1. Torp-Pedersen C, Goette A, Nielsen PB, et al. ‘Real-world’ observational studies in arrhythmia research: data sources, methodology, and interpretation. A position document from European Heart Rhythm Association (EHRA), endorsed by Heart Rhythm Society (HRS), Asia-Pacific HRS (APHRS), and Latin America HRS (LAHRS). Europace. 2020; 22:831–832. PMID:
31725156.

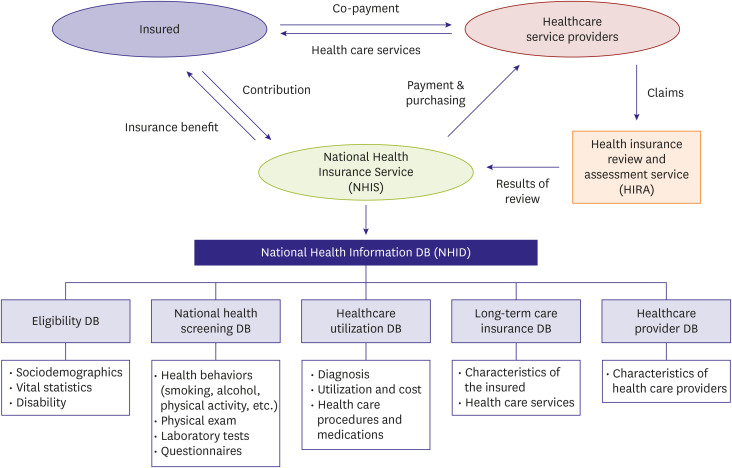
2. Song SO, Jung CH, Song YD, et al. Background and data configuration process of a nationwide population-based study using the korean national health insurance system. Diabetes Metab J. 2014; 38:395–403. PMID:
25349827.

3. Cheol Seong S, Kim YY, Khang YH, et al. Data resource profile: the National Health Information Database of the National Health Insurance Service in South Korea. Int J Epidemiol. 2017; 46:799–800. PMID:
27794523.

4. Won TY, Kang BS, Im TH, Choi HJ. The study of accuracy of death statistics. J Korean Soc Emerg Med. 2007; 18:256–262.
5. Seong SC, Kim YY, Park SK, et al. Cohort profile: the National Health Insurance Service-National Health Screening Cohort (NHIS-HEALS) in Korea. BMJ Open. 2017; 7:e016640.

6. National Health Insurance Service. National health screening statistical yearbook. Seoul: National Health Insurance Service;2014.
7. Lee J, Lee JS, Park SH, Shin SA, Kim K. Cohort profile: the National Health Insurance Service-National Sample Cohort (NHIS-NSC), South Korea. Int J Epidemiol. 2017; 46:e15. PMID:
26822938.

8. Kim JA, Yoon S, Kim LY, Kim DS. Towards actualizing the value potential of Korea Health Insurance Review and Assessment (HIRA) data as a resource for health research: strengths, limitations, applications, and strategies for optimal use of HIRA data. J Korean Med Sci. 2017; 32:718–728. PMID:
28378543.

9. Chao TF, Liu CJ, Tuan TC, et al. Lifetime risks, projected numbers, and adverse outcomes in asian patients with atrial fibrillation: a report from the Taiwan nationwide AF cohort study. Chest. 2018; 153:453–466. PMID:
29017957.
10. Chan YH, Kuo CT, Yeh YH, et al. Thromboembolic, bleeding, and mortality risks of rivaroxaban and dabigatran in asians with nonvalvular atrial fibrillation. J Am Coll Cardiol. 2016; 68:1389–1401. PMID:
27659460.
11. Chao TF, Liu CJ, Lin YJ, et al. Oral anticoagulation in very elderly patients with atrial fibrillation: a nationwide cohort study. Circulation. 2018; 138:37–47. PMID:
29490992.
12. Shih CJ, Ou SM, Chao PW, et al. Risks of death and stroke in patients undergoing hemodialysis with new-onset atrial fibrillation: a competing-risk analysis of a nationwide cohort. Circulation. 2016; 133:265–272. PMID:
26680239.
13. Chao TF, Lip GY, Lin YJ, et al. Age threshold for the use of non-vitamin K antagonist oral anticoagulants for stroke prevention in patients with atrial fibrillation: insights into the optimal assessment of age and incident comorbidities. Eur Heart J. 2019; 40:1504–1514. PMID:
30605505.

