1. Period prior to the introduction of measles vaccine
Prior to the introduction of measles vaccines, measles in children was the most common infectious disease in Korea. Although there are no exact national statistics available, experts have reported that approximately one million children, representing close to 20% of entire Korean child population, were infected with this disease, usually between May and July, up to mid-1960s until the introduction of measles vaccines. Among those infected, approximately 20,000 children lost their lives to this disease [
1]. With such high numbers, measles was recognized as the most severe infectious disease with the highest morbidity and mortality rates. This period was also marked by complications due to various improper folk remedies (including crayfish juice and liquor), which further caused sequelae and mortality. Several media reports have confirmed that infectious disease experts at the time actively recommended hospitalization for patients who experienced persistent fever, breathing difficulties, or altered state of consciousness, while also emphasizing that intramuscular injection of gamma globulin could prevent measles and mitigate any symptoms in those who come in contact with a measles-infected patient [
2]. In addition, they recommended good personal hygiene, along with the need for sufficient hydration and intake of protein-based foods that are easy to digest.
2. Period prior to measles catch-up vaccinations
An inactivated and a live attenuated vaccine (Edmonston B strain) became commercially available as the first measles vaccines. However, the inactivated vaccine provided a short duration of sustained immunity and many people developed atypical measles after being vaccinated. Consequently, the use of this vaccine was discontinued in 1967. The live attenuated vaccine showed high seroconversion rate after vaccination. However, the use of this vaccine was also discontinued in 1975 due to the high frequency of fever and rash. In addition, the Schwarz strain vaccine, produced by further attenuation of the Edmonston A strain, has been used since 1965 while the Edmonston-Enders strain vaccine, produced by further attenuation of the Edmonston B strain, has been used since 1968.
Starting in 1965, live attenuated measles vaccines (Schwarz strain) were introduced and used in Korea under the brand names Lilugen
® and Rubio Box
®. Initially, the cost for vaccination was 1,500 won. This was very expensive at the time and made it difficult to vaccinate the poor. However, a free vaccination program for children from 9 months to 4 years old belonging to the extreme poverty group was implemented in March 1970 while the regular vaccination rate also increased steadily, leading to an appreciable decrease in the number of measles patients [
3].
Previously, children were vaccinated once with a measles vaccine between the ages of 6 months and 1 year. Vaccination at the age of 12 months was recommended and a single vaccination was believed to provide a lifetime of protection against measles. However, with the gradually increasing number of patients who developed measles even after measles immunization, issues concerning the improper management of measles vaccines (problems suspected to have been caused by non-compliance with the instruction to store the vaccines at low temperature) and the duration of protection from measles after vaccination began to emerge in 1978 [
4]. During the 1990s, it became known worldwide that long-lasting protection could be achieved through two rounds of vaccination. Consequently, Korea began recommending one vaccination at the age of 12 – 15 months and another vaccination at the age of 4 – 6 years.
Despite such efforts, the low measles immunization rate led to outbreaks of measles in 4-to-6-year cycles, which is the duration for people susceptible to measles to be accumulated to an epidemic level. As a result of this pattern of outbreak, an average of 4,000 – 6,000 new measles cases per year was reported until the early 1980s. However, the average number of new measles cases has decreased to 1,000 – 2,000 new cases per year owing to the immunization programs in the private sector and the free national immunization program implemented by the government in 1985 [
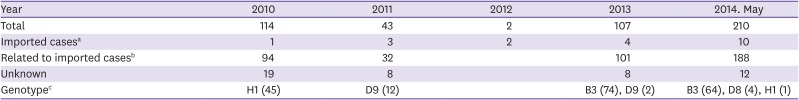
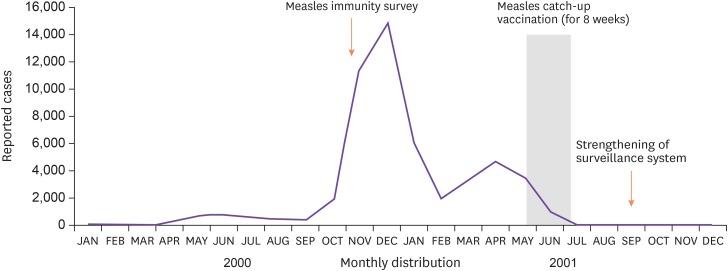
5]. However, during the global measles pandemic in 1989 and 1990, 2,394 and 3,415 cases, respectively, were reported. During the nationwide measles epidemic that occurred in Korea from 1993 to 1994, the incidence of measles among children who were 6 years or older was higher than the incidence reported between 1989 and 1990. Accordingly, in 1994, the Korean Pediatric Society temporarily recommended an additional secondary measles, mumps, and rubella (MMR) vaccination at the age of 6 years, in addition to the standard primary MMR vaccination at the age of 15 months. As a result, the vaccination schedule was adjusted after 1997. The age for primary MMR vaccination was changed to 12 – 15 months and that for secondary vaccination was changed to 4 – 6 years. Subsequently, the incidence of measles dropped to less than 100 cases per year. However, a major pandemic occurred during 2000 – 2001 with 52,897 reported cases and 7 mortalities (
Table 1 and
Fig. 1) [
6].
