INTRODUCTION
Acute myocarditis is a rare inflammatory condition of the myocardium. The spectrum of presentation can range between mild myocardial dysfunction and fulminant congestive heart failure, which causes significant morbidity and mortality. However, because of its rarity, few large-scale epidemiological studies have reported acute myocarditis in children.
1)2) Furthermore, no population-based epidemiological studies have been performed in Korea.
The Korean National Health Insurance (NHI) scheme is a public medical insurance system covering the entire Korean population. Under the NHI scheme, the Korean Health Insurance Review and Assessment Service (HIRA) evaluates the medical fees charged, the quality of care, and the adequacy of medical services rendered to each patient by recording data including diagnoses, treatments, procedures, and prescription drugs. In this study, we evaluated the 10-year (January 2007 through December 2016) epidemiological trends of acute myocarditis in Korean children by utilizing the HIRA database with the following objectives: 1) to describe the demographics of acute myocarditis in Korean children and, 2) to investigate temporal trends in the management of myocarditis in children.
Go to :

DISCUSSION
Previous research investigating epidemiology of pediatric myocarditis was based on Western population.
1) Our study is the first nationwide epidemiological study to investigate acute myocarditis in Korean children. Furthermore, our study provides comprehensive data regarding the demographic features and management of acute myocarditis in children over a 10-year period.
Several studies have reported the incidence of acute myocarditis in children. A nationwide study in Finland reported an incidence rate of 1.95 cases/100,000 person-years in children aged 0–15 years.
1) A Japanese study (based on questionnaires mailed to teaching hospitals) reported an incidence rate of 0.26 cases per 100,000 populations among children and adolescents aged 1 month–17 years.
2) Notably, the reported incidence rate varies significantly across studies,
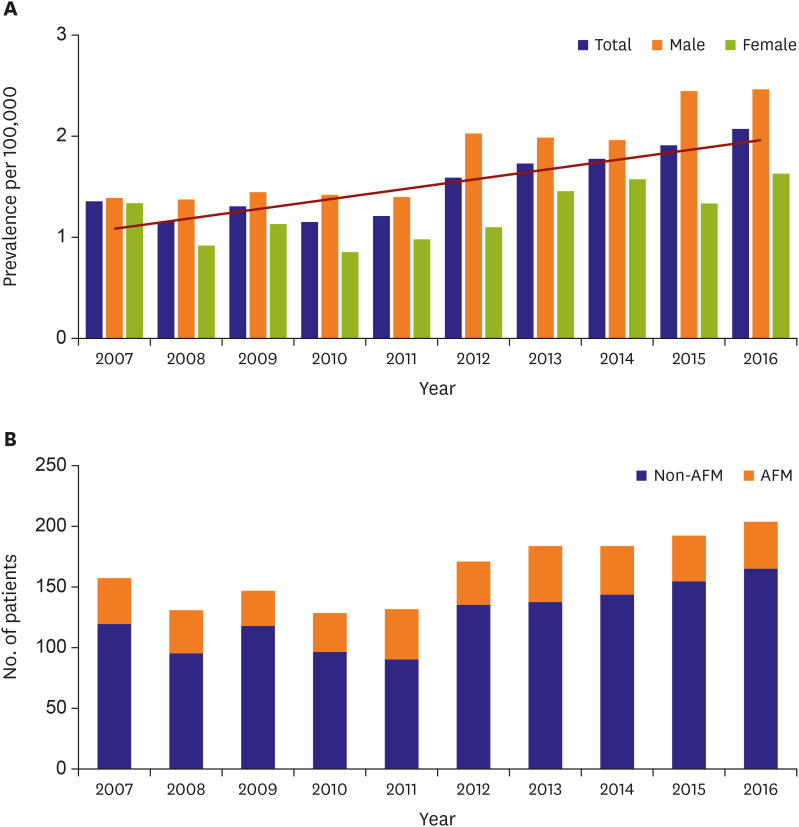
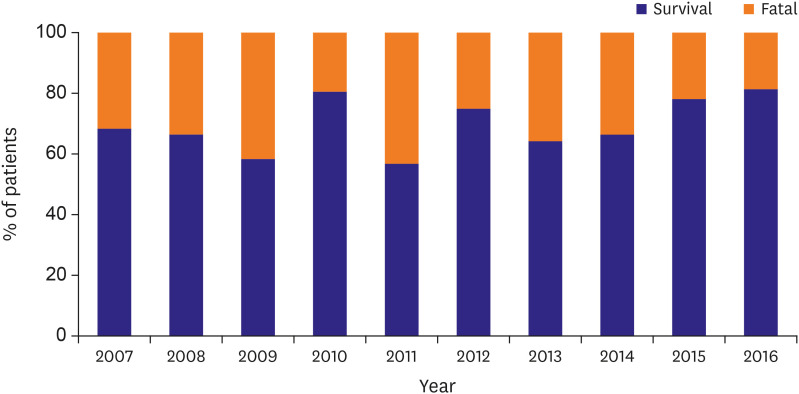
4)5) and the true incidence rate of acute myocarditis in children remains unknown. In this nationwide study, we observed that the predicted annual incidence rate of acute myocarditis in children and adolescents aged ≤19 years was approximately 2 cases/100,000 populations in Korea, which was nearly similar to the recent nationwide study performed in Finland.
