2. Wang Z, Chen Z, Zhang L, et al. Status of hypertension in China: results from the China hypertension survey, 2012–2015. Circulation. 2018; 137:2344–2356. PMID:
29449338.
3. Cheung BM, Ong KL. The challenge of managing hypertension. In : Finkel ML, editor. Public Health in the 21st Century. Vol. 1. Santa Barbara (CA): Praeger Publishing;2011. p. 117–128.
4. Kim HC, Ihm SH, Kim GH, et al. 2018 Korean Society of Hypertension guidelines for the management of hypertension: part I-epidemiology of hypertension. Clin Hypertens. 2019; 25:16. PMID:
31388451.

5. Cheung BM, Wat NM, Man YB, et al. Relationship between the metabolic syndrome and the development of hypertension in the Hong Kong cardiovascular risk factor prevalence study-2 (CRISPS2). Am J Hypertens. 2008; 21:17–22. PMID:
18091739.

6. Cheung BM, Wat NM, Tam S, et al. Components of the metabolic syndrome predictive of its development: a 6-year longitudinal study in Hong Kong Chinese. Clin Endocrinol (Oxf). 2008; 68:730–737. PMID:
17980012.

7. Cheung BM, Wat NM, Tso AW, et al. Association between raised blood pressure and dysglycemia in Hong Kong Chinese. Diabetes Care. 2008; 31:1889–1891. PMID:
18556342.

8. Janus ED. Epidemiology of cardiovascular risk factors in Hong Kong. Clin Exp Pharmacol Physiol. 1997; 24:987–988. PMID:
9406673.

9. Ong KL, Tso AW, Lam KS, Cheung BM. Gender difference in blood pressure control and cardiovascular risk factors in Americans with diagnosed hypertension. Hypertension. 2008; 51:1142–1148. PMID:
18259031.

10. Wilber JA, Barrow JG. Hypertension--a community problem. Am J Med. 1972; 52:653–663. PMID:
5027555.

11. Kotseva K, Wood D, De Bacquer D, et al. EUROASPIRE IV: a European Society of Cardiology survey on the lifestyle, risk factor and therapeutic management of coronary patients from 24 European countries. Eur J Prev Cardiol. 2016; 23:636–648. PMID:
25687109.
12. Williams B, Mancia G, Spiering W, et al. 2018 ESC/ESH guidelines for the management of arterial hypertension. Eur Heart J. 2018; 39:3021–3104. PMID:
30165516.
13. Bhatt DL, Kandzari DE, O'Neill WW, et al. A controlled trial of renal denervation for resistant hypertension. N Engl J Med. 2014; 370:1393–1401. PMID:
24678939.

14. Zhen Z, Liao SY, Zhu ZY, et al. Catheter-based splanchnic denervation for treatment of hypertensive cardiomyopathy. Hypertension. 2019; 74:47–55. PMID:
31132949.

15. Lobo MD, Ott C, Sobotka PA, et al. Central iliac arteriovenous anastomosis for uncontrolled hypertension: one-year results from the ROX CONTROL HTN trial. Hypertension. 2017; 70:1099–1105. PMID:
29061728.
16. Nakagami H, Morishita R. Recent advances in therapeutic vaccines to treat hypertension. Hypertension. 2018; 72:1031–1036. PMID:
30354822.

17. Phillips MI. Gene therapy for hypertension: the preclinical data. Hypertension. 2001; 38:543–548. PMID:
11566928.
18. Warren HR, Evangelou E, Cabrera CP, et al. Genome-wide association analysis identifies novel blood pressure loci and offers biological insights into cardiovascular risk. Nat Genet. 2017; 49:403–415. PMID:
28135244.
19. Calkins K, Devaskar SU. Fetal origins of adult disease. Curr Probl Pediatr Adolesc Health Care. 2011; 41:158–176. PMID:
21684471.

20. Parkinson JR, Hyde MJ, Gale C, Santhakumaran S, Modi N. Preterm birth and the metabolic syndrome in adult life: a systematic review and meta-analysis. Pediatrics. 2013; 131:e1240–63. PMID:
23509172.

