INTRODUCTION
Hypertension, one of the most prevalent and manageable risk factors for cardiovascular disease (CVD),
1)2)3) has been tackled in past decades by healthcare professionals both in population and high-risk approach. By introducing multidisciplinary public health programs and policies, the hypertension management status presented as awareness, treatment, and control rates have been substantially improved worldwide and also domestically.
1)4) According to the study conducted in 12 high-income countries, hypertension awareness, treatment, and control rates have increased to reach 40–80% over the last 2 decades until they became plateaued in the mid-2000s, while the prevalence has not changed a lot.
1) Given that the control rate was less than 25% in the 1980s–early 1990s in most countries, it was remarkable progress owing to the repeatedly updated hypertension management guidelines and public health programs.
3)5)6)
However, the achievement was different by age. The young adults in the US, aged 20–39 years, had a control rate of 33.0% in 2010, while the older people showed a control rate of 55.7% in 40–59 years and 54.9% in ≥60 years.
7) A study analyzing nation-wide data of China reported that the control rate was estimated 6.1–7.6% among young adults in contrast to 12.5–13.3% among elderly people.
8) The public health challenge derived from this discrepant management status between young and old hypertensive people was observed worldwide.
7)9)10)11) Even in South Korea, one of the countries with the best hypertension control,
1) both male and female young populations still have awareness and treatment rates below 50% as well as low control rates.
4) Kang et al.
11) reported that the proportion of controlled people among the hypertensive population in Korea was 9.8% among the age of 30–39 years, whereas 59.6% among 60–69 years.
If starting from a young age, hypertension could lead to life-time-long exposure to elevated blood pressure, which has been observed in previous studies that it elevated CVD risk significantly regardless of race.
12) Therefore, early intervention and management are crucial for young hypertension to prevent future adverse CVD events. Many studies have explored factors or barriers associated with hypertension awareness, treatment, and control to suggest strategies promoting hypertension management.
13)14)15) However, most studies were conducted among middle-aged to elderly hypertensive population. Therefore, we investigated factors affecting awareness, treatment, and control of hypertension, especially among the young Korean population by analyzing a national representative sample of Korea.
RESULTS
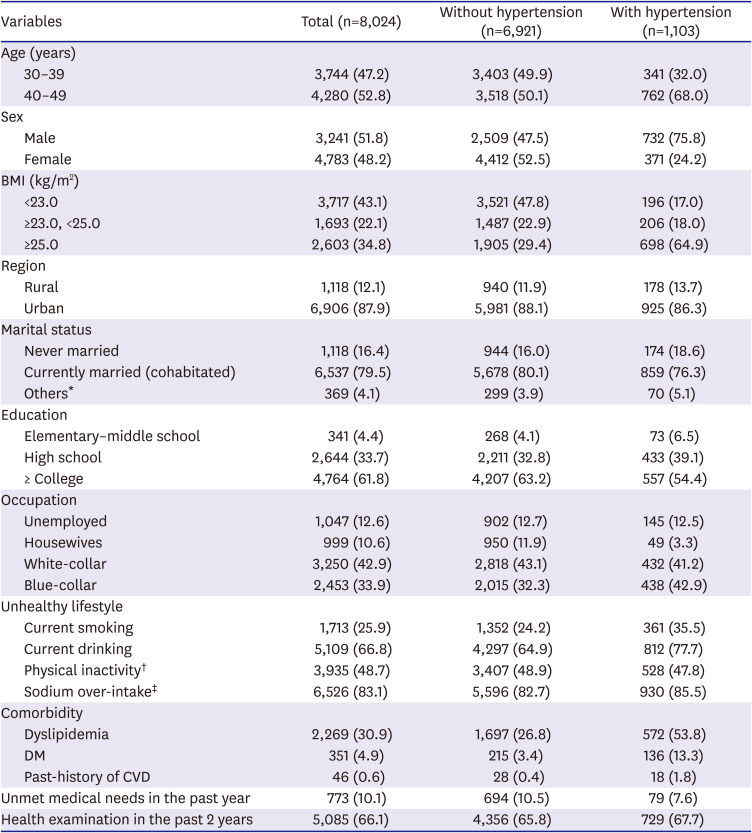
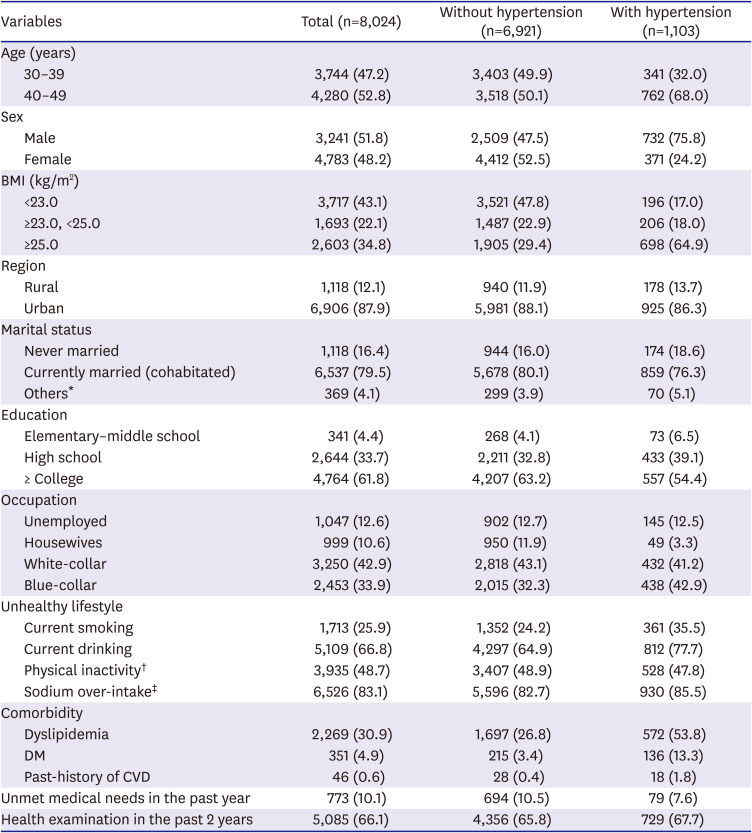
The weighted prevalence of hypertension among the age of 30–49 young Korean population was 15.2% in total (22.2% in male vs. 7.7% in female; p value for difference <0.001). This equates to an estimated 2.3 million young adults with hypertension (1.7 million male and 0.6 million female). The hypertensive participants compared to the participants without hypertension had a higher proportion of 40–49 age group, male, BMI ≥25.0 kg/m
2, current smokers, and also having other comorbid diseases (
Table 1).