1) We also observed that the incidence rate of acute myocarditis in children showed an increase over the 10-year study period. This increase in the incidence rate might be attributed (at least partially) to increased awareness of acute myocarditis among Korean physicians.
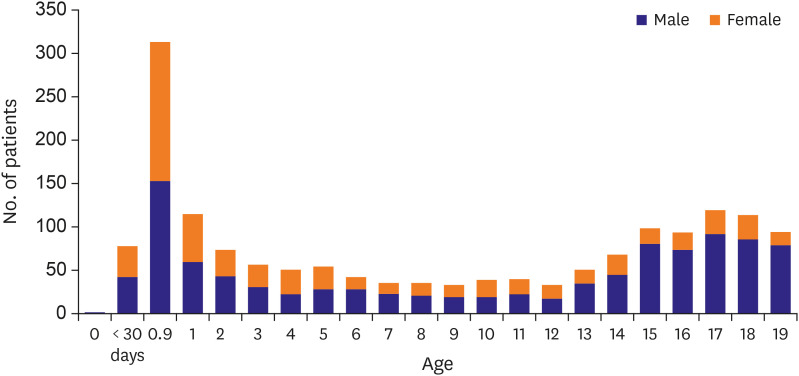
In this study, we observed a “bimodal age distribution” of acute myocarditis in children. Several previous studies have shown a bimodal age distribution with peaks during infancy and the mid-teenage years.
1)6) Interestingly, the age distribution in our study showed a remarkable peak during infancy in addition to a smaller peak during adolescence, which differed slightly from the patterns observed in the studies performed in the United States (US) or in Finland.
1)6) Notably, the age distribution observed in our study is nearly similar to that reported by Japanese studies.
2) The difference in the age distribution between Westerners and Asians has not been adequately discussed by previous studies. Therefore, no definitive conclusions can be drawn in this context. Nevertheless, it would be reasonable to consider the role of regional or racial variations.
Interestingly, the children included in this study showed a significant age-dependent sex distribution. No sex difference was observed in the incidence rate of acute myocarditis in children aged ≤5 years; however, the incidence rate in adolescents aged ≥13 years showed significant male preponderance. Although a few contradictory results have been observed with regard to the age- and sex distribution trends,
7)8) several previous studies have also reported similar male preponderance in adolescents.
1)6)9) The exact cause for the sex difference is unclear. Several experimental studies support the role of sex hormones in the occurrence of myocarditis in that estrogens have been shown to protect against myocarditis.
10) Thus, the increase in the incidence rate among adolescent males in the present study may be attributed to the increasing levels of testosterone in this patient population. However, in addition to the influence of sex hormones, complex genetic and sex chromosome–related factors and as yet unknown genetic variations might play key roles in the occurrence of myocarditis.
10)11)
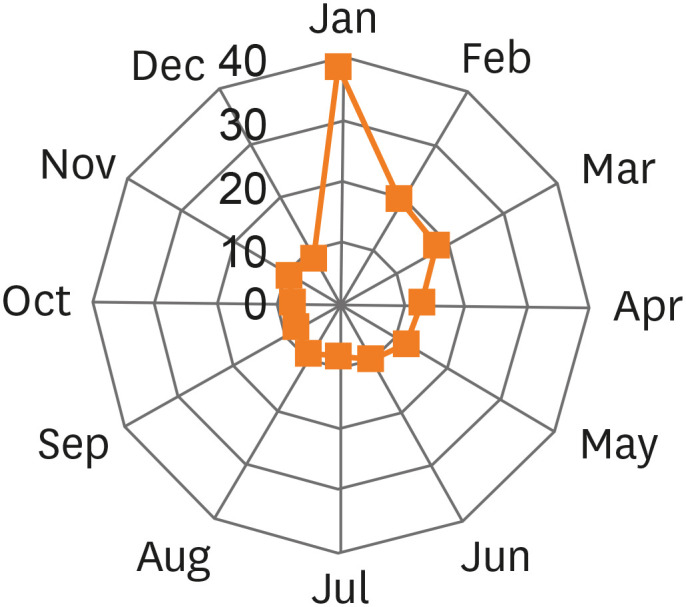
We also investigated the seasonal pattern of acute myocarditis. A previous study performed in Finland reported that the incidence of acute myocarditis was the highest between September and December.
