Analysis of diagnosis and surgical mortality by patient age
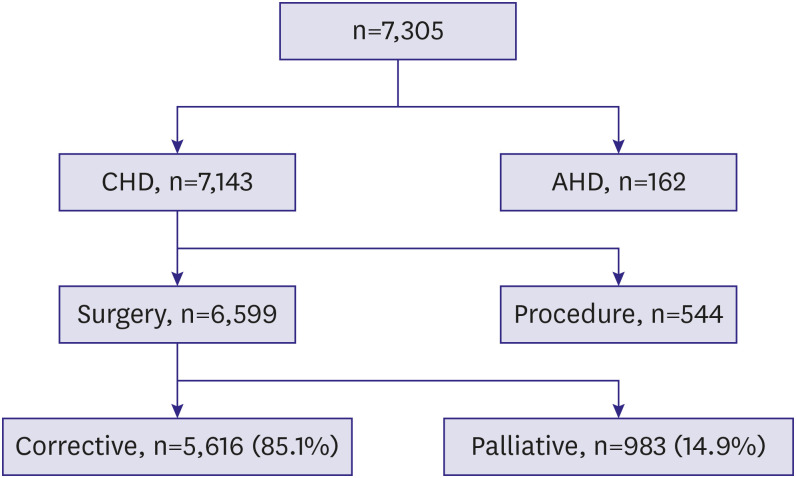
The early mortality rate was 3.8%, while the late mortality rate was 1.8%. Previous reports of the KHF (not published in English) (1984–1999) showed that the early surgical mortality rate was 8.6%, and the late mortality rate was 5.3%. The surgical outcomes of the current era were improved in contrast to those of the earlier time period (
Supplementary Figure 2).
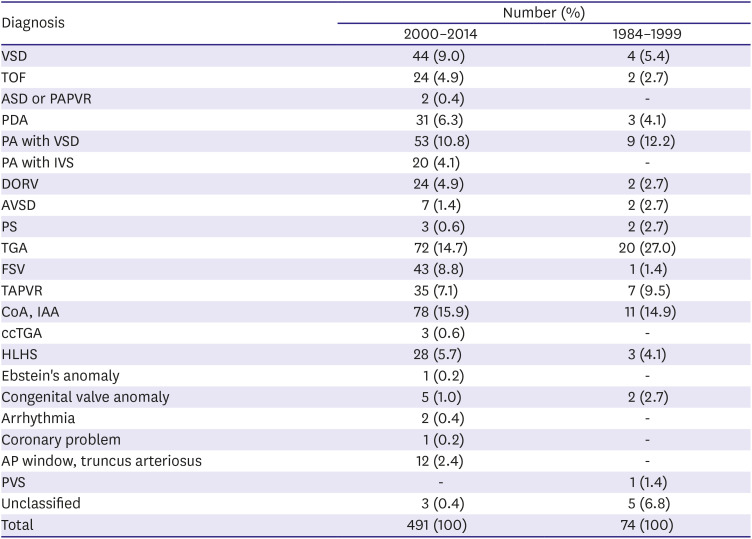
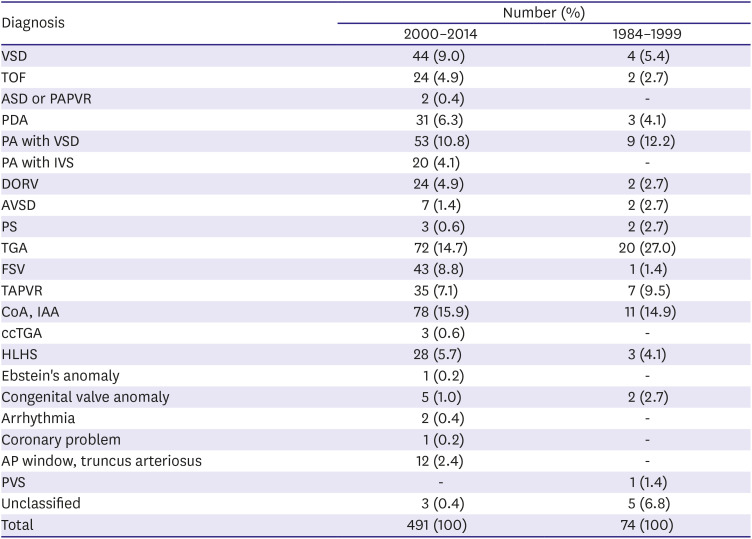
Neonates
There were 491 neonates (7.4%); of the, 288 (58.7%) were male. The disease prevalence is shown in
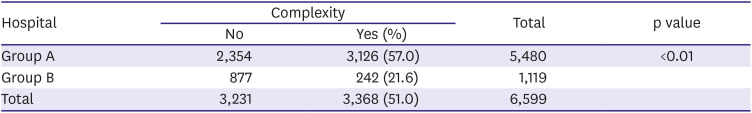
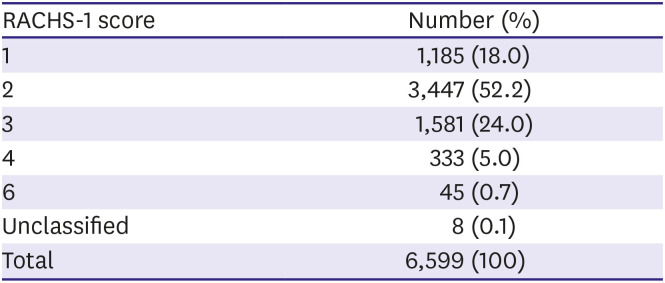
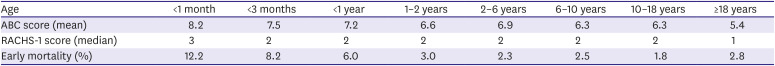
Table 3. Compared to the other surgical eras (1984–1999), there was a great increase in neonate patients (491 vs. 74), and new diseases were added, including atrial septal defect (ASD), partial anomalous pulmonary venous return (PAPVR), PA with IVS, ccTGA, arrhythmia, coronary problem. The median hospital stay was 19 days (range, 0–277 days). A total of 491 procedures were performed (457 [93.1%] in group A, 34 [6.9%] in group B): 343 (69.9%) biventricular repairs and 148 (30.1%) palliative procedures. The mean ABC score was 8.2±2.7. A RACHS-1 score of 3 was the most common. Complex procedures were performed in 365 patients (74.3%). The early mortality rate was 12.2%, while the late mortality rate was 3.7%. The early surgical mortality rate of other surgical eras (1984–1999) was 29.7%.
