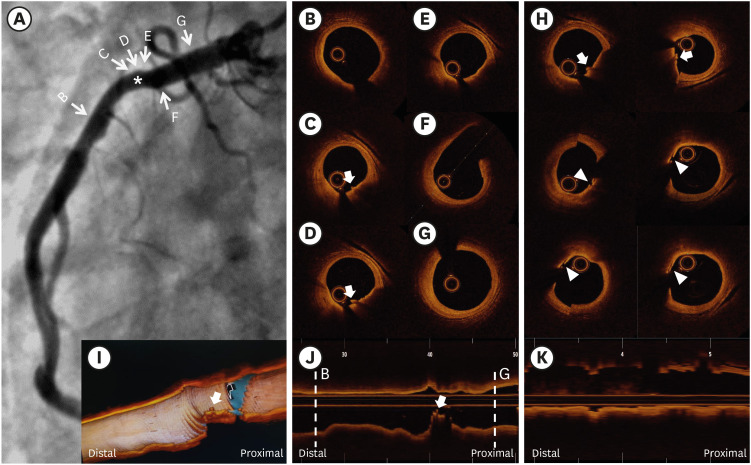
 | Figure 1(A) Diagnostic CAG showed an insignificant stenosis with vague plaque ulceration in the proximal RCA (asterisk). (B-G) Cross-sectional OCT imaging with the conventional pullback showing a white thrombus without any evidence of plaque disruption (arrow). (H) Cross-sectional OCT imaging of the ROI showing a white thrombus (arrow) and tiny plaque rupture (arrowheads). (I) Three-dimensional OCT imaging demonstrating a white thrombus (arrow), (J) Longitudinal OCT imaging of the conventional pullback showing a white thrombus (arrow). (K) Longitudinal OCT imaging using the stationary pullback.CAG = coronary angiography; OCT = optical coherence tomography; RCA = right coronary artery; ROI = region of interest.
|
A 54-year-old male was admitted to the hospital due to severe chest pain. He suffered from diabetes mellitus for 20 years and was an ex-smoker. The 12 leads electrocardiography showed ST-segment elevation in inferior leads. High sensitivity troponin level was elevated, and underwent coronary angiography. The echocardiogram showed basal inferior hypokinesia with normal left ventricular systolic function. The coronary angiography demonstrated an insignificant stenosis with vague plaque ulceration at the proximal portion of right coronary artery (Figure 1A, asterisk). The automatic motorized pullback of optical coherence tomography (OCT) was performed at 10 mm/sec with simultaneous injection of a contrast solution before the stationary imaging (SI). The minimal lumen area of the culprit lesion was measured 4.67 mm2. While a white thrombus was shown without any plaque disruption in the conventional pullback (Figure 1B-J, Supplementary Video 1), however a tiny plaque rupture (arrowhead) with the white thrombus (arrow) was clearly visible in SI (Figure 1H, Supplementary Video 2). The imaging duration was 6 seconds with 20/sec of frame rate without pulling the optical lens back in SI, however the location of an optical lens could be adjusted manually. Although the optical lens was moving by cardiac cycle and respiration, the number of acquired images (120 frames) for the region of interest was higher than with the automatic pullback (10 frames/mm). OCT is recognized as a promising, high-resolution imaging tool in coronary intervention.1)2)3) However, it often missed the target lesion unexpectedly because of a limited frame of the acquired images and cardiac motion.
References
1. Jang IK, Tearney GJ, MacNeill B, et al. In vivo characterization of coronary atherosclerotic plaque by use of optical coherence tomography. Circulation. 2005; 111:1551–1555. PMID: 15781733.

2. Kubo T, Imanishi T, Takarada S, et al. Assessment of culprit lesion morphology in acute myocardial infarction: ability of optical coherence tomography compared with intravascular ultrasound and coronary angioscopy. J Am Coll Cardiol. 2007; 50:933–939. PMID: 17765119.
3. Kwon JE, Lee WS, Mintz GS, et al. Multimodality intravascular imaging assessment of plaque erosion versus plaque rupture in patients with acute coronary syndrome. Korean Circ J. 2016; 46:499–506. PMID: 27482258.

Go to : 




 PDF
PDF Citation
Citation Print
Print




 XML Download
XML Download