Table 1
General characteristics of young (30–49 years) Korean population from KNHANES (2014–2018)
|
Variables |
Total (n=8,024) |
Without hypertension (n=6,921) |
With hypertension (n=1,103) |
|
Age (years) |
|
|
|
|
30–39 |
3,744 (47.2) |
3,403 (49.9) |
341 (32.0) |
|
40–49 |
4,280 (52.8) |
3,518 (50.1) |
762 (68.0) |
|
Sex |
|
|
|
|
Male |
3,241 (51.8) |
2,509 (47.5) |
732 (75.8) |
|
Female |
4,783 (48.2) |
4,412 (52.5) |
371 (24.2) |
|
BMI (kg/m2) |
|
|
|
|
<23.0 |
3,717 (43.1) |
3,521 (47.8) |
196 (17.0) |
|
≥23.0, <25.0 |
1,693 (22.1) |
1,487 (22.9) |
206 (18.0) |
|
≥25.0 |
2,603 (34.8) |
1,905 (29.4) |
698 (64.9) |
|
Region |
|
|
|
|
Rural |
1,118 (12.1) |
940 (11.9) |
178 (13.7) |
|
Urban |
6,906 (87.9) |
5,981 (88.1) |
925 (86.3) |
|
Marital status |
|
|
|
|
Never married |
1,118 (16.4) |
944 (16.0) |
174 (18.6) |
|
Currently married (cohabitated) |
6,537 (79.5) |
5,678 (80.1) |
859 (76.3) |
|
Others*
|
369 (4.1) |
299 (3.9) |
70 (5.1) |
|
Education |
|
|
|
|
Elementary–middle school |
341 (4.4) |
268 (4.1) |
73 (6.5) |
|
High school |
2,644 (33.7) |
2,211 (32.8) |
433 (39.1) |
|
≥ College |
4,764 (61.8) |
4,207 (63.2) |
557 (54.4) |
|
Occupation |
|
|
|
|
Unemployed |
1,047 (12.6) |
902 (12.7) |
145 (12.5) |
|
Housewives |
999 (10.6) |
950 (11.9) |
49 (3.3) |
|
White-collar |
3,250 (42.9) |
2,818 (43.1) |
432 (41.2) |
|
Blue-collar |
2,453 (33.9) |
2,015 (32.3) |
438 (42.9) |
|
Unhealthy lifestyle |
|
|
|
|
Current smoking |
1,713 (25.9) |
1,352 (24.2) |
361 (35.5) |
|
Current drinking |
5,109 (66.8) |
4,297 (64.9) |
812 (77.7) |
|
Physical inactivity†
|
3,935 (48.7) |
3,407 (48.9) |
528 (47.8) |
|
Sodium over-intake‡
|
6,526 (83.1) |
5,596 (82.7) |
930 (85.5) |
|
Comorbidity |
|
|
|
|
Dyslipidemia |
2,269 (30.9) |
1,697 (26.8) |
572 (53.8) |
|
DM |
351 (4.9) |
215 (3.4) |
136 (13.3) |
|
Past-history of CVD |
46 (0.6) |
28 (0.4) |
18 (1.8) |
|
Unmet medical needs in the past year |
773 (10.1) |
694 (10.5) |
79 (7.6) |
|
Health examination in the past 2 years |
5,085 (66.1) |
4,356 (65.8) |
729 (67.7) |
The hypertension awareness rate was 35.8% among total hypertensive participants, 33.4% in male and 43.5% in female when stratified by sex. The treatment rate and control rate were 30.9% and 23.0% respectively among hypertensive participants (28.1% and 19.3% in male, 39.8% and 34.6% in female, respectively) (
Supplementary Tables 5-
7).