Table 3
Neonates' diagnosis prevalence
|
Diagnosis |
Number (%) |
|
2000–2014 |
1984–1999 |
|
VSD |
44 (9.0) |
4 (5.4) |
|
TOF |
24 (4.9) |
2 (2.7) |
|
ASD or PAPVR |
2 (0.4) |
- |
|
PDA |
31 (6.3) |
3 (4.1) |
|
PA with VSD |
53 (10.8) |
9 (12.2) |
|
PA with IVS |
20 (4.1) |
- |
|
DORV |
24 (4.9) |
2 (2.7) |
|
AVSD |
7 (1.4) |
2 (2.7) |
|
PS |
3 (0.6) |
2 (2.7) |
|
TGA |
72 (14.7) |
20 (27.0) |
|
FSV |
43 (8.8) |
1 (1.4) |
|
TAPVR |
35 (7.1) |
7 (9.5) |
|
CoA, IAA |
78 (15.9) |
11 (14.9) |
|
ccTGA |
3 (0.6) |
- |
|
HLHS |
28 (5.7) |
3 (4.1) |
|
Ebstein's anomaly |
1 (0.2) |
- |
|
Congenital valve anomaly |
5 (1.0) |
2 (2.7) |
|
Arrhythmia |
2 (0.4) |
- |
|
Coronary problem |
1 (0.2) |
- |
|
AP window, truncus arteriosus |
12 (2.4) |
- |
|
PVS |
- |
1 (1.4) |
|
Unclassified |
3 (0.4) |
5 (6.8) |
|
Total |
491 (100) |
74 (100) |

Age <3 months
There were 1,084 patients; of them, 586 (54.1%) were male. The median hospital stay was 16 days (range, 0–277 days). A total of 845 (78.8%) biventricular repairs and 239 (22.0%) palliative procedures were performed; of them, 996 (91.9%) were in group A and 88 (8.1%) were in group B. The mean ABC score was 7.5±2.4. A RACHS-1 score of 2 was the most common. Complex procedures were performed in 607 patients (56.0%). The early mortality rate was 8.2%, while the late mortality rate was 3.0%. The early surgical mortality rate of other surgical eras (1984–1999) was 23.0%.
