Congenital heart disease (CHD) is the most common congenital anomaly, accounting for almost 30% of all major birth defects. Reported birth prevalence of CHD worldwide is around 9 per 1,000 live births, with significant geographical differences.1) The highest CHD birth prevalence was reported in Asia, with 9.3 per 1,000 live births, whereas 8.2 and 6.9 per 1,000 live births in Europe and North America, respectively.1) The incidence of ‘significant CHD’, which will require surgery before one year of age, was reported to be 3.2/1,000 live births in a population based study in North America.2) A worldwide annual birth rate is around 150 million, which corresponds to 1.35 million live births with CHD and 480,000 births with significant CHDs every year.2)3)
In 2017, 5.4 million children under 5 years of age died worldwide, of whom 214,214 children with CHD died, representing 3.97% of all causes of death and 31.5 deaths per 100,000 poplulation.4) The overall mortality rates in children has declined significantly, by half globally over the past two decades, but deaths and disabilities in children with CHD have been steadily increased in countries with low incomes and high fertility rates.4)5) There are the wide disparities of health system resources to treat CHD between countries, in terms of per capita income, education level, fertility rate, and pediatric cardiac experts and cardiovascular centers.4)6) Indeed, about 90% of CHD patients do not have adequate access to diagnosis and treatment, and 75% do not have access to cardiac surgery worldwide, indicating that CHD is still a great health care burden worldwide.6)7)8)
In this issue of the Korean Circulation Journal, Shin et al.9) reported the recent surgical outcomes of CHD in Korea based on the Korea Heart Foundation (KHF) data. The surgical data of 6,599 CHD patients with financial support from KHF in the recent 15-year period (2000–2014, the recent era) were analyzed and compared with those of the previous reports on patients who had CHD surgery from 1984 to 1999 (the past era). This study population represents about 12% of all CHD surgical volume in Korea during the same period, in which 54,144 CHD surgeries were performed, based on the KHF Annual Report on “The Present Status of Cardiovascular Surgery in Korea”.10) Given that no national data on surgical outcomes is available until recently, we may assume that the results of this study represents trends in CHD surgical outcomes over the last three decades in Korea.
The main finding of the study is surgical mortality rates by age at surgery and diagnosis. Compared to mortality rates in the past era, the overall mortality rates decreased significantly in the recent era, with an early mortality rate of 3.8% (vs. 8.6% in the past era) and late mortality rate of 1.8% (vs. 5.3%). Especially, substantial improvements were achieved in patients under one year of age at surgery. Compared with mortality rates in the past era, early mortality rates in neonates, patients under 3 months of age, and infants have decreased significantly, with 12.2% (vs. 29.7% in the past era), 8.2% (vs. 23.0%), and 6.0% (vs. 15.8%), respectively. Mortality rates in patients over 1 year of age ranged from 1.8% to 3.0%.
It is also noteworthy that the volume of neonatal surgical cases has increased significantly in the recent era with 491 patients (7.4% of all patients), while 74 patients (0.6%) in the past era. About 30% of neonatal surgeries were palliative procedures for complex CHD. The most common diagnosis in neonatal surgery was coarctation of the aorta or interrupted aortic arch (15.9%), followed by transposition of the great arteries (14.7%) and pulmonary atresia with ventricular septal defect (10.8%). It is encouraging that surgical outcomes improved substantially in neonates with more complex CHD, which needed more complicated surgical procedures in the recent era. Nevertheless, mortality rates were still relatively high (>10%) in patients with hypoplastic left heart syndrome, total anomalous pulmonary venous return, congenitally-corrected transposition of the great arteries, and some aortic diseases (diagnosis not specified).
Lastly, another notable data is the number of overseas patients, with 491 patients (7.4% of all patients) from 30 countries, mainly nearby Asian countries. As the health care system and resources improved dramatically during the past two decades, recent overall surgical outcomes have improved significantly in Korea, while there is still a great shortage of resources to treat these patients in some countries worldwide.
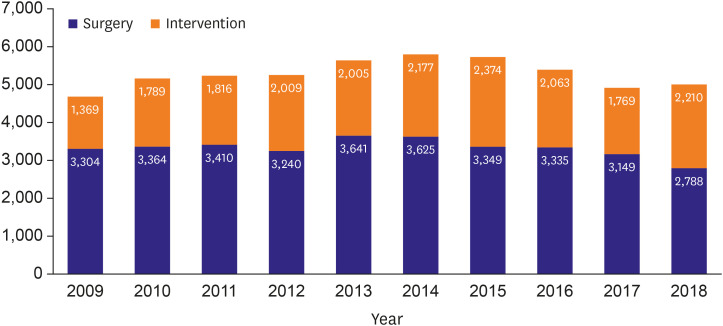
Treatment of CHD by surgery or intervention is always relatively expensive, requiring specialized equipment and facilities, and well-trained pediatric cardiologists and cardiac surgeons. Most patients with CHD require life-long follow up and care, furthermore many patients also need additional surgeries or interventions. Given that the incidence of CHD is similar worldwide, the burden of treating these patients is very challenging in countries with low oncome and high fertility rates.6) In addition, in underdeveloped countries infectious diseases and nutritional deficiencies are the major causes of death, while CHD accounts for a small portion of childhood mortality, less than 5% of all-cause mortality, which result in insufficient investment in CHD treatment.4)6) Until the early 1980s, the burden of CHD in Korea was quite high. In 1984, the year KHF was established, the gross national income per capita was $2,378 and the annual birth rate was 675,000 (Korean Statistical Information Service, http://kosis.kr/search/search.do). Some of the CHD patients had to go abroad to undergo surgery at the time, mainly due to financial difficulties. Since the establishment of KHF, the volume of CHD surgery or intervention has increased dramatically, and in 2014, a total of 5,802 surgeries or interventions were performed with a total mortality rate of only 1.6% (Figure 1).10)
The great achievements in the treatment of CHD in Korea are thought to be fueled by the support of KHF, and have been boosted by increase in per capita income, the national health insurance system, decrease in fertility rate, and high education level. These experiences in Korea could be potential solutions to decrease the burdens of CHD treatment in underdeveloped countries. However, this is a very complex problem because those countries have more urgent socio-economic and other public health issues than CHD.4)6) Given that the main barriers to the treatment of CHD are poverty and limited manpower, especially cardiac surgeons, it will be difficult and time consuming to improve the situations. Therefore, as Korea has been doing recently, a practical, but not fundamental, way for solving the problems at this time is that developed countries invite CHD patients for surgery, invite medical staffs for training, or have medical teams go to underdeveloped countries, treat patients, and help train local doctors.
Currently, CHD is not a ‘burden’ in Korea. As the authors concluded, surgical outcomes improved significantly, comparable to those of other developed countries, and Korea has become a country to help other underdeveloped countries. Obviously, this achievement was made through the great socio-economic development of Korea. Additionally, I believe that the dedication of Korean doctors to care for CHD patients also contributed to that. Because the burden of CHD in underdeveloped countries are still serious, international cooperation is urgently needed to increase investments in pediatric cardiac care across the world.5)
References
1. van der Linde D, Konings EE, Slager MA, et al. Birth prevalence of congenital heart disease worldwide: a systematic review and meta-analysis. J Am Coll Cardiol. 2011; 58:2241–2247. PMID: 22078432.
2. Peyvandi S, Baer RJ, Chambers CD, et al. Environmental and socioeconomic factors influence the live-born incidence of congenital heart disease: a population-based study in California. J Am Heart Assoc. 2020; 9:e015255. PMID: 32306820.