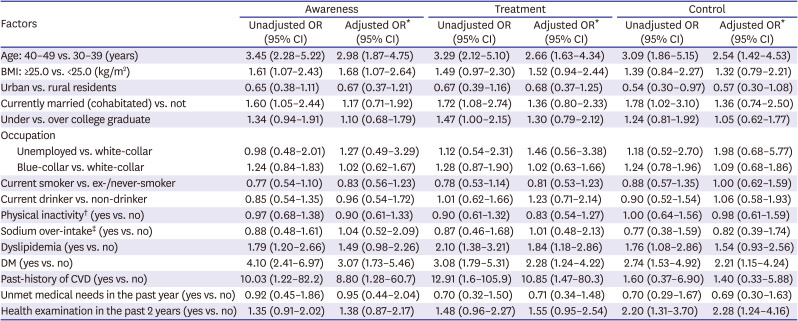
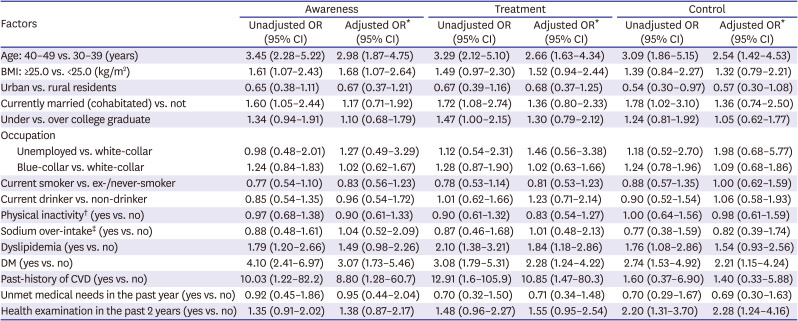
Table 2 shows the factors affecting hypertension management status among male participants. The odds of being aware of hypertension was 2.98-fold (95% CI, 1.87–4.75) higher in older (40–49 years) age group compared to younger (30–39 years) age group. The older age group also showed 2.65-fold (95% CI, 1.63–4.34) higher odds of being treated, and 2.54-fold (95% CI, 1.42–4.53) higher odds of controlling the disease compared to the younger age group. Those with higher BMI (≥25.0 kg/m
2) showed higher odds of being aware of hypertension (OR, 1.68; 95% CI, 1.07–2.64) and being treated (OR, 1.52; 95% CI, 0.94–2.44), but the control rate was not significantly higher than the lower BMI (<25.0 kg/m
2) group. Marital status was associated with hypertension management status in a crude model, but not statistically significant after covariates adjustment. Having DM was associated with a higher awareness rate (OR, 3.07; 95% CI, 1.73–5.46), treatment rate (OR, 2.28; 95% CI, 1.24–4.22), and control rate (OR, 2.24; 95% CI, 1.15–4.24). The male participants with past-history of CVDs were more likely to be aware (OR, 8.80; 95% CI, 1.28–60.67) of hypertension and to be treated (OR, 10.85; 95% CI, 1.47–80.26), but not to be controlled (OR, 1.40; 95% CI, 0.33–5.88). Those who have got health examination in the past 2 years showed a significantly higher control rate (OR, 2.28; 95% CI, 1.24–4.16) compared to those who have not.
Table 2
Factors affecting hypertension awareness, treatment, and control rate among young (30–49 years) Korean males
|
Factors |
Awareness |
Treatment |
Control |
|
Unadjusted OR (95% CI) |
Adjusted OR* (95% CI) |
Unadjusted OR (95% CI) |
Adjusted OR* (95% CI) |
Unadjusted OR (95% CI) |
Adjusted OR* (95% CI) |
|
Age: 40–49 vs. 30–39 (years) |
3.45 (2.28–5.22) |
2.98 (1.87–4.75) |
3.29 (2.12–5.10) |
2.66 (1.63–4.34) |
3.09 (1.86–5.15) |
2.54 (1.42–4.53) |
|
BMI: ≥25.0 vs. <25.0 (kg/m2) |
1.61 (1.07–2.43) |
1.68 (1.07–2.64) |
1.49 (0.97–2.30) |
1.52 (0.94–2.44) |
1.39 (0.84–2.27) |
1.32 (0.79–2.21) |
|
Urban vs. rural residents |
0.65 (0.38–1.11) |
0.67 (0.37–1.21) |
0.67 (0.39–1.16) |
0.68 (0.37–1.25) |
0.54 (0.30–0.97) |
0.57 (0.30–1.08) |
|
Currently married (cohabitated) vs. not |
1.60 (1.05–2.44) |
1.17 (0.71–1.92) |
1.72 (1.08–2.74) |
1.36 (0.80–2.33) |
1.78 (1.02–3.10) |
1.36 (0.74–2.50) |
|
Under vs. over college graduate |
1.34 (0.94–1.91) |
1.10 (0.68–1.79) |
1.47 (1.00–2.15) |
1.30 (0.79–2.12) |
1.24 (0.81–1.92) |
1.05 (0.62–1.77) |
|
Occupation |
|
|
|
|
|
|
|
Unemployed vs. white-collar |
0.98 (0.48–2.01) |
1.27 (0.49–3.29) |
1.12 (0.54–2.31) |
1.46 (0.56–3.38) |
1.18 (0.52–2.70) |
1.98 (0.68–5.77) |
|
Blue-collar vs. white-collar |
1.24 (0.84–1.83) |
1.02 (0.62–1.67) |
1.28 (0.87–1.90) |
1.02 (0.63–1.66) |
1.24 (0.78–1.96) |
1.09 (0.68–1.86) |
|
Current smoker vs. ex-/never-smoker |
0.77 (0.54–1.10) |