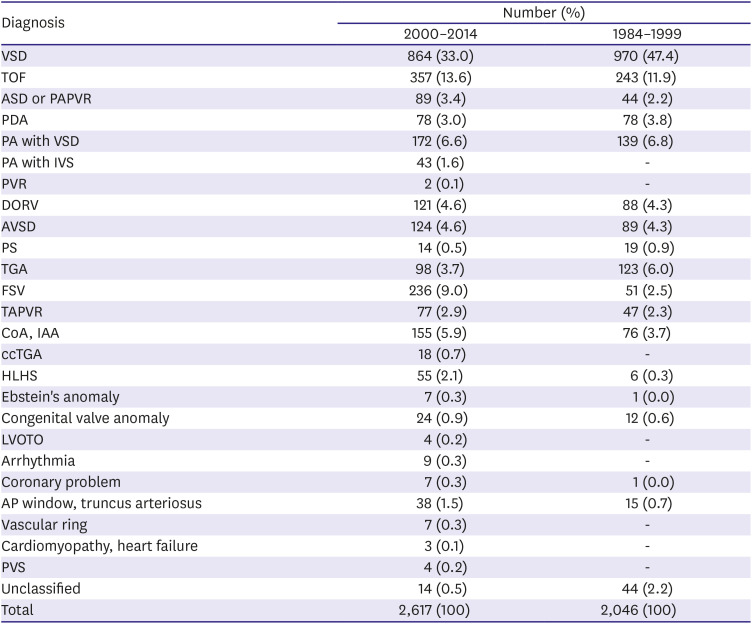
Infants
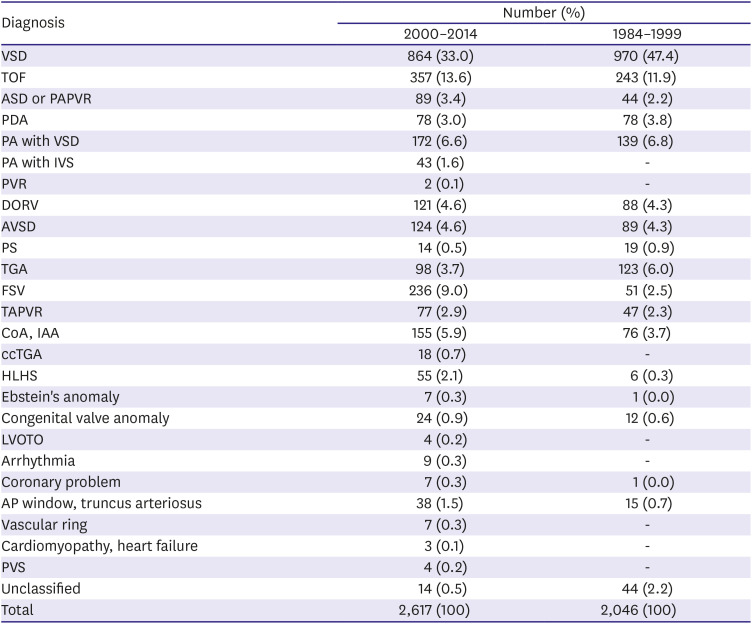
There were 2,617 patients; of them, 1,429 (54.6%) were male. The diagnosis prevalence is shown in
Table 4 and new diseases were added, including PVR, LVOTO, vascular ring, cardiomyopathy, and heart failure. The median hospital stay was 13 days (range, 0–277 days). A total of 2,617 operations were performed (2,323 [88.8%] in group A, 294 [11.2%] in group B), including 2,101 (80.3%) biventricular repairs and 516 (19.7%) palliative procedures. The mean ABC score was 7.2±2.1. A RACHS-1 score of 2 was the most common. Complex procedures were performed in 1,440 patients (55.0%). The early mortality rate was 6.0%, while the late mortality rate was 2.3%. The early surgical mortality rate of other surgical eras (1984–1999) was 15.8%.
