1. Attizzani GF, Capodanno D, Ohno Y, Tamburino C. Mechanisms, pathophysiology, and clinical aspects of incomplete stent apposition. J Am Coll Cardiol. 2014; 63:1355–1367. PMID:
24530675.

2. Mintz GS, Nissen SE, Anderson WD, et al. American College of Cardiology clinical expert consensus document on standards for acquisition, measurement and reporting of intravascular ultrasound studies (IVUS). a report of the American College of Cardiology task force on clinical expert consensus documents. J Am Coll Cardiol. 2001; 37:1478–1492. PMID:
11300468.
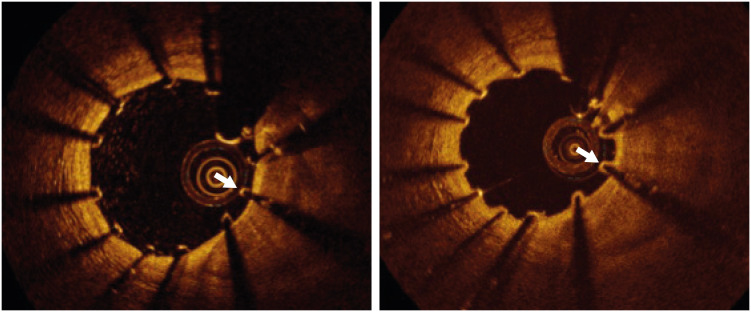
3. Tearney GJ, Regar E, Akasaka T, et al. Consensus standards for acquisition, measurement, and reporting of intravascular optical coherence tomography studies: a report from the International Working Group for Intravascular Optical Coherence Tomography Standardization and Validation. J Am Coll Cardiol. 2012; 59:1058–1072. PMID:
22421299.
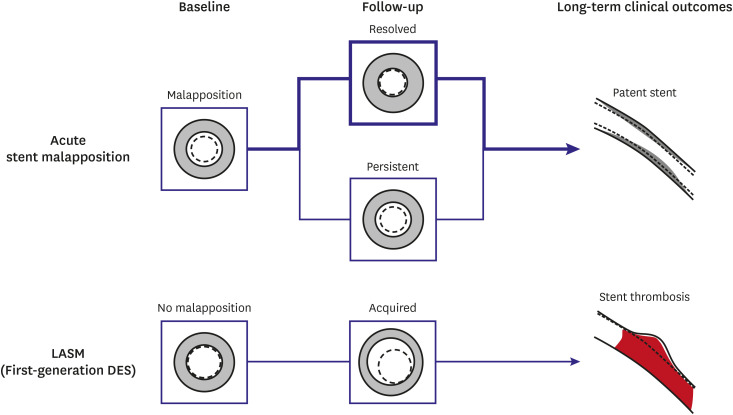
4. Lee SY, Ahn CM, Yoon HJ, et al. Early follow-up optical coherence tomographic findings of significant drug-eluting stent malapposition. Circ Cardiovasc Interv. 2018; 11:e007192. PMID:
30562088.

5. Im E, Kim BK, Ko YG, et al. Incidences, predictors, and clinical outcomes of acute and late stent malapposition detected by optical coherence tomography after drug-eluting stent implantation. Circ Cardiovasc Interv. 2014; 7:88–96. PMID:
24425586.

6. Wang B, Mintz GS, Witzenbichler B, et al. Predictors and long-term clinical impact of acute stent malapposition: an assessment of dual antiplatelet therapy with drug-eluting stents (ADAPT-DES) intravascular ultrasound substudy. J Am Heart Assoc. 2016; 5:e004438. PMID:
28007741.

7. Romagnoli E, Gatto L, La Manna A, et al. Role of residual acute stent malapposition in percutaneous coronary interventions. Catheter Cardiovasc Interv. 2017; 90:566–575. PMID:
28295990.

8. Lee SY, Im E, Hong SJ, et al. Severe acute stent malapposition after drug-eluting stent implantation: effects on long-term clinical outcomes. J Am Heart Assoc. 2019; 8:e012800. PMID:
31237187.