1) We also observed a prominent seasonal variation in that nearly 50% of the cases presented between January and March in our Korean population. Acute myocarditis is primarily a viral infection; thus, this prominent seasonal variation may be explained by this etiology.
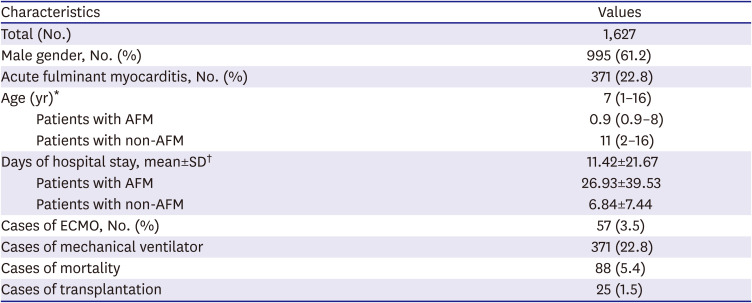
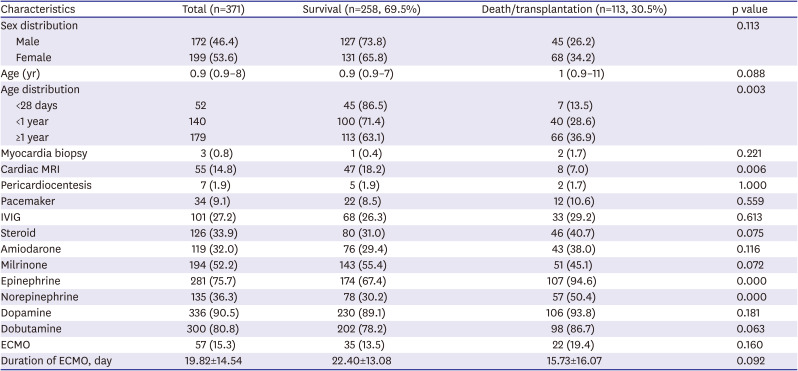
Notably, in this study, the survival rate in neonates with AFM was significantly better than that of older children; there is a possibility that transient myocardial dysfunction in neonates with ventilator support may have included and influenced the result. Clinical features of acute myocarditis vary, and AFM differs from non-AFM in terms of the aggressive and fulminant presentation of the former. Previous studies reported that the incidence of AFM may constitute approximately 10%–38% of all cases of acute myocarditis.
12)13) In our Korean population-based study, we observed that 22.8% of children with AFM received ECMO and/or mechanical ventilator support. Compared with the excellent overall survival rate of acute myocarditis (1,514 of 1,627 children, 93%), the survival rate of children with AFM was poor (69.1%), and this finding concurred with earlier reports.
2) However, the recent study in Finland reported a much higher survival rate of 84.6% in children with AFM.
1)
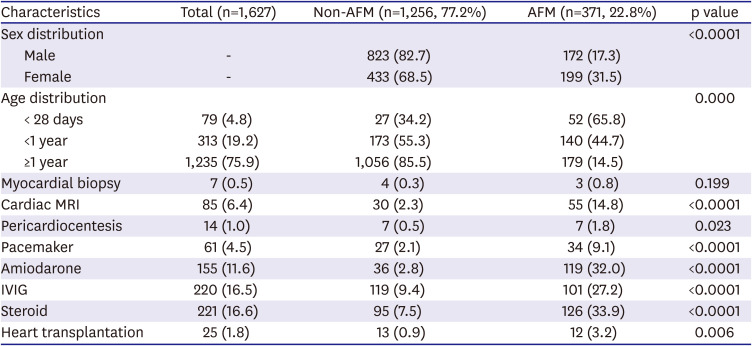
In this study, 32% of children with AFM needed amiodarone, and 9.1% of children with AFM required temporary pacemaker support. We admit that these data cannot represent the prevalence of whole kind of arrhythmias in children with myocarditis, yet it showed that clinically significant tachyarrhythmias which need medication or bradyarrhythmias which need pacemaker treatment are common complications of AFM in children. Similar with previous reports, death or heart transplantation seems not directly attributed to the arrhythmias (p=0.116 for amiodarone; p=0.559 for pacemaker).
14)15)
Those with AFM frequently tend to progress to refractory heart failure and require rescue intervention with mechanical circulatory support, like ECMO, which is the most common form of mechanical support used in children with myocarditis.
16) Despite serious risks associated with ECMO therapy, such as bleeding, brain injury, and limb ischemia, it is considered as the most important life-saving option in patients with severe, life-threatening AFM. In our study, 15.4% of children with AFM received ECMO support. A previous study reported that ECMO was initiated in approximately 17% of the children who were hospitalized with myocarditis.
17) Another study in US that used the Pediatric Health Information System database reported that ECMO was initiated in 18.9% of children hospitalized with myocarditis.