0.83 (0.56–1.23) |
0.78 (0.53–1.14) |
0.81 (0.53–1.23) |
0.88 (0.57–1.35) |
1.00 (0.62–1.59) |
|
Current drinker vs. non-drinker |
0.85 (0.54–1.35) |
0.96 (0.54–1.72) |
1.01 (0.62–1.66) |
1.23 (0.71–2.14) |
0.90 (0.52–1.54) |
1.06 (0.58–1.93) |
|
Physical inactivity† (yes vs. no) |
0.97 (0.68–1.38) |
0.90 (0.61–1.33) |
0.90 (0.61–1.32) |
0.83 (0.54–1.27) |
1.00 (0.64–1.56) |
0.98 (0.61–1.59) |
|
Sodium over-intake‡ (yes vs. no) |
0.88 (0.48–1.61) |
1.04 (0.52–2.09) |
0.87 (0.46–1.68) |
1.01 (0.48–2.13) |
0.77 (0.38–1.59) |
0.82 (0.39–1.74) |
|
Dyslipidemia (yes vs. no) |
1.79 (1.20–2.66) |
1.49 (0.98–2.26) |
2.10 (1.38–3.21) |
1.84 (1.18–2.86) |
1.76 (1.08–2.86) |
1.54 (0.93–2.56) |
|
DM (yes vs. no) |
4.10 (2.41–6.97) |
3.07 (1.73–5.46) |
3.08 (1.79–5.31) |
2.28 (1.24–4.22) |
2.74 (1.53–4.92) |
2.21 (1.15–4.24) |
|
Past-history of CVD (yes vs. no) |
10.03 (1.22–82.2) |
8.80 (1.28–60.7) |
12.91 (1.6–105.9) |
10.85 (1.47–80.3) |
1.60 (0.37–6.90) |
1.40 (0.33–5.88) |
|
Unmet medical needs in the past year (yes vs. no) |
0.92 (0.45–1.86) |
0.95 (0.44–2.04) |
0.70 (0.32–1.50) |
0.71 (0.34–1.48) |
0.70 (0.29–1.67) |
0.69 (0.30–1.63) |
|
Health examination in the past 2 years (yes vs. no) |
1.35 (0.91–2.02) |
1.38 (0.87–2.17) |
1.48 (0.96–2.27) |
1.55 (0.95–2.54) |
2.20 (1.31–3.70) |
2.28 (1.24–4.16) |
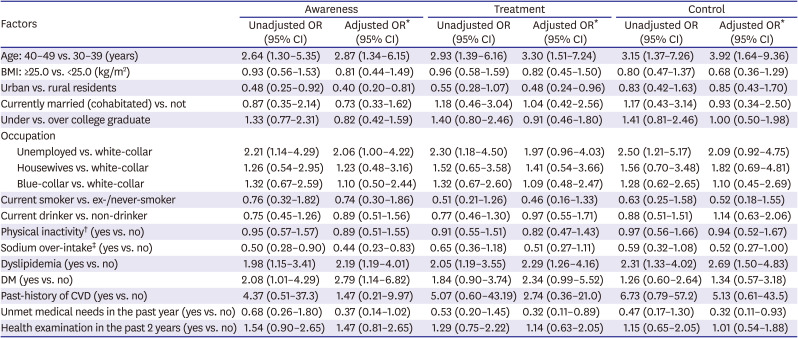
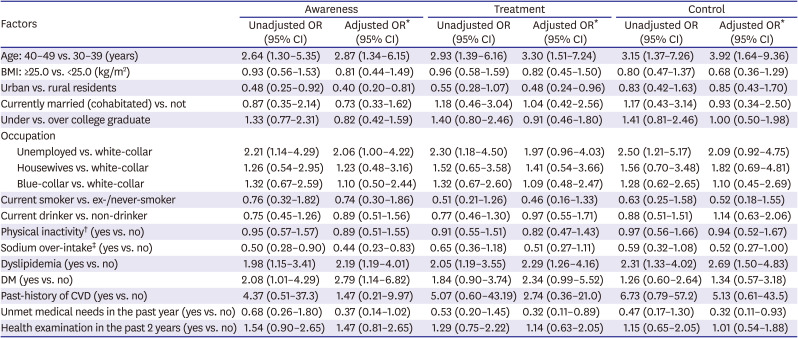
The factors affecting hypertension management among female participants were presented in
Table 3. The older (40–49 years) age group showed higher odds of being aware (OR, 2.87; 95% CI, 1.34–6.15), being treated (OR, 3.30; 95% CI, 1.51–7.24), and being controlled of hypertension (OR, 3.92; 95% CI, 1.64–9.36). The participants living in urban areas had a lower OR of awareness (OR, 0.40; 95% CI, 0.20–0.81) and treatment (OR, 0.48; 95% CI, 0.24–0.96) compared to those residing in rural areas. Unemployed participants showed significantly higher odds of awareness (OR, 2.06; 95% CI, 1.00–4.22), treatment (OR, 1.97; 95% CI, 0.96–4.03), and control (OR, 2.09; 95% CI, 0.92–4.75) than female white-collar workers. Females who reported to take sodium more than the recommendation for daily intake
20) had a lower likelihood of being aware (OR, 0.44; 95% CI, 0.23–0.83), control (OR, 0.52; 95% CI, 0.27–1.00) of hypertension. The participants with dyslipidemia showed a higher likelihood of controlling the disease with OR of 2.19; 95% CI, 1.19–4.01; as well as of being aware of and being treated. Having DM was associated with a higher awareness rate (OR, 2.79; 95% CI, 1.11–6.82), treatment rate (OR, 2.34; 95% CI, 0.99–5.52) similar to male participants, but not control rate (OR, 1.34; 95% CI, 0.57–3.18). Those who had experienced unmet medical needs in the past year were less likely to be aware (OR, 0.37; 95% CI, 0.14–1.02), to be treated (OR, 0.32; 95% CI, 0.11–0.89), and to be controlled (OR, 0.32; 95% CI, 0.11–0.93) of hypertension.