Table 4
Infants' diagnosis prevalence
|
Diagnosis |
Number (%) |
|
2000–2014 |
1984–1999 |
|
VSD |
864 (33.0) |
970 (47.4) |
|
TOF |
357 (13.6) |
243 (11.9) |
|
ASD or PAPVR |
89 (3.4) |
44 (2.2) |
|
PDA |
78 (3.0) |
78 (3.8) |
|
PA with VSD |
172 (6.6) |
139 (6.8) |
|
PA with IVS |
43 (1.6) |
- |
|
PVR |
2 (0.1) |
- |
|
DORV |
121 (4.6) |
88 (4.3) |
|
AVSD |
124 (4.6) |
89 (4.3) |
|
PS |
14 (0.5) |
19 (0.9) |
|
TGA |
98 (3.7) |
123 (6.0) |
|
FSV |
236 (9.0) |
51 (2.5) |
|
TAPVR |
77 (2.9) |
47 (2.3) |
|
CoA, IAA |
155 (5.9) |
76 (3.7) |
|
ccTGA |
18 (0.7) |
- |
|
HLHS |
55 (2.1) |
6 (0.3) |
|
Ebstein's anomaly |
7 (0.3) |
1 (0.0) |
|
Congenital valve anomaly |
24 (0.9) |
12 (0.6) |
|
LVOTO |
4 (0.2) |
- |
|
Arrhythmia |
9 (0.3) |
- |
|
Coronary problem |
7 (0.3) |
1 (0.0) |
|
AP window, truncus arteriosus |
38 (1.5) |
15 (0.7) |
|
Vascular ring |
7 (0.3) |
- |
|
Cardiomyopathy, heart failure |
3 (0.1) |
- |
|
PVS |
4 (0.2) |
- |
|
Unclassified |
14 (0.5) |
44 (2.2) |
|
Total |
2,617 (100) |
2,046 (100) |

Age 1–2 years
There were 709 patients in this group; of them, 355 (50.1%) were male. The median hospital stay was 9 days (range, 0–291 days). A total of 709 procedures were performed (582 [82.1%] in group A, 127 [17.9%] in group B), including 614 (86.6%) biventricular repairs and 95 (13.4%) palliative procedures. The mean ABC score was 6.6±2.2. A RACHS-1 score of 2 was the most common. Complex procedures were performed in 362 patients (51.1%). The early mortality rate was 3.0%, while the late mortality rate was 1.2%.
Age 2–6 years
There were 1,053 patients; of them, 554 (52.6%) were male. The median hospital stay was 10 days (range, 0–135 days). A total of 1,053 procedures were performed (892 [84.7%] in group A, 161 [15.3%] in group B), including 805 (76.4%) biventricular repairs and 248 (23.6%) palliative procedures. The mean ABC score was 6.9±2.2. A RACHS-1 score of 2 was the most common. Complex procedures were performed in 565 patients (53.7%). The early mortality rate was 2.3%, while the late mortality rate was 1.5%.
Age 6–10 years
There were 510 patients; of them, 263 (51.6%) were male. The median hospital stay was 9 days (range, 0–254 days). A total of 510 procedures were performed (394 [77.3%] in group A, 116 [22.7%] in group B), including 466 (91.4%) biventricular repairs and 44 (8.6%) palliative procedures. The mean ABC score was 6.3±2.0. A RACHS-1 score of 2 was the most common. Complex procedures were performed in 224 patients (43.9%). The early mortality rate was 2.5%, while the late mortality rate was 1.8%.
Age 10–18 years
There were 678 patients; of them, 346 (51.0%) were male. The median hospital stay was 10 days (range, 0–105 days). A total of 678 procedures were performed (546 [80.5%] in group A, 132 [19.5%] in group B), including 631 (93.1%) biventricular repairs and 47 (6.9%) palliative procedures. The mean ABC score was 6.3±2.1. A RACHS-1 score of 2 was the most common. Complex procedures were performed in 376 patients (55.5%). The early mortality rate was 1.8%, while the late mortality rate was 1.5%.
Age ≥18 years
There were 1,032 patients; of them, 450 (43.6%) were male. The median hospital stay was 11 days (range, 0–372 days). A total of 1,032 procedures were performed: 994 (96.3%) biventricular repairs and 38 (3.7%) palliative procedures; of them, 747 (72.4%) were performed in 12 hospitals, while the other 285 (27.6%) were performed in the other 52 hospitals. The mean ABC score was 5.4±2.2. A RACHS-1 score of 2 was the most common. Complex procedures were performed in 401 patients (38.9%). The early mortality rate was 2.8%, while the late mortality rate was 1.3%.
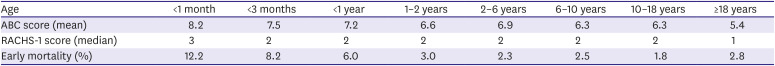
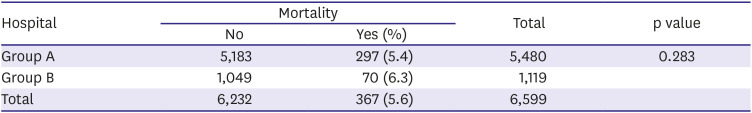
Table 5 depicts the ABC score, RACHS-1 score, and early mortality rate by patient age.