6) The rate of ECMO use in our study was slightly lower than that in previous studies. Furthermore, the utilization of ECMO did not provide significant survival benefit in our study: 57 of the 371 children with AFM (15.3%) received ECMO support, and 22 of these 57 children (38.5%) died during hospitalization. In many centers, ECMO was considered as last-resort rescue therapy after unsuccessful trials of other modalities, therefore, timely ECMO initiation seems not always take place; therefore, the lack of timely initiation of ECMO might contribute (at least partially) to this unsatisfactory result. The importance of early ECMO treatment in the survival of children with AFM was recently demonstrated by Jung et al.
18); they reported an outstanding survival rate (92.3%) in children with AFM who managed by early ECMO treatment strategy.
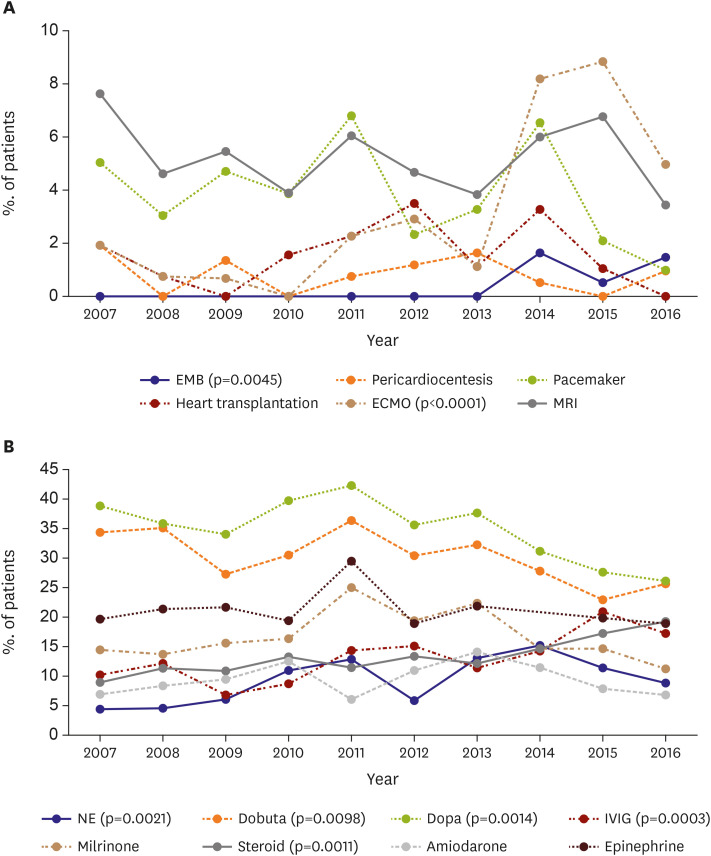
Based on the belief, that an autoreactive cellular and humoral immune response triggered by viral infection may be responsible for the myocardial inflammation, immunosuppressive therapies including corticosteroids or immunoglobulin continue to be widely used to treat acute myocarditis in children.
6)19)20)21) Similar with previous studies, immunosuppressive agents were commonly used to treat acute myocarditis in our study population (IVIG 27.2%, and corticosteroids 33.9% in children with AFM). An increasing trend was observed in immunosuppressive agents use during the study period (IVIG, p=0.0003; corticosteroids, p=0.0011). However, no significant survival benefit was observed, which was consistent with many previous studies.
22)23) Nonetheless, it is worthy of attention, that significant improvement in LVEF or LVEDD was noticed in the IVIG group in their studies. A focused trial enrolling children with severe viral myocarditis is crucial to determine the true benefit of IVIG in this group of patients.
The limitations of our study are as follows: 1) The retrospective study design is a drawback of this study. 2) Errors related to possible coding inaccuracy cannot be excluded. Besides, it is unclear what diagnostic criteria were used to label children as having myocarditis with such databases designed for cost claim issues. Further studies using either hospital-based medical records or prospective studies are required. 3) The incidence of acute myocarditis may have been under- or over-estimated in children presenting with acute myocarditis and concomitant clinical conditions such as sudden cardiac death in outpatient clinics or emergency departments. 4) Data related to etiological factors, and long-term follow-up outcomes were unavailable. Despite these limitations, the present study is clinically important because this was a large-scale study in a real-world setting that utilized data from the national database. Additionally, no selection bias was observed.
This is the first nationwide study to investigate the epidemiology and management of acute myocarditis in children in the entire Korean population. In this study, we observed an increase in the incidence of acute myocarditis in children over the last decade. To date, there is a lack of consensus regarding the management of acute myocarditis in children.
24) However, in our view, this study could serve as the backbone for future clinical trials and nationwide strategy planning for the management of acute myocarditis in children.
Go to :





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download