21. Cheung BM. Hypertension: a weighty problem in children. Postgrad Med J. 2017; 93:647. PMID:
28823997.

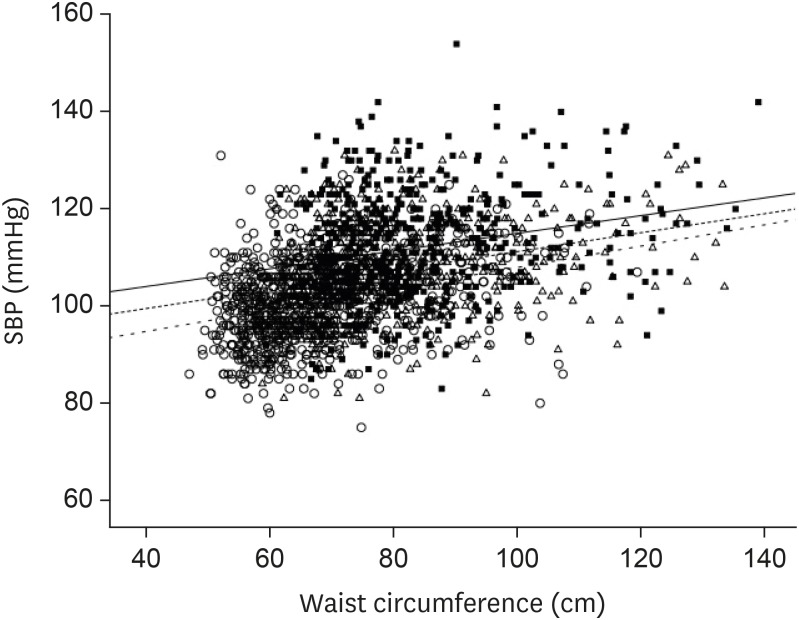
22. Cheung AJ, Cheung BMY. Association of increased systolic blood pressure in children with obesity and the metabolic syndrome. J Hum Hypertens. 2015; 29(Suppl1):S15.
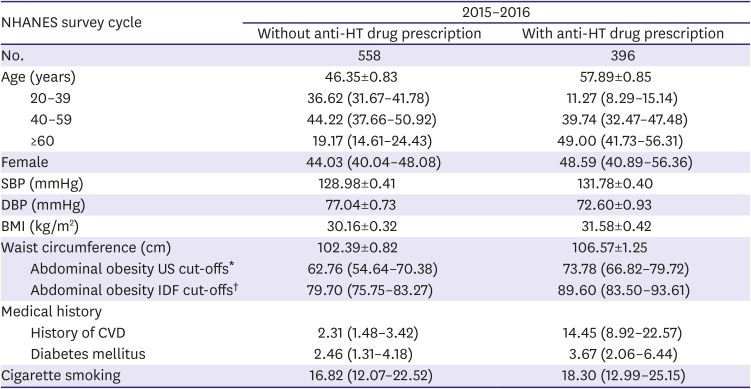
23. Ong KL, Cheung BM, Man YB, Lau CP, Lam KS. Prevalence, awareness, treatment, and control of hypertension among United States adults 1999–2004. Hypertension. 2007; 49:69–75. PMID:
17159087.

24. Muntner P, Carey RM, Gidding S, et al. Potential U.S. population impact of the 2017 ACC/AHA high blood pressure guideline. J Am Coll Cardiol. 2018; 71:109–118. PMID:
29146532.

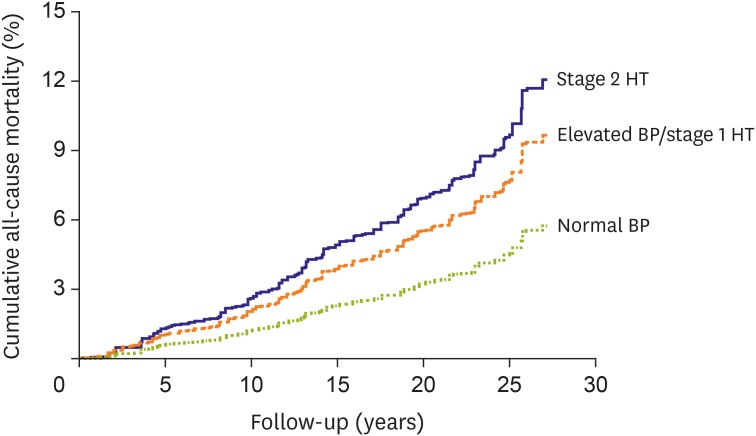
25. Son JS, Choi S, Kim K, et al. Association of blood pressure classification in Korean young adults according to the 2017 American College of Cardiology/American Heart Association guidelines with subsequent cardiovascular disease events. JAMA. 2018; 320:1783–1792. PMID:
30398603.

