1. Jaeschke H, Gores GJ, Cederbaum AI, Hinson JA, Pessayre D, Lemasters JJ. Mechanisms of hepatotoxicity. Toxicol Sci. 2002; 65:166–176. PMID:
11812920.

2. Patel T, Roberts LR, Jones BA, Gores GJ. Dysregulation of apoptosis as a mechanism of liver disease: an overview. Semin Liver Dis. 1998; 18:105–114. PMID:
9606808.

3. Li S, Tan HY, Wang N, Zhang ZJ, Lao L, Wong CW, Feng Y. The role of oxidative stress and antioxidants in liver diseases. Int J Mol Sci. 2015; 16:26087–26124. PMID:
26540040.

4. Aubé C, Bazeries P, Lebigot J, Cartier V, Boursier J. Liver fibrosis, cirrhosis, and cirrhosis-related nodules: Imaging diagnosis and surveillance. Diagn Interv Imaging. 2017; 98:455–468. PMID:
28461073.

5. Hong IH, Park SJ, Goo MJ, Lee HR, Park JK, Ki MR, Kim SH, Lee EM, Kim AY, Jeong KS. JNK1 and JNK2 regulate α-SMA in hepatic stellate cells during CCl4 -induced fibrosis in the rat liver. Pathol Int. 2013; 63:483–491. PMID:
24134609.
6. Keppler D, Decker K. Studies on the mechanism of galactosamine-1-phosphate and its inhibition of UDP-glucose pyrophosphorylase. Eur J Biochem. 1969; 10:219–225. PMID:
5823097.
7. Pushpavalli G, Kalaiarasi P, Veeramani C, Pugalendi KV. Effect of chrysin on hepatoprotective and antioxidant status in D-galactosamine-induced hepatitis in rats. Eur J Pharmacol. 2010; 631:36–41. PMID:
20056116.

8. Choi KT. Botanical characteristics, pharmacological effects and medicinal components of Korean
Panax ginseng C A Meyer. Acta Pharmacol Sin. 2008; 29:1109–1118. PMID:
18718180.
9. Shin MS, Song JH, Choi P, Lee JH, Kim SY, Shin KS, Ham J, Kang KS. Stimulation of innate immune function by
Panax ginseng after heat processing. J Agric Food Chem. 2018; 66:4652–4659. PMID:
29659255.
10. Choi JG, Kim N, Huh E, Lee H, Oh MH, Park JD, Pyo MK, Oh MS. White ginseng protects mouse hippocampal cells against amyloid-beta oligomer toxicity. Phytother Res. 2017; 31:497–506. PMID:
28112442.

11. Liu Z, Li Y, Li X, Ruan CC, Wang LJ, Sun GZ. The effects of dynamic changes of malonyl ginsenosides on evaluation and quality control of
Panax ginseng C.A. Meyer. J Pharm Biomed Anal. 2012; 64-65:56–63. PMID:
22387101.
12. Du XW, Wills RB, Stuart DL. Changes in neutral and malonyl ginsenosides in American ginseng (Panax quinquefolium) during drying, storage and ethanolic extraction. Food Chem. 2004; 86:155–159.
13. Liu Z, Li W, Li X, Zhang M, Chen L, Zheng YN, Sun GZ, Ruan CC. Antidiabetic effects of malonyl ginsenosides from
Panax ginseng on type 2 diabetic rats induced by high-fat diet and streptozotocin. J Ethnopharmacol. 2013; 145:233–240. PMID:
23147499.
14. Oh MH, Park YS, Lee H, Kim NY, Jang YB, Park JH, Kwak JY, Park YS, Park JD, Pyo MK. Comparison of physicochemical properties and malonyl ginsenoside contents between white and red ginseng. Korean J Pharmacogn. 2016; 47:84–91.
15. Lu KH, Weng CY, Chen WC, Sheen LY. Ginseng essence, a medicinal and edible herbal formulation, ameliorates carbon tetrachloride-induced oxidative stress and liver injury in rats. J Ginseng Res. 2017; 41:316–325. PMID:
28701872.