Table 5
ABC score, RACHS-1 score, and early mortality rate by patient age
|
Age |
<1 month |
<3 months |
<1 year |
1–2 years |
2–6 years |
6–10 years |
10–18 years |
≥18 years |
|
ABC score (mean) |
8.2 |
7.5 |
7.2 |
6.6 |
6.9 |
6.3 |
6.3 |
5.4 |
|
RACHS-1 score (median) |
3 |
2 |
2 |
2 |
2 |
2 |
2 |
1 |
|
Early mortality (%) |
12.2 |
8.2 |
6.0 |
3.0 |
2.3 |
2.5 |
1.8 |
2.8 |

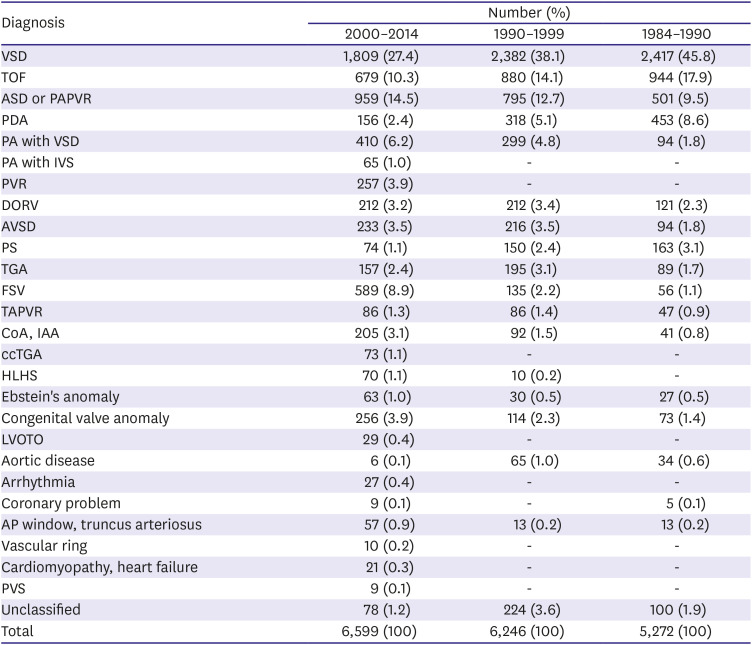
Analysis of surgical mortality by patient diagnosis
We described the number of interventions for each diagnosis, although these procedures were not included in the surgical number.
Ventricular septal defect
There were 1,809 patients; of them, 940 (52.0%) were male. The median age was 1.1 years (range, 0–66.5 years). The median hospital stay was 9 days (range, 0–372 days). Ten (0.6%) palliative procedures were performed: 7 pulmonary artery bandings, 1 bidirectional cavopulmonary shunt, and 2 VSD partial closures. A total of 1,809 procedures were performed: 1,362 (75.3%) in group A, and the other 447 (24.7%) in group B. Two VSD device closures were performed. The early mortality rate was 1.4%, while the late mortality rate was 0.6%.
Tetralogy of Fallot
There were 679 patients; of them, 379 (55.8%) were male. Patients who received PVR were excluded. The median patient age was 11.5 months (range, 0.1 months–65.1 years). The median hospital stay was 11 days (range, 0–240 days). There were 44 (6.5%) palliative procedures. A total of 679 procedures were performed: 579 (85.3%) in group A vs. 100 (14.7%) in group B. A total of 31 interventional procedures like pulmonary artery balloon dilatation were performed. The early mortality rate was 4.6%, while the late mortality rate was 0.9%.
Atrial septal defect or partial anomalous pulmonary venous return
There were 959 patients; of them, 314 (32.7%) were male. The median patient age was 12.6 months (range, 3 months–69.5 years). The median hospital stay was 8 days (range, 1–291 days). A total of 959 operations were performed: 643 (67.0%) in group A and 316 (33.0%) in group B. There were 23 PAPVR cases with one of surgical mortality. There were 95 ASD device closures. The early mortality rate was 1.3%, while the late mortality rate was 0.9%.