Table 3
Factors affecting hypertension awareness, treatment, and control rate among young (30–49 years) Korean females
|
Factors |
Awareness |
Treatment |
Control |
|
Unadjusted OR (95% CI) |
Adjusted OR* (95% CI) |
Unadjusted OR (95% CI) |
Adjusted OR* (95% CI) |
Unadjusted OR (95% CI) |
Adjusted OR* (95% CI) |
|
Age: 40–49 vs. 30–39 (years) |
2.64 (1.30–5.35) |
2.87 (1.34–6.15) |
2.93 (1.39–6.16) |
3.30 (1.51–7.24) |
3.15 (1.37–7.26) |
3.92 (1.64–9.36) |
|
BMI: ≥25.0 vs. <25.0 (kg/m2) |
0.93 (0.56–1.53) |
0.81 (0.44–1.49) |
0.96 (0.58–1.59) |
0.82 (0.45–1.50) |
0.80 (0.47–1.37) |
0.68 (0.36–1.29) |
|
Urban vs. rural residents |
0.48 (0.25–0.92) |
0.40 (0.20–0.81) |
0.55 (0.28–1.07) |
0.48 (0.24–0.96) |
0.83 (0.42–1.63) |
0.85 (0.43–1.70) |
|
Currently married (cohabitated) vs. not |
0.87 (0.35–2.14) |
0.73 (0.33–1.62) |
1.18 (0.46–3.04) |
1.04 (0.42–2.56) |
1.17 (0.43–3.14) |
0.93 (0.34–2.50) |
|
Under vs. over college graduate |
1.33 (0.77–2.31) |
0.82 (0.42–1.59) |
1.40 (0.80–2.46) |
0.91 (0.46–1.80) |
1.41 (0.81–2.46) |
1.00 (0.50–1.98) |
|
Occupation |
|
|
|
|
|
|
|
Unemployed vs. white-collar |
2.21 (1.14–4.29) |
2.06 (1.00–4.22) |
2.30 (1.18–4.50) |
1.97 (0.96–4.03) |
2.50 (1.21–5.17) |
2.09 (0.92–4.75) |
|
Housewives vs. white-collar |
1.26 (0.54–2.95) |
1.23 (0.48–3.16) |
1.52 (0.65–3.58) |
1.41 (0.54–3.66) |
1.56 (0.70–3.48) |
1.82 (0.69–4.81) |
|
Blue-collar vs. white-collar |
1.32 (0.67–2.59) |
1.10 (0.50–2.44) |
1.32 (0.67–2.60) |
1.09 (0.48–2.47) |
1.28 (0.62–2.65) |
1.10 (0.45–2.69) |
|
Current smoker vs. ex-/never-smoker |
0.76 (0.32–1.82) |
0.74 (0.30–1.86) |
0.51 (0.21–1.26) |
0.46 (0.16–1.33) |
0.63 (0.25–1.58) |
0.52 (0.18–1.55) |
|
Current drinker vs. non-drinker |
0.75 (0.45–1.26) |
0.89 (0.51–1.56) |
0.77 (0.46–1.30) |
0.97 (0.55–1.71) |
0.88 (0.51–1.51) |
1.14 (0.63–2.06) |
|
Physical inactivity† (yes vs. no) |
0.95 (0.57–1.57) |
0.89 (0.51–1.55) |
0.91 (0.55–1.51) |
0.82 (0.47–1.43) |
0.97 (0.56–1.66) |
0.94 (0.52–1.67) |
|
Sodium over-intake‡ (yes vs. no) |
0.50 (0.28–0.90) |
0.44 (0.23–0.83) |
0.65 (0.36–1.18) |
0.51 (0.27–1.11) |
0.59 (0.32–1.08) |
0.52 (0.27–1.00) |
|
Dyslipidemia (yes vs. no) |
1.98 (1.15–3.41) |
2.19 (1.19–4.01) |
2.05 (1.19–3.55) |