14. Chao TF, Liu CJ, Wang KL, et al. Should atrial fibrillation patients with 1 additional risk factor of the CHA2DS2-VASc score (beyond sex) receive oral anticoagulation? J Am Coll Cardiol. 2015; 65:635–642. PMID:
25677422.
15. Chao TF, Wang KL, Liu CJ, et al. Age threshold for increased stroke risk among patients with atrial fibrillation: a nationwide cohort study from Taiwan. J Am Coll Cardiol. 2015; 66:1339–1347. PMID:
26383720.
16. Chao TF, Lip GY, Liu CJ, et al. Relationship of aging and incident comorbidities to stroke risk in patients with atrial fibrillation. J Am Coll Cardiol. 2018; 71:122–132. PMID:
29325634.
17. Go AS, Hylek EM, Phillips KA, et al. Prevalence of diagnosed atrial fibrillation in adults: national implications for rhythm management and stroke prevention: the AnTicoagulation and Risk Factors in Atrial Fibrillation (ATRIA) study. JAMA. 2001; 285:2370–2375. PMID:
11343485.
18. Schnabel RB, Yin X, Gona P, et al. 50 year trends in atrial fibrillation prevalence, incidence, risk factors, and mortality in the Framingham Heart Study: a cohort study. Lancet. 2015; 386:154–162. PMID:
25960110.

19. Lee SR, Choi EK, Han KD, Cha MJ, Oh S. Trends in the incidence and prevalence of atrial fibrillation and estimated thromboembolic risk using the CHA
2DS
2-VASc score in the entire Korean population. Int J Cardiol. 2017; 236:226–231. PMID:
28233629.
20. Kim D, Yang PS, Jang E, et al. Increasing trends in hospital care burden of atrial fibrillation in Korea, 2006 through 2015. Heart. 2018; 104:2010–2017. PMID:
29666179.

21. Benjamin EJ, Wolf PA, D'Agostino RB, Silbershatz H, Kannel WB, Levy D. Impact of atrial fibrillation on the risk of death: the Framingham Heart Study. Circulation. 1998; 98:946–952. PMID:
9737513.
22. Lee E, Choi EK, Han KD, et al. Mortality and causes of death in patients with atrial fibrillation: a nationwide population-based study. PLoS One. 2018; 13:e0209687. PMID:
30586468.

23. Lee SR, Choi EK, Han KD, Cha MJ, Oh S, Lip GY. Temporal trends of antithrombotic therapy for stroke prevention in Korean patients with non-valvular atrial fibrillation in the era of non-vitamin K antagonist oral anticoagulants: a nationwide population-based study. PLoS One. 2017; 12:e0189495. PMID:
29261716.

24. Huisman MV, Rothman KJ, Paquette M, et al. GLORIA-AF Investigators. The changing landscape for stroke prevention in AF: findings from the GLORIA-AF registry phase 2. J Am Coll Cardiol. 2017; 69:777–785. PMID:
28209218.
25. Lee SR, Choi EK, Han K, Cha MJ, Oh S. Prevalence of non-valvular atrial fibrillation based on geographical distribution and socioeconomic status in the entire Korean population. Korean Circ J. 2018; 48:622–634. PMID:
29968435.

26. Yu HT, Yang PS, Hwang J, et al. Social inequalities of oral anticoagulation after the introduction of non-vitamin K antagonists in patients with atrial fibrillation. Korean Circ J. 2020; 50:267–277. PMID:
32100483.

27. Lee SR, Choi EK, Kwon S, et al. Effectiveness and safety of direct oral anticoagulants in relation to temporal changes in their use. Circ Cardiovasc Qual Outcomes. 2020; 13:e005894. PMID:
32160790.

28. Cannon CP, Bhatt DL, Oldgren J, et al. Dual antithrombotic therapy with dabigatran after PCI in atrial fibrillation. N Engl J Med. 2017; 377:1513–1524. PMID:
28844193.

29. Lopes RD, Heizer G, Aronson R, et al. Antithrombotic therapy after acute coronary syndrome or PCI in atrial fibrillation. N Engl J Med. 2019; 380:1509–1524. PMID:
30883055.

30. Vranckx P, Valgimigli M, Eckardt L, et al. Edoxaban-based versus vitamin K antagonist-based antithrombotic regimen after successful coronary stenting in patients with atrial fibrillation (ENTRUST-AF PCI): a randomised, open-label, phase 3b trial. Lancet. 2019; 394:1335–1343. PMID:
31492505.

31. Gibson CM, Mehran R, Bode C, et al. Prevention of bleeding in patients with atrial fibrillation undergoing PCI. N Engl J Med. 2016; 375:2423–2434. PMID:
27959713.

32. Park J, Choi EK, Han KD, et al. Temporal trends in prevalence and antithrombotic treatment among Asians with atrial fibrillation undergoing percutaneous coronary intervention: a nationwide Korean population-based study. PLoS One. 2019; 14:e0209593. PMID:
30645601.