Patent ductus arteriosus
There were 156 patients; of them, 56 (35.9%) were male. The median patient age was 2.1 years (range, 3 months–62.9 years). The median hospital stay was 10 days (range, 1–122 days). A total of 156 procedures were performed: 83 (53.2%) in group A and 73 (46.8%) in group B. There were 137 patent ductus arteriosus (PDA) device closures. The early mortality rate was 2.6%, while the late mortality rate was 1.3%.
Pulmonary atresia with ventricular septal defect
There were 410 patients; of them, 223 (54.4%) were male. The median patient age was 1.4 years (range, 0–52.6 years). The median hospital stay was 14 days (range, 0–168 days). A total of 410 procedures were performed: 392 (95.6%) in group A and 18 (4.4%) in group B. There were 280 (68.3%) biventricular repairs and 130 (31.7%) palliative procedures. A total of 111 (27.1%) patients had a major aortopulmonary collateral artery. There were 3 (0.7%) patients with a RACHS-1 score of 1, 85 (20.7%) with a RACHS-1 score of 2, 219 (53.4%) with a RACHS-1 score of 3, and 103 (25.1%) with a RACHS-1 score of 4. The early mortality rate was 4.9%, while the late mortality rate was 3.3%.
Pulmonary atresia with intact ventricular septum
There were 65 patients; of them, 34 (52.3%) were male. The median patient age was 6.3 months (range, 0–29.3 years). The median hospital stay was 16 days (range, 7–169 days). Of the 65 procedures, 64 (98.5%) were in group A, while the other 1 (1.5%) was in group B. There were 29 (44.6%) biventricular repairs and 36 (55.4%) palliative procedures. There were 6 interventions like right ventricular outflow tract balloon dilatation. The early mortality rate was 4.6%, while the late mortality rate was 6.5%.
Double-outlet right ventricle
There were 212 patients; of them, 124 (58.5%) were male. The median patient age was 0.7 years (range, 0–53 years). The median hospital stay was 14 days (range, 0–220 days). Of the 212 procedures, 201 (94.8%) were in group A, while the other 11 (5.2%) were in group B. There were 184 (86.8%) biventricular repairs and 28 (13.2%) palliative procedures. Of the 212 patients, 106 (50.0%) were treated with double-outlet right ventricle (DORV) with VSD (subaortic type), 73 (34.4%) with DORV with VSD for pulmonary stenosis (PS) (TOF type), 20 (9.4%) with DORV with VSD (subpulmonic type) (Taussig-Bing anomaly), 12 (5.7%) with DORV with VSD (remote type), and 1 (0.5%) patient with DORV with intact ventricular septum. Three (1.4%) patients had a RACHS-1 score of 1, 49 (23.1%) had a RACHS-1 score of 2, 151 (71.2%) had a RACHS-1 score of 3, 5 (2.4%) had a RACHS-1 score of 4, and 4 (1.9%) had a RACHS-1 score of 5. The early mortality rate was 6.1%, while the late mortality rate was 3.0%.
Atrioventricular septal defect
There were 233 patients; of them, 98 (42.1%) were male. The median patient age was 0.7 years (range, 10 days–68.2 years). The median hospital stay was 13 days (range, 1–157 days). Of the 233 procedures, 205 (88.0%) were in group A, while the other 28 (12.0%) were in group B. A total of 214 (91.8%) biventricular repairs and 19 (8.2%) palliative procedures were performed: There were 167 (71.7%) patients with complete atrioventricular septal defect (AVSD), 54 (23.2%) with partial AVSD, 6 (2.6%) with intermediate AVSD, and 6 (2.6%) with complete AVSD accompanying TOF. The early mortality rate was 5.6%, while the late mortality rate was 2.3%.
Pulmonary stenosis
There were 74 patients; of them, 43 (58.1%) were male. The median patient age was 6.3 years (range, 10 days–54.1 years). The median hospital stay was 13 days (range, 3–50 days). Of the 74 patients, 58 (78.4%) were in group A, while the other 16 (21.6%) were in group B. There were 72 (97.3%) biventricular repairs and 2 (2.7%) palliative procedures. A total of 51 interventions like pulmonary valve balloon dilatation were performed. The early mortality rate was 2.7%, while the late mortality rate was 0%.
