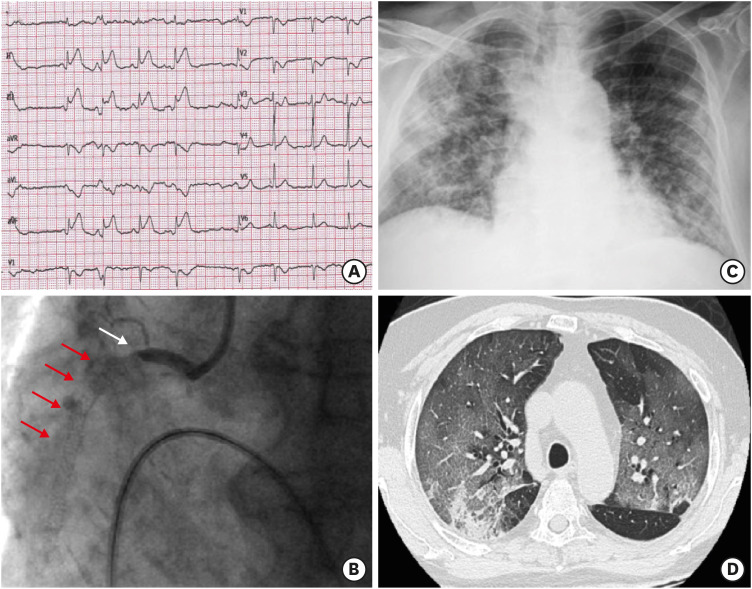
A 79-year-old man presented at our hospital with acute myocardial infarction after he had been successfully treated with percutaneous coronary intervention 2 years earlier, and discharged on dual antiplatelet therapy (clopidogrel 75 mg/day for 12 months and aspirin 100 mg/day indefinitely). The patient had remained asymptomatic after the procedure but had started complaining of fever and cough the week before hospitalization. An intense chest pain was present at admission while the electrocardiogram showed a significant ST-elevation in the inferior leads (Figure 1A). Coronary angiography documented an occlusive in-stent thrombotic lesion of the proximal right coronary artery, that was immediately treated (Figure 1B). A severe bilateral pneumonia was documented at chest X-ray and confirmed at computed tomography (Figure 1C and D). Nasopharyngeal swab tested positive for coronavirus disease 2019 (COVID-19) infection. Arterial blood gas analysis on oxygen therapy showed severe hypoxemia with a PaO2/FiO2 ratio of 100. The patient was treated with noninvasive ventilation but died a few hours later of severe acute respiratory distress syndrome.
Patients with chronic coronary artery disease have an increased probability of developing an acute coronary syndrome (ACS) during acute infections.1) COVID-19 may affect the cardiovascular system in multiple ways and these mechanisms can interact each other: direct myocardial involvement mediated via angiotensin-converting enzyme 22); hypoxemia due to severe COVID-19 infection3); cytokines storm and high concentrations of inflammatory mediators that could lead to atherosclerotic plaque instability and rupture4); repeated floods of catecholamines due to anxiety.5)
This case of diffuse COVID-19 pneumonia seems to confirm the role of severe infection as a precipitating factor for ACS in patients with chronic coronary artery disease, and causal relationship.
References
1. Smeeth L, Thomas SL, Hall AJ, Hubbard R, Farrington P, Vallance P. Risk of myocardial infarction and stroke after acute infection or vaccination. N Engl J Med. 2004; 351:2611–2618. PMID: 15602021.

2. Oudit GY, Kassiri Z, Jiang C, et al. SARS-coronavirus modulation of myocardial ACE2 expression and inflammation in patients with SARS. Eur J Clin Invest. 2009; 39:618–625. PMID: 19453650.

3. Zheng YY, Ma YT, Zhang JY, Xie X. COVID-19 and the cardiovascular system. Nat Rev Cardiol. 2020; 17:259–260. PMID: 32139904.

4. Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020; 395:497–506. PMID: 31986264.

5. Zvonarev V. Takotsubo cardiomyopathy: medical and psychiatric aspects. Role of psychotropic medications in the treatment of adults with “Broken Heart” syndrome. Cureus. 2019; 11:e5177. PMID: 31423403.

Figure 1
(A) Significant ST-segment elevation in inferior leads on electrocardiogram at presentation. (B) Acute occlusion of the proximal right coronary artery at the edge of previously implanted stents (arrows). (C) Bilateral diffuse airspace opacities on chest X-ray. (D) Cross-sectional computed tomography-scan showing extensive ground-glass opacifications involving both the lung parenchymas with areas of consolidation in the right lower lobe posterior segment.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download