9. Guo N, Maehara A, Mintz GS, et al. Incidence, mechanisms, predictors, and clinical impact of acute and late stent malapposition after primary intervention in patients with acute myocardial infarction: an intravascular ultrasound substudy of the harmonizing outcomes with revascularization and stents in acute myocardial infarction (HORIZONS-AMI) trial. Circulation. 2010; 122:1077–1084. PMID:
20805433.
10. Kawamori H, Shite J, Shinke T, et al. Natural consequence of post-intervention stent malapposition, thrombus, tissue prolapse, and dissection assessed by optical coherence tomography at mid-term follow-up. Eur Heart J Cardiovasc Imaging. 2013; 14:865–875. PMID:
23291393.

11. Shimamura K, Kubo T, Akasaka T, et al. Outcomes of everolimus-eluting stent incomplete stent apposition: a serial optical coherence tomography analysis. Eur Heart J Cardiovasc Imaging. 2015; 16:23–28. PMID:
25342855.

12. Kolandaivelu K, Swaminathan R, Gibson WJ, et al. Stent thrombogenicity early in high-risk interventional settings is driven by stent design and deployment and protected by polymer-drug coatings. Circulation. 2011; 123:1400–1409. PMID:
21422389.

13. Sawaya FJ, Lefèvre T, Chevalier B, et al. Contemporary approach to coronary bifurcation lesion treatment. JACC Cardiovasc Interv. 2016; 9:1861–1878. PMID:
27659563.
14. Hong SJ, Kim H, Ahn CM, et al. Coronary artery aneurysm after second-generation drug-eluting stent implantation. Yonsei Med J. 2019; 60:824–831. PMID:
31433580.

15. Mintz GS, Shah VM, Weissman NJ. Regional remodeling as the cause of late stent malapposition. Circulation. 2003; 107:2660–2663. PMID:
12771011.

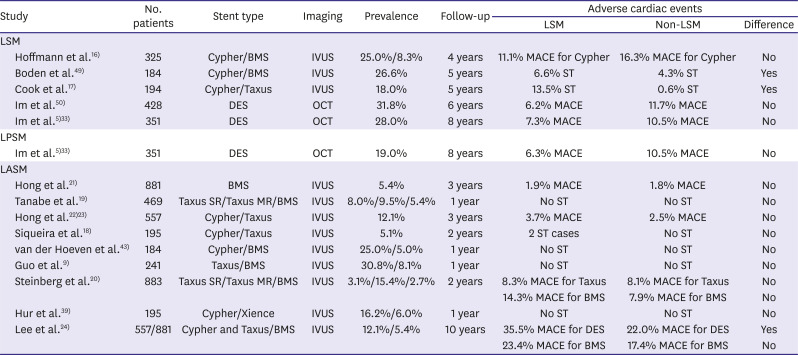
16. Hoffmann R, Morice MC, Moses JW, et al. Impact of late incomplete stent apposition after sirolimus-eluting stent implantation on 4-year clinical events: intravascular ultrasound analysis from the multicentre, randomised, RAVEL, E-SIRIUS and SIRIUS trials. Heart. 2008; 94:322–328. PMID:
17761505.

17. Cook S, Eshtehardi P, Kalesan B, et al. Impact of incomplete stent apposition on long-term clinical outcome after drug-eluting stent implantation. Eur Heart J. 2012; 33:1334–1343. PMID:
22285579.

18. Siqueira DA, Abizaid AA, Costa JR, et al. Late incomplete apposition after drug-eluting stent implantation: incidence and potential for adverse clinical outcomes. Eur Heart J. 2007; 28:1304–1309. PMID:
17478457.

19. Tanabe K, Serruys PW, Degertekin M, et al. Incomplete stent apposition after implantation of paclitaxel-eluting stents or bare metal stents: insights from the randomized TAXUS II trial. Circulation. 2005; 111:900–905. PMID:
15710761.