16. Kim MH, Lee EJ, Cheon JM, Nam KJ, Oh TH, Kim KS. Antioxidant and hepatoprotective effects of fermented red ginseng against high fat diet-induced hyperlipidemia in rats. Lab Anim Res. 2016; 32:217–223. PMID:
28053615.

17. Wang W, Wang S, Liu J, Cai E, Zhu H, He Z, Gao Y, Li P, Zhao Y. Sesquiterpenoids from the root of
Panax ginseng protect CCl
4-induced acute liver injury by anti-inflammatory and anti-oxidative capabilities in mice. Biomed Pharmacother. 2018; 102:412–419. PMID:
29573620.
18. Niranjana Murthy H, Dandin VS, Yoeup Paek K. Hepatoprotective activity of ginsenosides from
Panax ginseng adventitious roots against carbon tetrachloride treated hepatic injury in rats. J Ethnopharmacol. 2014; 158 Pt A:442–446. PMID:
25446594.
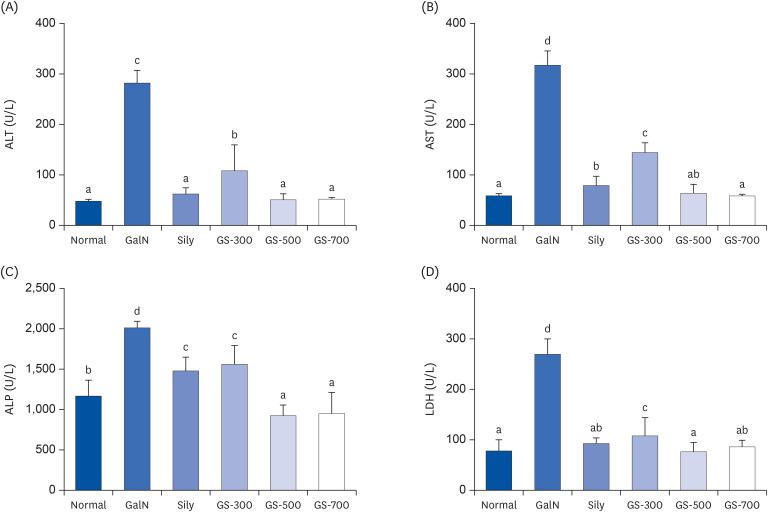
19. McGill MR. The past and present of serum aminotransferases and the future of liver injury biomarkers. EXCLI J. 2016; 15:817–828. PMID:
28337112.
20. Saraç F, Saygılı F. Causes of high bone alkaline phosphatase. Biotechnol Biotechnol Equip. 2007; 21:194–197.

21. Chaudhary A, Chauhan V. Lactate dehydrogenase as an indicator of liver diseases. J Adv Med Dent Sci Res. 2015; 3:S20–2.
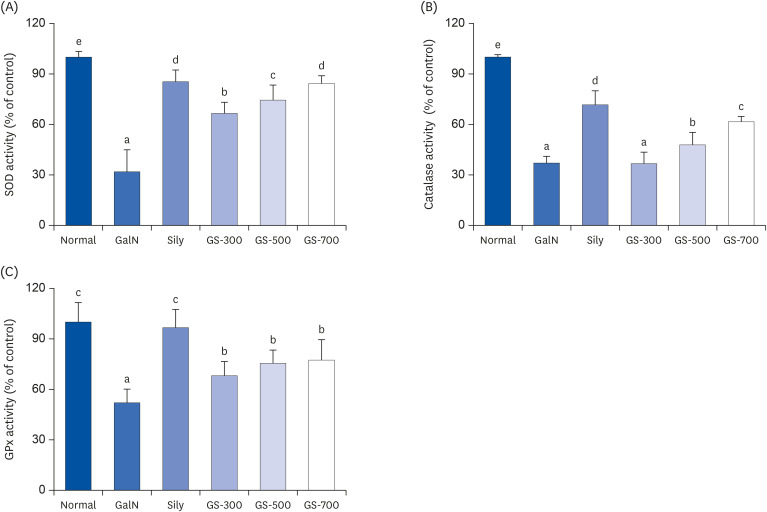
22. Ighodaro OM, Akinloye OA. First line defence antioxidants-superoxide dismutase (SOD), catalase (CAT) and glutathione peroxidase (GPX): Their fundamental role in the entire antioxidant defence grid. Alexandria J Med. 2018; 54:287–293.

