:
12835667.

22. Grayburn PA, Weissman NJ, Zamorano JL. Quantitation of mitral regurgitation. Circulation. 2012; 126:2005–2017. PMID:
23071176.

23. Asch FM, Grayburn PA, Siegel RJ, et al. Echocardiographic outcomes after transcatheter leaflet approximation in patients with secondary mitral regurgitation: the COAPT trial. J Am Coll Cardiol. 2019; 74:2969–2979. PMID:
31574303.
24. Maisano F, Franzen O, Baldus S, et al. Percutaneous mitral valve interventions in the real world: early and 1-year results from the ACCESS-EU, a prospective, multicenter, nonrandomized post-approval study of the MitraClip therapy in Europe. J Am Coll Cardiol. 2013; 62:1052–1061. PMID:
23747789.
25. Nickenig G, Estevez-Loureiro R, Franzen O, et al. Percutaneous mitral valve edge-to-edge repair: in-hospital results and 1-year follow-up of 628 patients of the 2011-2012 Pilot European Sentinel Registry. J Am Coll Cardiol. 2014; 64:875–884. PMID:
25169171.
26. Baldus S, Schillinger W, Franzen O, et al. MitraClip therapy in daily clinical practice: initial results from the German transcatheter mitral valve interventions (TRAMI) registry. Eur J Heart Fail. 2012; 14:1050–1055. PMID:
22685268.

27. Sorajja P, Vemulapalli S, Feldman T, et al. Outcomes with transcatheter mitral valve repair in the United States: an STS/ACC TVT registry report. J Am Coll Cardiol. 2017; 70:2315–2327. PMID:
29096801.
28. Yeo KK, Yap J, Yamen E, et al. Percutaneous mitral valve repair with the MitraClip: early results from the MitraClip Asia-Pacific Registry (MARS). EuroIntervention. 2014; 10:620–625. PMID:
24425362.

29. Tay E, Muda N, Yap J, et al. The MitraClip Asia-Pacific registry: differences in outcomes between functional and degenerative mitral regurgitation. Catheter Cardiovasc Interv. 2016; 87:E275–81. PMID:
26508564.

30. Hayashida K, Yasuda S, Matsumoto T, et al. AVJ-514 Trial - Baseline characteristics and 30-day outcomes following MitraClip
® treatment in a Japanese cohort. Circ J. 2017; 81:1116–1122. PMID:
28321004.
31. Lee CW, Sung SH, Tsai YL, et al. Initial experience with percutaneous edge-to-edge transcatheter mitral valve repair in a tertiary medical center in Taiwan. J Chin Med Assoc. 2018; 81:305–310. PMID:
29291891.

32. Wong N, Hamid N, Tang HC, Yeo KK. Killing two birds with one stone-MitraClip for flail P2 and systolic anterior motion of mitral valve: a case report. Eur Heart J Case Rep. 2018; 2:yty146. PMID:
31020221.

33. Sorajja P, Pedersen WA, Bae R, et al. First experience with percutaneous mitral valve plication as primary therapy for symptomatic obstructive hypertrophic cardiomyopathy. J Am Coll Cardiol. 2016; 67:2811–2818. PMID:
27311518.

34. Schäfer U, Frerker C, Thielsen T, et al. Targeting systolic anterior motion and left ventricular outflow tract obstruction in hypertrophic obstructed cardiomyopathy with a MitraClip. EuroIntervention. 2015; 11:942–947. PMID:
25169590.

35. Szymanski C, Levine RA, Tribouilloy C, et al. Impact of mitral regurgitation on exercise capacity and clinical outcomes in patients with ischemic left ventricular dysfunction. Am J Cardiol. 2011; 108:1714–1720. PMID:
21943932.

36. Lancellotti P, Gérard PL, Piérard LA. Long-term outcome of patients with heart failure and dynamic functional mitral regurgitation. Eur Heart J. 2005; 26:1528–1532. PMID:
15814566.

37. Lapu-Bula R, Robert A, Van Craeynest D, et al. Contribution of exercise-induced mitral regurgitation to exercise stroke volume and exercise capacity in patients with left ventricular systolic dysfunction. Circulation. 2002; 106:1342–1348. PMID:
12221050.

38. Izumo M, Suzuki K, Moonen M, et al. Changes in mitral regurgitation and left ventricular geometry during exercise affect exercise capacity in patients with systolic heart failure. Eur J Echocardiogr. 2011; 12:54–60. PMID:
20810450.

39. Masumoto A, Kubo S, Ohya M, Maruo T, Kadota K. MitraClip therapy for dynamic mitral regurgitation with repetitive heart failure exacerbation. JACC Cardiovasc Interv. 2019; 12:e215–7. PMID:
31786214.
40. Duino V, Fiocca L, Musumeci G, et al. An intriguing case report of functional mitral regurgitation treated with MitraClip. Medicine (Baltimore). 2015; 94:e608. PMID:
25997036.

41. Taramasso M, Alessandrini H, Latib A, et al. Outcomes after current transcatheter tricuspid valve intervention: mid-term results from the international TriValve registry. JACC Cardiovasc Interv. 2019; 12:155–165. PMID:
30594510.
42. Nickenig G, Weber M, Lurz P, et al. Transcatheter edge-to-edge repair for reduction of tricuspid regurgitation: 6-month outcomes of the TRILUMINATE single-arm study. Lancet. 2019; 394:2002–2011. PMID:
31708188.

43. Lim DS, Kar S, Spargias K, et al. Transcatheter valve repair for patients with mitral regurgitation: 30-day results of the CLASP study. JACC Cardiovasc Interv. 2019; 12:1369–1378. PMID:
31255562.




 PDF
PDF Citation
Citation Print
Print




 XML Download
XML Download