3. Hoffman JI, Kaplan S. The incidence of congenital heart disease. J Am Coll Cardiol. 2002; 39:1890–1900. PMID: 12084585.

4. Institute for Health Metrics and Evaluation. Global Burden of Disease 2017 [Internet]. Seattle (WA): Institute for Health Metrics and Evaluation;2018. cited 2020 May 1. Available from: http://ghdx.healthdata.org/gbd-results-tool.
5. Zheleva B, Atwood JB. The invisible child: childhood heart disease in global health. Lancet. 2017; 389:16–18. PMID: 27989557.

6. Hoffman JI. The global burden of congenital heart disease. Cardiovasc J Afr. 2013; 24:141–145. PMID: 24217047.
7. Tchervenkov CI, Jacobs JP, Bernier PL, et al. The improvement of care for paediatric and congenital cardiac disease across the world: a challenge for the World Society for Pediatric and Congenital Heart Surgery. Cardiol Young. 2008; 18(Suppl 2):63–69.

8. Bernier PL, Stefanescu A, Samoukovic G, Tchervenkov CI, et al. The challenge of congenital heart disease worldwide: epidemiologic and demographic facts. Semin Thorac Cardiovasc Surg Pediatr Card Surg Annu. 2010; 13:26–34. PMID: 20307858.

9. Shin HJ, Park YH, Cho BK. Recent surgical outcomes of congenital heart disease according to Korea Heart Foundation data. Korean Circ J. 2020; 50:677–690.

10. The Korean Heart Foundation. The present status of cardiovascular surgery in Korea [Internet]. Seoul: The Korean Heart Foundation;2020. cited 2020 May 1. Available from: https://new.heart.or.kr.
Figure 1
The number of surgery and intervention for congenital heart disease in the recent 10 years, based on the Korean Heart Foundation annual report on “The Present Status of Cardiovascular Surgery in Korea”.10)




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download