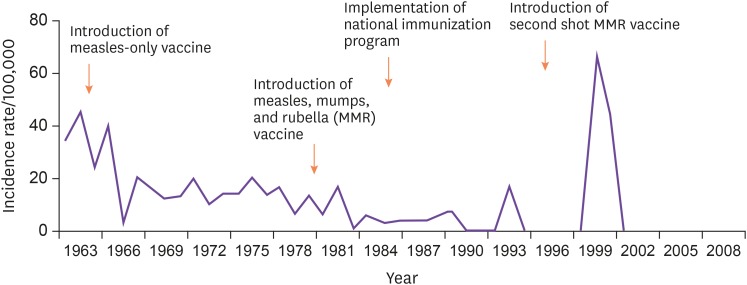 | Figure 1Incidence of measles by year in South Korea (1963 – 2010).
|
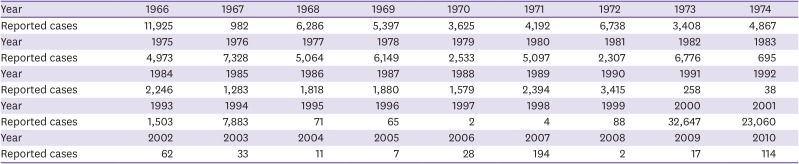
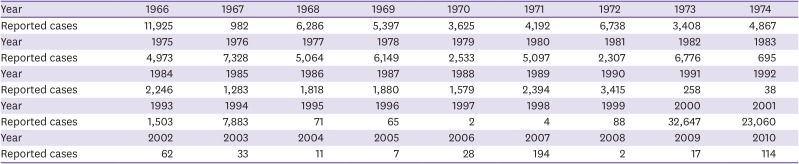
Table 1
Reported measles cases by year in Korea (1966 – 2010) unit: cases
|
Year |
1966 |
1967 |
1968 |
1969 |
1970 |
1971 |
1972 |
1973 |
1974 |
|
Reported cases |
11,925 |
982 |
6,286 |
5,397 |
3,625 |
4,192 |
6,738 |
3,408 |
4,867 |
|
Year |
1975 |
1976 |
1977 |
1978 |
1979 |
1980 |
1981 |
1982 |
1983 |
|
Reported cases |
4,973 |
7,328 |
5,064 |
6,149 |
2,533 |
5,097 |
2,307 |
6,776 |
695 |
|
Year |
1984 |
1985 |
1986 |
1987 |
1988 |
1989 |
1990 |
1991 |
1992 |
|
Reported cases |
2,246 |
1,283 |
1,818 |
1,880 |
1,579 |
2,394 |
3,415 |
258 |
38 |
|
Year |
1993 |
1994 |
1995 |
1996 |
1997 |
1998 |
1999 |
2000 |
2001 |
|
Reported cases |
1,503 |
7,883 |
71 |
65 |
2 |
4 |
88 |
32,647 |
23,060 |
|
Year |
2002 |
2003 |
2004 |
2005 |
2006 |
2007 |
2008 |
2009 |
2010 |
|
Reported cases |
62 |
33 |
11 |
7 |
28 |
194 |
2 |
17 |
114 |

According to the measles outbreak survey in 2000, the distribution pattern by age is as follows: high incidence among those who were <1 year old; decreased incidence among those who were 2 years and older; appreciably low incidence among those who were between the ages of 4 and 5 years; gradual increase among those who were more than 6 years old; and gradual decrease after reaching its peak level among those who were 10 years old. In the same survey, the basic MMR vaccination rate among children aged 1 – 3, 4 – 6, and 7 – 15 years was 34.9%, 72.1%, and 72.0 – 79.0%, respectively. Among children who were 3 years or older, measles occurred mostly in those who had been vaccinated. However, for those between the ages of 4 and 6 years, the actual MMR vaccination rate was very low (19.4%).