23. Hu HL, Chen RD. Changes in free radicals, trace elements, and neurophysiological function in rats with liver damage induced by D-galactosamine. Biol Trace Elem Res. 1992; 34:19–25. PMID:
1382518.
24. Parthasarathi S, Hong SC, Oh MH, Park YS, Yoo JH, Seol SY, Lee H, Park JD, Pyo MK. Anti-oxidant and hepatoprotective effect of white ginsengs in H2O2-treated HepG2 cells. Nat Prod Sci. 2015; 21:210–218.
25. Kemelo MK, Horinek A, Canová NK, Farghali H. Comparative effects of Quercetin and SRT1720 against D-galactosamine/lipopolysaccharide-induced hepatotoxicity in rats: biochemical and molecular biological investigations. Eur Rev Med Pharmacol Sci. 2016; 20:363–371. PMID:
26875909.
26. Choi JW, Kim IH, Kim YM, Lee MK, Nam TJ.
Pyropia yezoensis glycoprotein regulates antioxidant status and prevents hepatotoxicity in a rat model of D-galactosamine/lipopolysaccharide-induced acute liver failure. Mol Med Rep. 2016; 13:3110–3114. PMID:
26935645.
27. Takahashi T, Morita K, Akagi R, Sassa S. Heme oxygenase-1: a novel therapeutic target in oxidative tissue injuries. Curr Med Chem. 2004; 11:1545–1561. PMID:
15180563.

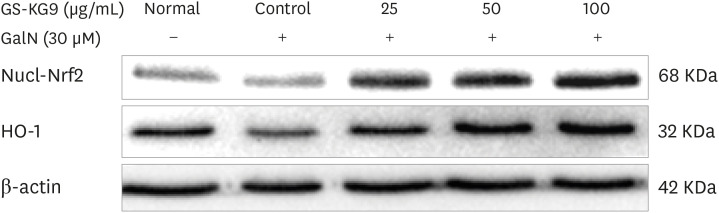
28. Tian Y, Li Z, Shen B, Wu L, Han L, Zhang Q, Feng H. The protective effects of Shikonin on lipopolysaccharide/D-galactosamine-induced acute liver injury via inhibiting MAPK and NF-κB and activating Nrf2/HO-1 signaling pathways. RSC Advances. 2017; 7:34846–34856.

29. Ma Q. Role of Nrf2 in oxidative stress and toxicity. Annu Rev Pharmacol Toxicol. 2013; 53:401–426. PMID:
23294312.

30. Guyot C, Lepreux S, Combe C, Doudnikoff E, Bioulac-Sage P, Balabaud C, Desmoulière A. Hepatic fibrosis and cirrhosis: the (myo)fibroblastic cell subpopulations involved. Int J Biochem Cell Biol. 2006; 38:135–151. PMID:
16257564.

31. Bataller R, Brenner DA. Liver fibrosis. J Clin Invest. 2005; 115:209–218. PMID:
15690074.

32. Tomanovic NR, Boricic IV, Brasanac DC, Stojsic ZM, Delic DS, Brmbolic BJ. Activated liver stellate cells in chronic viral C hepatitis: histopathological and immunohistochemical study. J Gastrointestin Liver Dis. 2009; 18:163–167. PMID:
19565045.
33. Liu RM, Desai LP. Reciprocal regulation of TGF-β and reactive oxygen species: A perverse cycle for fibrosis. Redox Biol. 2015; 6:565–577. PMID:
26496488.

34. Meng XM, Nikolic-Paterson DJ, Lan HY. TGF-β: the master regulator of fibrosis. Nat Rev Nephrol. 2016; 12:325–338. PMID:
27108839.





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download