Transposition of the great arteries
There were 157 patients; of them, 111 (70.7%) were male. The median patient age was 0.3 years (range, 0–38.5 years). The median hospital stay was 15 days (range, 0–218 days). Of the 157 procedures, 151 (96.2%) were performed in group A versus 6 (3.8%) in group B. A total of 141 (89.8%) biventricular repairs and 16 (10.2%) palliative procedures were performed: 57 (36.3%) with transposition of the great arteries (TGA) with IVS, 51 (32.5%) with TGA with VSD, and 49 (31.2%) with TGA with VSD and PS. One (0.6%) patient had a RACHS-1 score of 1, 14 (8.9%) had a RACHS-1 score of 2, 86 (54.8%) had a RACHS-1 score of 3, and 56 (35.7%) had a RACHS-1 score of 4. There were 9 interventions like coronary artery stent insertion. The early mortality rate was 8.3%, while the late mortality rate was 0%.
Functional single ventricle
There were 589 patients; of them, 378 (64.2%) were male. This patient group excluded those with hypoplastic left heart syndrome (HLHS). The median patient age was 1.9 years (range, 3 days–45.6 years). The median hospital stay was 18 days (range, 0–181 days). Of the 589 procedures, 573 (97.3%) were performed in group A vs. 16 (2.7%) in group B. Four (0.7%) patients had a RACHS-1 score of 1, 184 (31.2%) had a RACHS-1 score of 2, 382 (64.9%) patients had a RACHS-1 score of 3, 11 (1.9%) had a RACHS-1 score of 4, and 8 (1.4%) had a RACHS-1 score of 6. A total of 37 interventional procedures like cardiac catheter examinations were performed. The early mortality rate was 7.5%, while the late mortality rate was 4.2%.
Total anomalous pulmonary venous return
There were 86 patients; of them, 47 (54.7%) were male. The median patient age was 1.7 months (range, 0–37.8 years). The median hospital stay was 17 days (range, 0–236 days). Of the 86 procedures, 81 (94.2%) were performed in group A, while the other 5 (5.8%) were performed in group B. The early mortality rate was 12.8%, while the late mortality rate was 4%.
Coarctation of the aorta and interrupted aortic arch
There were 205 patients; of them, 119 (58.0%) were male. The median patient age was 1.4 months (range, 0.1 months–47.4 years). The median hospital stay was 15 days (range, 3–277 days). Of the 205 procedures, 188 (91.7%) operations were in group A, while the other 17 (8.3%) were in group B. There were 121 (59.0%) patients with coarctation of the aorta (CoA) with VSD, 32 (15.6%) with interrupted aortic arch (IAA) with VSD, 45 (22.0%) with isolated CoA, and 7 (3.4%) with another aortic arch anomaly. A total of 11 interventions like aortic re-coarctation balloon dilatation were performed. The early mortality rate was 4.9%, while the late mortality rate was 1.0%.
Congenitally corrected transposition of the great arteries
There were 73 patients; of them, 42 (57.5%) were male. The median patient age was 5 years (range, 0–56.1 years). The median hospital stay was 15 days (range, 32–77 days). Of the 73 procedures, 72 (98.6%) were performed in group A, while the other 1 (1.4%) was performed in group B. There were 22 (30.1%) patients with ccTGA with VSD, 45 (61.6%) patients with ccTGA with VSD, PS, and 6 (8.2%) patients with isolated ccTGA. The early mortality rate was 12.3%, while the late mortality rate was 10.9%.
Hypoplastic left heart syndrome
These data included operations for all disease stages. There were 70 patients; of them, 45 (64.3%) were male. The median patient age was 3.4 months (range, 0–4.3 years). The median hospital stay was 27.5 days (range, 0–196 days). All 70 (100%) operations were performed in group A. The early mortality rate was 18.6%, while the late mortality rate was 1.8%.
Ebstein's anomaly
There were 63 patients; of them, 24 (38.1%) were male. The median patient age was 16.3 years (range, 0–53.7 years). The median hospital stay was 13 days (range, 5–62 days). Of the 63 procedures, 57 (90.5%) were performed in group A, while the other 6 (9.5%) were in group B. There were 60 (95.2%) biventricular repairs and 3 (4.8%) palliative procedures. The early mortality rate was 1.6%, while the late mortality rate was 16%.
Congenital valve anomaly
There were 256 patients; of them, 128 (50.0%) were male. The median patient age was 13.3 years (range, 0–71.5 years). The median hospital stay was 13 days (range, 5–62 days). Of the 256 procedures, 245 (95.7%) were performed in group A, while the other 11 (4.3%) were performed in group B. The early mortality rate was 3.1%, while the late mortality rate was 16%.