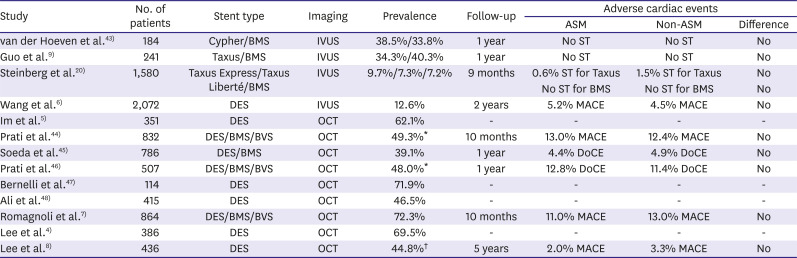
20. Steinberg DH, Mintz GS, Mandinov L, et al. Long-term impact of routinely detected early and late incomplete stent apposition: an integrated intravascular ultrasound analysis of the TAXUS IV, V, and VI and TAXUS ATLAS workhorse, long lesion, and direct stent studies. JACC Cardiovasc Interv. 2010; 3:486–494. PMID:
20488404.
21. Hong MK, Mintz GS, Lee CW, et al. Incidence, mechanism, predictors, and long-term prognosis of late stent malapposition after bare-metal stent implantation. Circulation. 2004; 109:881–886. PMID:
14967732.

22. Hong MK, Mintz GS, Lee CW, et al. Late stent malapposition after drug-eluting stent implantation: an intravascular ultrasound analysis with long-term follow-up. Circulation. 2006; 113:414–419. PMID:
16432073.
23. Hong MK, Mintz GS, Lee CW, et al. Impact of late drug-eluting stent malapposition on 3-year clinical events. J Am Coll Cardiol. 2007; 50:1515–1516. PMID:
17919574.

24. Lee SY, Ahn JM, Mintz GS, et al. Ten-year clinical outcomes of late-acquired stent malapposition after coronary stent implantation. Arterioscler Thromb Vasc Biol. 2020; 40:288–295. PMID:
31766872.

25. Virmani R, Guagliumi G, Farb A, et al. Localized hypersensitivity and late coronary thrombosis secondary to a sirolimus-eluting stent: should we be cautious? Circulation. 2004; 109:701–705. PMID:
14744976.
26. Cook S, Ladich E, Nakazawa G, et al. Correlation of intravascular ultrasound findings with histopathological analysis of thrombus aspirates in patients with very late drug-eluting stent thrombosis. Circulation. 2009; 120:391–399. PMID:
19620501.

27. Karalis I, Ahmed TA, Jukema JW. Late acquired stent malapposition: why, when and how to handle? Heart. 2012; 98:1529–1536. PMID:
23001063.

28. Lüscher TF, Steffel J, Eberli FR, et al. Drug-eluting stent and coronary thrombosis: biological mechanisms and clinical implications. Circulation. 2007; 115:1051–1058. PMID:
17325255.
29. Wilson GJ, Nakazawa G, Schwartz RS, et al. Comparison of inflammatory response after implantation of sirolimus- and paclitaxel-eluting stents in porcine coronary arteries. Circulation. 2009; 120:141–149. PMID:
19564562.

30. Nakazawa G, Finn AV, Vorpahl M, Ladich ER, Kolodgie FD, Virmani R. Coronary responses and differential mechanisms of late stent thrombosis attributed to first-generation sirolimus- and paclitaxel-eluting stents. J Am Coll Cardiol. 2011; 57:390–398. PMID:
21251578.

31. Otsuka F, Vorpahl M, Nakano M, et al. Pathology of second-generation everolimus-eluting stents versus first-generation sirolimus- and paclitaxel-eluting stents in humans. Circulation. 2014; 129:211–223. PMID:
24163064.

32. Rizas KD, Mehilli J. Stent polymers: do they make a difference? Circ Cardiovasc Interv. 2016; 9:e002943. PMID:
27193905.
33. Im E, Hong SJ, Ahn CM, et al. Long-term clinical outcomes of late stent malapposition detected by optical coherence tomography after drug-eluting stent implantation. J Am Heart Assoc. 2019; 8:e011817. PMID:
30905253.

34. Räber L, Mintz GS, Koskinas KC, et al. Clinical use of intracoronary imaging. Part 1: guidance and optimization of coronary interventions. An expert consensus document of the European Association of Percutaneous Cardiovascular Interventions. Eur Heart J. 2018; 39:3281–3300. PMID:
29790954.

35. Souteyrand G, Amabile N, Mangin L, et al. Mechanisms of stent thrombosis analysed by optical coherence tomography: insights from the national PESTO French registry. Eur Heart J. 2016; 37:1208–1216. PMID:
26757787.