33. Park J, Choi EK, Han KD, et al. Antithrombotic therapy in patients with atrial fibrillation after percutaneous coronary intervention during 2-year follow-up, from a nationwide population study. Am J Cardiol. 2019; 123:1921–1926. PMID:
30967291.

34. Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005; 43:1130–1139. PMID:
16224307.

35. Lip GY, Nieuwlaat R, Pisters R, Lane DA, Crijns HJ. Refining clinical risk stratification for predicting stroke and thromboembolism in atrial fibrillation using a novel risk factor-based approach: the euro heart survey on atrial fibrillation. Chest. 2010; 137:263–272. PMID:
19762550.
36. Kang SH, Choi EK, Han KD, et al. Risk of ischemic stroke in patients with non-valvular atrial fibrillation not receiving oral anticoagulants - Korean nationwide population-based study. Circ J. 2017; 81:1158–1164. PMID:
28413184.
37. Kim TH, Yang PS, Uhm JS, et al. CHA
2DS
2-VASc score (congestive heart failure, hypertension, age ≥75 [doubled], diabetes mellitus, prior stroke or transient ischemic attack [doubled], vascular disease, age 65–74, female) for stroke in Asian patients with atrial fibrillation: a Korean nationwide sample cohort study. Stroke. 2017; 48:1524–1530. PMID:
28455320.
38. Joung B, Lee JM, Lee KH, et al. 2018 Korean guideline of atrial fibrillation management. Korean Circ J. 2018; 48:1033–1080. PMID:
30403013.

39. Lip GY, Wang KL, Chiang CE. Non-vitamin K antagonist oral anticoagulants (NOACs) for stroke prevention in Asian patients with atrial fibrillation: time for a reappraisal. Int J Cardiol. 2015; 180:246–254. PMID:
25463377.

40. Li YG, Lee SR, Choi EK, Lip GY. stroke prevention in atrial fibrillation: focus on Asian patients. Korean Circ J. 2018; 48:665–684. PMID:
30073805.

41. Lin YC, Chien SC, Hsieh YC, et al. Effectiveness and safety of standard- and low-dose rivaroxaban in Asians with atrial fibrillation. J Am Coll Cardiol. 2018; 72:477–485. PMID:
30049307.
42. Cha MJ, Choi EK, Han KD, et al. Effectiveness and safety of non-vitamin K antagonist oral anticoagulants in Asian patients with atrial fibrillation. Stroke. 2017; 48:3040–3048. PMID:
28974629.

43. Lee SR, Choi EK, Han KD, Jung JH, Oh S, Lip GY. Edoxaban in Asian patients with atrial fibrillation: effectiveness and Safety. J Am Coll Cardiol. 2018; 72:838–853. PMID:
30115222.
44. Lee SR, Choi EK, Han KD, Jung JH, Oh S, Lip GY. Optimal rivaroxaban dose in Asian patients with atrial fibrillation and normal or mildly impaired renal function. Stroke. 2019; 50:1140–1148. PMID:
30913984.

45. Lee SR, Choi EK, Han KD, et al. Non-vitamin K antagonist oral anticoagulants in Asian patients with supranormal renal function. Stroke. 2019; 50:1480–1489. PMID:
31084339.

46. Lee SR, Choi EK, Kwon S, et al. Effectiveness and safety of contemporary oral anticoagulants among Asians with nonvalvular atrial fibrillation. Stroke. 2019; 50:2245–2249. PMID:
31208303.

47. Lee SR, Choi EK, Park CS, et al. Direct oral anticoagulants in patients with nonvalvular atrial fibrillation and low body weight. J Am Coll Cardiol. 2019; 73:919–931. PMID:
30819360.
48. Lee SR, Lee HJ, Choi EK, et al. Direct oral anticoagulants in patients with atrial fibrillation and liver disease. J Am Coll Cardiol. 2019; 73:3295–3308. PMID:
31248551.
49. Connolly SJ, Ezekowitz MD, Yusuf S, et al. Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med. 2009; 361:1139–1151. PMID:
19717844.

50. Granger CB, Alexander JH, McMurray JJ, et al. Apixaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2011; 365:981–992. PMID:
21870978.
51. Patel MR, Mahaffey KW, Garg J, et al. Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. N Engl J Med. 2011; 365:883–891. PMID:
21830957.

52. Giugliano RP, Ruff CT, Braunwald E, et al. Edoxaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2013; 369:2093–2104. PMID:
24251359.