26. Yano Y, Reis JP, Colangelo LA, et al. Association of blood pressure classification in young adults using the 2017 American College of Cardiology/American Heart Association blood pressure guideline with cardiovascular events later in life. JAMA. 2018; 320:1774–1782. PMID:
30398601.

27. Or B, Tsoi MF, Cheung TT, Cheung BM. Decreased survival in young adults with stage 1 and 2 hypertension in the National Health and Nutrition Examination Survey III. Hong Kong Med J. 2020; 26(Suppl 1):14.
28. Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: executive summary: a report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines. Hypertension. 2018; 71:1269–1324. PMID:
29133354.

29. SPRINT Research Group, Wright JT Jr, Williamson JD, et al. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med. 2015; 373:2103–2116. PMID:
26551272.

30. Fei Y, Tsoi MF, Cheung BM. Determining the optimal systolic blood pressure for hypertensive patients: a network meta-analysis. Can J Cardiol. 2018; 34:1581–1589. PMID:
30414702.

31. Tsoi MF, Fei Y, Cheung TT, Cheung BM. Characteristics of Americans with stage-1 hypertension: United States National Health Nutrition and Examination Survey 2011–2016. Hong Kong Med J. 2018; 24(Suppl 1):54.
32. Ng M, Fleming T, Robinson M, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2014; 384:766–781. PMID:
24880830.
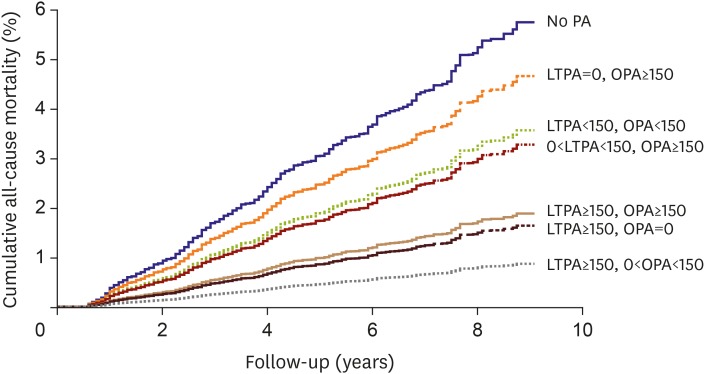
33. Or B, Tsoi MF, Cheung TT, Cheung BM. Leisure time, occupational aerobic physical activity, and mortality risk in adults of United States: National Health and Nutrition Examination Survey 2007–2016. Hong Kong Med J. 2020; 26(Suppl 1):13.
34. Ludwig DS. The glycemic index: physiological mechanisms relating to obesity, diabetes, and cardiovascular disease. JAMA. 2002; 287:2414–2423. PMID:
11988062.
35. Chan HM, Brand-Miller JC, Holt SH, Wilson D, Rozman M, Petocz P. The glycaemic index values of Vietnamese foods. Eur J Clin Nutr. 2001; 55:1076–1083. PMID:
11781674.

36. Cheung BM. The cardiovascular continuum in Asia--a new paradigm for the metabolic syndrome. J Cardiovasc Pharmacol. 2005; 46:125–129. PMID:
16044022.

37. National Heart, Lung, and Blood Institute (US). The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Bethesda (MD): National Heart, Lung, and Blood Institute;2004.
38. Vest AR, Heneghan HM, Agarwal S, Schauer PR, Young JB. Bariatric surgery and cardiovascular outcomes: a systematic review. Heart. 2012; 98:1763–1777. PMID:
23077152.

39. Sharma AM, Golay A. Effect of orlistat-induced weight loss on blood pressure and heart rate in obese patients with hypertension. J Hypertens. 2002; 20:1873–1878. PMID:
12195131.

40. Wang B, Zhong J, Lin H, et al. Blood pressure-lowering effects of GLP-1 receptor agonists exenatide and liraglutide: a meta-analysis of clinical trials. Diabetes Obes Metab. 2013; 15:737–749. PMID:
23433305.

41. Georgianos PI, Agarwal R. Ambulatory blood pressure reduction with SGLT-2 inhibitors: dose-response meta-analysis and comparative evaluation with low-dose hydrochlorothiazide. Diabetes Care. 2019; 42:693–700. PMID:
30894383.

42. Fei Y, Tsoi MF, Cheung BMY. Cardiovascular outcomes in trials of new antidiabetic drug classes: a network meta-analysis. Cardiovasc Diabetol. 2019; 18:112. PMID:
31462224.





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download