2.29 (1.26–4.16) |
2.31 (1.33–4.02) |
2.69 (1.50–4.83) |
|
DM (yes vs. no) |
2.08 (1.01–4.29) |
2.79 (1.14–6.82) |
1.84 (0.90–3.74) |
2.34 (0.99–5.52) |
1.26 (0.60–2.64) |
1.34 (0.57–3.18) |
|
Past-history of CVD (yes vs. no) |
4.37 (0.51–37.3) |
1.47 (0.21–9.97) |
5.07 (0.60–43.19) |
2.74 (0.36–21.0) |
6.73 (0.79–57.2) |
5.13 (0.61–43.5) |
|
Unmet medical needs in the past year (yes vs. no) |
0.68 (0.26–1.80) |
0.37 (0.14–1.02) |
0.53 (0.20–1.45) |
0.32 (0.11–0.89) |
0.47 (0.17–1.30) |
0.32 (0.11–0.93) |
|
Health examination in the past 2 years (yes vs. no) |
1.54 (0.90–2.65) |
1.47 (0.81–2.65) |
1.29 (0.75–2.22) |
1.14 (0.63–2.05) |
1.15 (0.65–2.05) |
1.01 (0.54–1.88) |
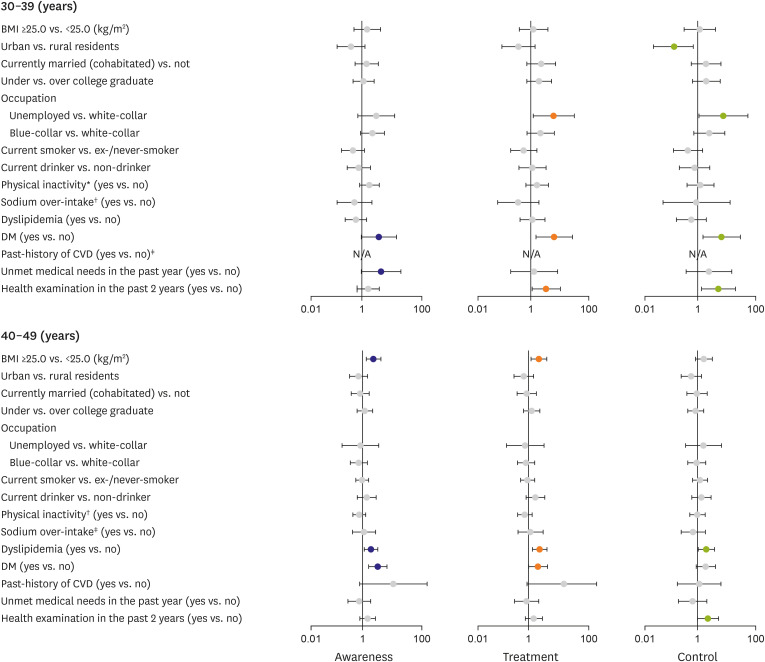
The results of stratified analysis by age group are presented in
Figures 1 and
2. Among male participants aged 30–39 years, DM, and unmet medical needs in the past year were marginally associated with a higher proportion of hypertension awareness. The unemployment, DM, and health examination in the past 2 years were associated with both higher treatment and control rates (
Figure 1;
Supplementary Table 8). Among the male participants in 40s, however, higher BMI (≥25.0 kg/m
2) and having dyslipidemia, DM had higher ORs for awareness, treatment, and control. Health examination in the past 2 years showed a higher likelihood of being controlled (
Figure 1;
Supplementary Table 9).
Figure 1
Adjusted ORs (in log-scale) stratified by age group for hypertension awareness, treatment, and control status among Korean young male adults aged 30–49 years. The ORs were adjusted for age (continuous), obesity, region, marital status, education, occupation, smoking status, drinking status, physical inactivity, sodium over-intake, dyslipidemia, DM, past history of CVD, unmet medical needs in the past year, and health examination in the past 2 years.
BMI = body mass index; CVD = cardiovascular disease; DM = diabetes mellitus; N/A = not available; OR = odds ratio.
*Defined as not participating or participating less than 150 minutes per week in moderate-to-vigorous physical activity; †Defined as taking over 2,000 mg/day; ‡The estimates were not computed due to small sample size.