53. Yu HT, Yang PS, Kim TH, et al. Impact of renal function on outcomes with edoxaban in real-world patients with atrial fibrillation. Stroke. 2018; 49:2421–2429. PMID:
30355093.

55. Lee SR, Choi EK, Kwon S, et al. Oral anticoagulation in Asian patients with atrial fibrillation and a history of intracranial hemorrhage. Stroke. 2020; 51:416–423. PMID:
31813363.

56. Park J, Lee SR, Choi EK, et al. Effectiveness and safety of direct oral anticoagulant for secondary prevention in Asians with atrial fibrillation. J Clin Med. 2019; 8:8.

57. Kim YG, Han KD, Choi JI, et al. Frequent drinking is a more important risk factor for new-onset atrial fibrillation than binge drinking: a nationwide population-based study. Europace. 2020; 22:216–224. PMID:
31620800.

58. Rhee TM, Lee JH, Choi EK, et al. Increased risk of atrial fibrillation and thromboembolism in patients with severe psoriasis: a nationwide population-based study. Sci Rep. 2017; 7:9973. PMID:
28855659.

59. Lee SR, Choi EK, Han KD, Cha MJ, Oh S. Association between γ-glutamyltransferase level and incidence of atrial fibrillation: a nationwide population-based study. Int J Cardiol. 2017; 245:149–155. PMID:
28757090.

60. Kim MK, Han K, Park YM, et al. Associations of variability in blood pressure, glucose and cholesterol concentrations, and body mass index with mortality and cardiovascular outcomes in the general population. Circulation. 2018; 138:2627–2637. PMID:
30571256.

61. Kim MK, Han K, Kim HS, et al. Cholesterol variability and the risk of mortality, myocardial infarction, and stroke: a nationwide population-based study. Eur Heart J. 2017; 38:3560–3566. PMID:
29069458.

62. Lee HJ, Lee SR, Choi EK, Han KD, Oh S. Low lipid levels and high variability are associated with the risk of new-onset atrial fibrillation. J Am Heart Assoc. 2019; 8:e012771. PMID:
31771440.

63. Kwon S, Lee SR, Choi EK, et al. Fluctuating renal function and the risk of incident atrial fibrillation: a nationwide population-based study. Sci Rep. 2019; 9:18055. PMID:
31792292.

64. Lee SR, Choi YJ, Choi EK, et al. Blood pressure variability and incidence of new-onset atrial fibrillation: a nationwide population-based study. Hypertension. 2020; 75:309–315. PMID:
31838903.
65. Lee SR, Choi EK, Han KD, Lee SH, Oh S. Effect of the variability of blood pressure, glucose level, total cholesterol level, and body mass index on the risk of atrial fibrillation in a healthy population. Heart Rhythm. 2020; 17:12–19. PMID:
31299298.

66. Kwon S, Lee SR, Choi EK, et al. Visit-to-visit variability of metabolic parameters and risk of heart failure: a nationwide population-based study. Int J Cardiol. 2019; 293:153–158. PMID:
31253527.

67. Lee H, Park JB, Hwang IC, et al. Association of four lipid components with mortality, myocardial infarction, and stroke in statin-naïve young adults: a nationwide cohort study. Eur J Prev Cardiol. 2020.

68. Park JB, Kim DH, Lee H, et al. Mildly abnormal lipid levels, but not high lipid variability, are associated with increased risk of myocardial infarction and stroke in “statin-naive” young population a nationwide cohort study. Circ Res. 2020; 126:824–835. PMID:
31978313.

69. Choi YJ, Choi EK, Han KD, et al. Temporal trends of the prevalence and incidence of atrial fibrillation and stroke among Asian patients with hypertrophic cardiomyopathy: a nationwide population-based study. Int J Cardiol. 2018; 273:130–135. PMID:
30150122.

70. Moon I, Lee SY, Kim HK, et al. Trends of the prevalence and incidence of hypertrophic cardiomyopathy in Korea: a nationwide population-based cohort study. PLoS One. 2020; 15:e0227012. PMID:
31929538.

71. Choi YJ, Choi EK, Han KD, et al. Increased risk of atrial fibrillation in patients with inflammatory bowel disease: a nationwide population-based study. World J Gastroenterol. 2019; 25:2788–2798. PMID:
31236001.

72. Moon I, Choi EK, Jung JH, et al. Ankylosing spondylitis: a novel risk factor for atrial fibrillation - a nationwide population-based study. Int J Cardiol. 2019; 275:77–82. PMID:
30360993.

73. Lee E, Choi EK, Jung JH, et al. Increased risk of atrial fibrillation in patients with Behçet's disease: a nationwide population-based study. Int J Cardiol. 2019; 292:106–111. PMID:
31256991.