36. Taniwaki M, Radu MD, Zaugg S, et al. Mechanisms of very late drug-eluting stent thrombosis assessed by optical coherence tomography. Circulation. 2016; 133:650–660. PMID:
26762519.

37. Adriaenssens T, Joner M, Godschalk TC, et al. Optical coherence tomography findings in patients with coronary stent thrombosis: a report of the PRESTIGE consortium (prevention of late stent thrombosis by an interdisciplinary global European effort). Circulation. 2017; 136:1007–1021. PMID:
28720725.
38. Banning AP, Lassen JF, Burzotta F, et al. Percutaneous coronary intervention for obstructive bifurcation lesions: the 14th consensus document from the European Bifurcation Club. EuroIntervention. 2019; 15:90–98. PMID:
31105066.

39. Hur SH, Lee BR, Kim SW, et al. Late-acquired incomplete stent apposition after everolimus-eluting stent versus sirolimus-eluting stent implantation in patients with non-ST-segment elevation myocardial infarction and ST-segment elevation myocardial infarction. EuroIntervention. 2016; 12:e979–86. PMID:
26403637.

40. Palmerini T, Kirtane AJ, Serruys PW, et al. Stent thrombosis with everolimus-eluting stents: meta-analysis of comparative randomized controlled trials. Circ Cardiovasc Interv. 2012; 5:357–364. PMID:
22668554.

41. Doi T, Kataoka Y, Noguchi T, et al. Coronary artery ectasia predicts future cardiac events in patients with acute myocardial infarction. Arterioscler Thromb Vasc Biol. 2017; 37:2350–2355. PMID:
29051141.
42. Kawsara A, Núñez Gil IJ, Alqahtani F, Moreland J, Rihal CS, Alkhouli M. Management of coronary artery aneurysms. JACC Cardiovasc Interv. 2018; 11:1211–1223. PMID:
29976357.
43. van der Hoeven BL, Liem SS, Dijkstra J, et al. Stent malapposition after sirolimus-eluting and bare-metal stent implantation in patients with ST-segment elevation myocardial infarction: acute and 9-month intravascular ultrasound results of the MISSION! intervention study. JACC Cardiovasc Interv. 2008; 1:192–201. PMID:
19463300.
44. Prati F, Romagnoli E, Burzotta F, et al. Clinical impact of OCT findings during PCI: the CLI-OPCI II study. JACC Cardiovasc Imaging. 2015; 8:1297–1305. PMID:
26563859.
45. Soeda T, Uemura S, Park SJ, et al. Incidence and clinical significance of poststent optical coherence tomography findings: one-year follow-up study from a multicenter registry. Circulation. 2015; 132:1020–1029. PMID:
26162917.
46. Prati F, Romagnoli E, Gatto L, et al. Clinical impact of suboptimal stenting and residual intrastent plaque/thrombus protrusion in patients with acute coronary syndrome: the CLI-OPCI ACS substudy (Centro per la Lotta Contro L'Infarto-Optimization of Percutaneous Coronary Intervention in Acute Coronary Syndrome). Circ Cardiovasc Interv. 2016; 9:e003726. PMID:
27965297.

47. Bernelli C, Shimamura K, Komukai K, et al. Impact of culprit plaque and atherothrombotic components on incomplete stent apposition in patients with ST-elevation myocardial infarction treated with everolimus-eluting stents - an OCTAVIA substudy. Circ J. 2016; 80:895–905. PMID:
26853719.
48. Ali ZA, Maehara A, Généreux P, et al. Optical coherence tomography compared with intravascular ultrasound and with angiography to guide coronary stent implantation (ILUMIEN III: OPTIMIZE PCI): a randomised controlled trial. Lancet. 2016; 388:2618–2628. PMID:
27806900.

49. Boden H, van der Hoeven BL, Liem SS, et al. Five-year clinical follow-up from the MISSION! intervention study: sirolimus-eluting stent versus bare metal stent implantation in patients with ST-segment elevation myocardial infarction, a randomised controlled trial. EuroIntervention. 2012; 7:1021–1029. PMID:
22207227.

50. Im E, Lee SY, Hong SJ, et al. Impact of late stent malapposition after drug-eluting stent implantation on long-term clinical outcomes. Atherosclerosis. 2019; 288:118–123. PMID:
31357039.





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download