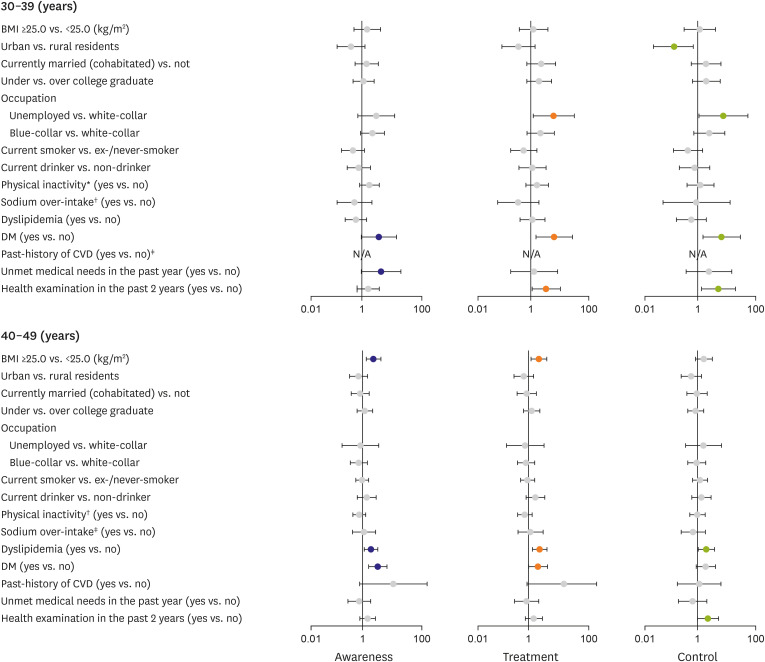
Figure 2
Adjusted ORs (in log-scale) stratified by age group for hypertension awareness, treatment, and control status among Korean young female adults aged 30–49 years. The ORs were adjusted for age (continuous), obesity, region, marital status, education, occupation, smoking status, drinking status, physical inactivity, sodium over-intake, dyslipidemia, DM, past history of CVD, unmet medical needs in the past year, and health examination in the past 2 years.
BMI = body mass index; CVD = cardiovascular disease; DM = diabetes mellitus; N/A = not available; OR = odds ratio.
*Defined as not participating or participating less than 150 minutes per week in moderate-to-vigorous physical activity; †Defined as taking over 2,000 mg/day; ‡The estimates were not computed due to small sample size.

Among female participants in the age of 30–39 years, people with higher BMI (≥25.0 kg/m
2) and unemployment were less likely to be treated. In contrast, people under-college graduates and who take sodium more than 2,000 mg/day were more likely to be treated (
Figure 2;
Supplementary Table 10). In female aged 40–49 years, urban residents showed a negative association with the awareness and treatment of hypertension. Unemployment was positively associated with higher hypertension awareness, treatment, and control. Consuming sodium more than 2,000 mg/day was associated with lower awareness, and having dyslipidemia was associated with higher awareness, treatment, and control. Having experienced unmet medical needs in the past year was associated with lower treatment among females aged 40–49 years (
Figure 2;
Supplementary Table 11).
DISCUSSION
In this representative sample of the young Korean population, we observed several factors associated with hypertension awareness, treatment, and control. The older (40≤ age <50), obese (BMI ≥25.0 kg/m2), having dyslipidemia, having DM, and having past-history of CVD participants were more likely to be aware of their hypertensive status among the young male population. Including the factors associated with higher hypertension awareness, having taken health examination in the past 2 years was positively associated with a higher treatment rate among young males. The participants who were older (40≤ age <50), having DM, and having taken health examination in the past 2 years were more controlled of hypertension among young males.
Among young female participants, older age (40≤ age <50), rural residency, unemployment, not taking sodium over recommended daily amount, having dyslipidemia, and having DM were associated with a higher likelihood of being aware of hypertension. The factors associated with higher awareness except sodium intake were positively associated with a higher treatment rate and not having experience of unmet medical needs in the past year was also positively associated. The female participants who were older (40≤ age <50), unemployed, not taking sodium over daily recommendation amount, having dyslipidemia, and not having experienced unmet medical needs in the past year were more likely to be controlled of hypertension.
The improvement of hypertension management status among young hypertension has been challenged due to the young population's lack of healthcare use, lack of knowledge, and their neglect of health management.
12)14)24) The age factor among young hypertension has been indicated the strongest challenging in relation to hypertension awareness and treatment.
11)14)25) In the study conducted by Wu et al.,
25) younger than 40 years of age group had 2-folds lower likelihood of being treated compared to the 40–49 years age group among the young Singaporean population. Kang et al.
11) also reported that awareness and treatment rates were lower in the 30–39 years-age group than the 40–49 years-age group (20.2% vs. 43.9% of awareness rate; 15.2% vs. 39.5% of treatment rate in the 30s vs. 40s, respectively). They suggested that younger people would have had lesser symptoms and comorbid diseases, which made them less recognize the dangers of the disease. In this study, we also observed that 40–49 years-age group had around 3-folds higher likelihood of being aware and treated in both males and females compared to the 30–39 years-age group.
When stratified the analysis by age, we found that the factors associated with hypertension management were different by the age group. Having DM was positively associated with awareness, treatment, and control of hypertension among males regardless of age group. Unlike the males in the 30s, however, the obese males (BMI ≥25.0 kg/m2) compared to not obese males were more aware, treated, and controlled of hypertension among the males in the 40s. Taking health examination in the past 2 years and unemployment were the factors increasing hypertension treatment and control among males in the 30s, unlike 40s. Because of the big age disproportion among hypertensive females (75 vs. 296 in 30s vs. 40s, respectively; a total of 371), the factors associated with hypertension management among young females were mostly derived from factors in the age 40s. As in total female participants, rural residency, having dyslipidemia, and unemployment enhanced hypertension awareness and treatment in females aged 40–49 years.