74. Choi YJ, Kim SH, Kang SH, et al. Reconsidering the cut-off diastolic blood pressure for predicting cardiovascular events: a nationwide population-based study from Korea. Eur Heart J. 2019; 40:724–731. PMID:
30535368.

75. Lee CJ, Ryu J, Kim HC, et al. Clinical benefit of treatment of stage-1, low-risk hypertension. Hypertension. 2018; 72:1285–1293. PMID:
30571236.

76. Kim MK, Han K, Koh ES, et al. Blood pressure and development of cardiovascular disease in Koreans with type 2 diabetes mellitus. Hypertension. 2019; 73:319–326. PMID:
30624985.

77. Lee YH, Han K, Ko SH, et al. Data analytic process of a nationwide population-based study using National Health Information Database established by National Health Insurance Service. Diabetes Metab J. 2016; 40:79–82. PMID:
26912157.

78. Kim TH, Yang PS, Kim D, et al. CHA
2DS
2-VASc score for identifying truly low-risk atrial fibrillation for stroke: a Korean nationwide cohort study. Stroke. 2017; 48:2984–2990. PMID:
28939672.
79. Ha KH, Kim B, Shin HS, et al. Comparative cardiovascular risks of dipeptidyl peptidase-4 inhibitors: analyses of real-world data in Korea. Korean Circ J. 2018; 48:395–405. PMID:
29671284.

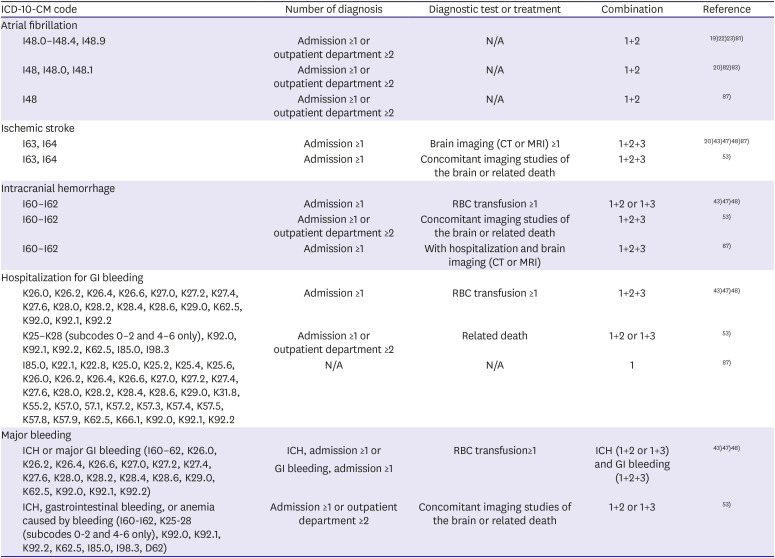
80. Park J, Kwon S, Choi EK, et al. Validation of diagnostic codes of major clinical outcomes in a National Health Insurance database. Int J Arrhythmia. 2019; 20:5.

81. Kang SH, Choi EK, Han KD, et al. Underweight is a risk factor for atrial fibrillation: A nationwide population-based study. Int J Cardiol. 2016; 215:449–456. PMID:
27131763.

82. Yang PS, Ryu S, Kim D, et al. Variations of prevalence and incidence of atrial fibrillation and oral anticoagulation rate according to different analysis approaches. Sci Rep. 2018; 8:6856. PMID:
29717165.

83. Lee SS, Ae Kong K, Kim D, et al. Clinical implication of an impaired fasting glucose and prehypertension related to new onset atrial fibrillation in a healthy Asian population without underlying disease: a nationwide cohort study in Korea. Eur Heart J. 2017; 38:2599–2607. PMID:
28662568.

84. Chao TF, Liu CJ, Tuan TC, et al. Rate-control treatment and mortality in atrial fibrillation. Circulation. 2015; 132:1604–1612. PMID:
26384160.

85. Chang CH, Lee YC, Tsai CT, et al. Continuation of statin therapy and a decreased risk of atrial fibrillation/flutter in patients with and without chronic kidney disease. Atherosclerosis. 2014; 232:224–230. PMID:
24401243.

86. Lee SR, Choi EK, Han KD, Jung JH, Oh S, Lip GY. Comparison of once-daily administration of edoxaban and rivaroxaban in Asian patients with atrial fibrillation. Sci Rep. 2019; 9:6690. PMID:
31040359.

87. Cho MS, Yun JE, Park JJ, et al. Outcomes after use of standard- and low-dose non-vitamin K oral anticoagulants in asian patients with atrial fibrillation. Stroke. 2018.





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download