Left ventricular outflow tract obstruction
There were 29 patients; of them, 21 (72.4%) were male. The median patient age was 4.8 years (range, 2.4 months–38.1 years). The median hospital stay was 8 days (range, 5–109 days). Of the 29 procedures, 23 (79.3%) were performed in group A, while the other 6 (20.7%) were performed in group B. The early mortality rate was 0%, while the late mortality rate was 3.4%.
Aortic disease
There were 6 patients; of them, 4 (66.7%) were male. The median patient age was 13.1 years (range, 5.9–17.7 years). The median hospital stay was 9 days (range, 6–32 days). All 6 (100%) operations were performed in group A. The early mortality rate was 16.7%, while the late mortality rate was 3.4%.
Arrhythmia
There were 27 patients; of them, 13 (48.1%) were male. The median patient age was 13.1 years (range, 0–62.2 years). The median hospital stay was 6 days (range, 3–27 days). All 27 (100%) operations were performed in group A. There were 25 permanent pacemaker insertions, 1 Maze operation, and 1 atrial ablation. A total of 46 interventions like radiofrequency catheter ablation were performed. The early mortality rate was 3.7%, while the late mortality rate was 0%.
Coronary anomaly
There were 9 patients; of them, 3 (33.3%) were male. The median patient age was 5 months (range, 10 days–39.9 years). The median hospital stay was 15 days (range, 8–23 days). Of the 9 procedures, 8 (88.9%) were performed in group A, while the other 1 (11.1%) was performed in group B. There was 1 neonate (11.1%) and 7 infants (77.8%). The early and late mortality rates were 0%.
Aortopulmonary window, truncus arteriosus
There were 57 patients; of them, 34 (59.6%) were male. The median patient age was 4.2 months (range, 3 days–20.6 years). The median hospital stay was 20 days (range, 5–147 days). Of the 57 procedures, 54 (94.7%) were performed in group A, while the other 3 (5.3%) were performed in group B. There were 13 neonates (22.8%) and 38 infants (66.7%). The early mortality rate was 7.0%, while the late mortality rate was 5.7%.
Vascular ring
There were 10 patients; of them, 5 (50.0%) were male. The median patient age was 4.4 months (range, 1.3 months–39.9 years). The median hospital stay was 10.5 days (range, 4–104 days). Of the 10 procedures, 8 (80.0%) were performed in group A, while the other 2 (20.0%) were performed in group B. The early mortality rate was 10.0%, while the late mortality rate was 0%.
Cardiomyopathy, heart failure
There were 21 patients; of them, 12 (57.1%) were male. The median patient age was 8.6 years (range, 2.7 months–57.5 years). The median hospital stay was 26 days (range, 9–117 days). Of the 21 procedures, 20 (95.2%) were performed in group A, while the other 1 (4.8%) was performed in group B. There were 11 heart transplantations, with an early mortality rate of 9.1%. The overall early mortality rate was 19%, while the late mortality rate was 17.6%.
Pulmonary vein stenosis
All of the cases were isolated PVS; these data did not include postoperative complications. There were 9 patients; of them, 2 (22.2%) were male. The median patient age was 8.6 months (range, 2.4 months–19.9 years). The median hospital stay was 17 days (range, 6–54 days). Of the 9 procedures, 6 (66.7%) were performed in group A, while the other 3 (33.3%) were performed in group B. The early mortality rate was 11.1%, while the late mortality rate was 50.0%.
Pulmonary valve replacement
There were 257 patients; of them, 163 (63.4%) were male. The median patient age was 17 years (range, 4 months–59.9 years). The median hospital stay was 11 days (range, 0–254 days). Of the 257 procedures, 249 (96.9%) were performed in group A, while the other 8 (3.1%) were performed in group B. A total of 217 (84.4%) patients had TOF, 24 (9.3%) had PA with VSD, and 16 (6.2%) had DORV. The early mortality rate was 1.6%, while the late mortality rate was 1.6%.
Unclassified
There were 76 patients; of them, 41 (53.9%) were male. The median patient age was 10.9 years (range, 3 days–50.5 years). The median hospital stay was 18 days (range, 1–109 days). Of the 76 procedures, 55 (72.4%) were performed in group A, while the other 21 (27.6%) were performed in group B. These diseases included pectus excavatum, sternal instability, phrenic nerve palsy, congenital tracheal stenosis, and constrictive pericarditis. The early mortality rate was 5.3%, while the late mortality rate was 1.4%.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download