Having comorbid diseases such as DM, dyslipidemia, and CVD elevated the likelihood of being aware of, treated, and controlled hypertension in our study. It suggests that young people with comorbid diseases might visit clinics more frequently than people without, which led them to take care more about their hypertension status.
23)26) Females visits healthcare facilities more often than males for birth control and regular gynecological check-up.
23)27) This also explains the higher awareness (33.4% in males vs. 43.5% in females) and treatment rate (28.1% in males vs. 39.8% in females) among females in our study.
The unemployed young females in this nationally representative sample showed higher hypertension management status than female white-collar workers. The previous studies showed an inconsistent association between unemployment and hypertension management status. Li et al.
28) analyzed provincial representative samples in China and found that unemployed participants had a 1.59-fold higher likelihood of being aware of hypertension. In contrast, Satoh et al.
15) revealed that unemployed Japanese people were less likely to be aware of and treated hypertension than employed people. Unlike the previous views on the association between unemployment and hypertension management, financial barriers related to employment status would have less impact on Korean citizens thanks to the universal health coverage of South Korea.
14) We compared the characteristics of young Korean females with hypertension by employment status (
Supplementary Table 12). The unemployed young females having hypertension had less unhealthy lifestyles (fewer smokers, fewer physically inactive people, and fewer sodium over-intake people), whereas they had more comorbidities such as obesity, dyslipidemia, DM, and past-history of CVD. These factors could have led the unemployed young females with hypertension to visit more healthcare clinics more than white-collar females. Moreover, day-time deprivation due to working hours could have prevented white-collar working females from visiting healthcare clinics than unemployed females. Young adulthood is the period when people are preoccupied with their career development, which has been indicated as a determining factor in lowering hypertension management.
25) We need further in-depth observation of the association between employment status and hypertension management among the young Korean population.
To consider if difference on medication adherence by subgroup could have affected control rates, we estimated the good medication adherence, which was defined as the proportion of people taking anti-hypertensive medication every day among people who were currently taking the medication.
29) The proportion of good adherence was not significantly different by sex (94.7% in males and 94.2% in females, p value for difference=0.879). When stratified by age, the proportion was 92.4% in the 30s and 95.0% in the 40s showing no significant difference as well (p value for difference=0.824).
After the 2017 American College of Cardiology/American Heart Association (ACC/AHA) guideline had launched, the enlarged number of young hypertension and the following public health challenges have been highlighted. A previous study showed that the 2017 ACC/AHA guideline's potential impacts could be the biggest on the young adults' hypertension prevalence (21.3% in increase 30–39 years; 23.9% in 40–49 years) among the Korean population.
2) Applying the 2017 ACC/AHA guideline to hypertension management status may increase the awareness rate to 15.5%, the treatment rate to 12.4%, and the control rate to 3.3%. Broadening the diagnostic range of hypertension increases the number of young adults with uncontrolled hypertension, but the 2018 Korean Society of Hypertension Guidelines for the Management of Hypertension has maintained the diagnostic criteria of 140/90 mmHg.
2)
In our study, the factors related to enhancing attention on health conditions such as older age, obesity, comorbid diseases, or health examination, increased awareness and treatment rates among young Korean adults. Moreover, some factors partially related to more frequent clinic visits increased treatment and control rates among young Korean females. An international commission group on hypertension emphasized creating a healthy environment and health education through a life-course approach.
30) Johnson et al.
24)27) indicated that numerous life stressors and conflicting demands could have decreased visit adherence among young hypertension, especially females who are socially required to balance being a household mom with work responsibilities. Creating a more comfortable environment to seek healthcare services by alleviating such conflicting conditions could lead to young hypertension to visit clinics. Moreover, we need more practical health education programs both in school and the public level, as the young male's insufficient healthcare visit and disregard for their health have been indicated as a major barrier against hypertension management.
14)21)
This study has several limitations. Because we excluded those who missed statistical weight values in our analysis, there is a possibility of confounding by indication. However, by properly using the statistical weight to the analysis, the estimates we made can be interpreted as representative of the Korean general population. Second, there could be residual confounders or unobserved interactions between the factors. Further consideration of other additional factors or interaction between each factor needs to be drawn in the future since we simply aimed to investigate the factors associated with hypertension management in the current study. Lastly, since we conducted a cross-sectional study, factors affecting young hypertension should be explored in a longitudinal manner to see if those factors determine further disease progression in the real world.
There were previous studies investigating temporal trends of hypertension management status
10)11)22) or factors affecting the status among the overall Korean adult population.
14) However, our study exclusively focused on the young Korean population aged 30 to 49 years and the factors associated with hypertension awareness, treatment, and control, which is a rare observation using a nationally representative sample.
Among young adults with hypertension in Korea, the factors possibly enhancing young people's attention on health were associated with higher hypertension management indices. Besides, the factors indicating obstacles to visit clinics hindered hypertension treatment and control, especially among young Korean females. Considering the factors associated with hypertension awareness, treatment, and control may help establish effective strategies to improve hypertension management status among the young population.





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download