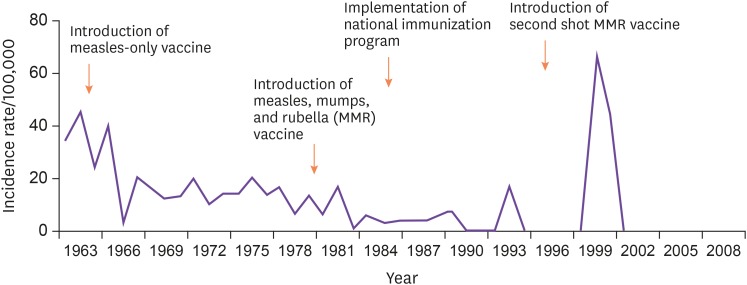
To eradicate these pandemics, the Ministry of Health and Welfare developed the National Measles Elimination 5 Year Program and established strong policies to maintain vaccination rate at ≥ 95% to expedite the eradication and elimination of measles outbreaks before 2005 [
7]. The policy strategy included the following: first, a nationwide survey of measles immunity was conducted to determine the measles susceptibility level; and second, a secondary measles vaccination history confirmation program before admitting primary school was established to increase the secondary measles vaccination rate among pre-school aged children. Based on the distribution of measles patients by age during the 2000 – 2001 outbreak and the results from the measles immunity survey which involved 18,139 children aged between 7 and 18 years, a catch-up vaccination program for one-time immunization with the measles and rubella (MR) vaccine was conducted between May 21 and June 30, 2001, which involved 5,849,816 children aged between 8 and 16 years (
Fig. 2). As a result, 97.1% of the target population was vaccinated [
8].
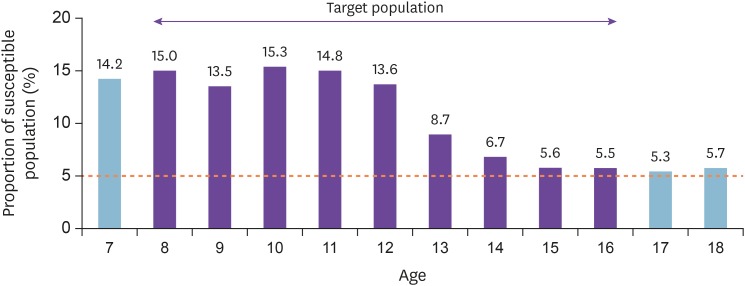 | Figure 2Proportion of susceptible population and target population of catch-up vaccination by age.
|
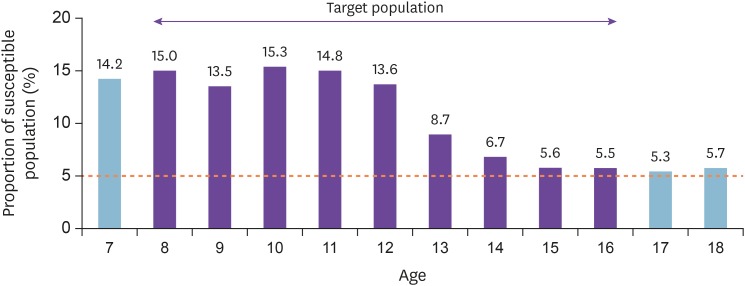
There was a significant public backlash concerning the catch-up vaccination during its implementation and several challenges, especially after adverse reactions among large groups of people following the vaccination [
9]. Specifically, middle and high school-aged girls showed adverse reactions after MR catch-up vaccination. However, such adverse reactions were identified as serial reactions due to group vaccinations unrelated to the immunization vaccine. With the exceptions of death, which occurred in one case, and acute disseminated encephalomyelitis, which occurred in another case, there were no other serious adverse reactions, and only mild symptoms which occurred transiently after the vaccination, including fever, headache, and rash, were found. The number of measles patients decreased drastically after the measles catch-up vaccination (
Fig. 3). During this time, the Korean government notified the North Korean delegation for family reunion to vaccinate their citizens against measles before visiting Korea, as a preventive measure against measles outbreak. This indicates the extent to which measles was considered a sensitive social issue at the time [
10]. To eradicate measles by 2005, the Korean government conducted annual secondary measles vaccination confirmation projects for children who were entering primary school. This resulted in the implementation of the law which required the mandatory submission of vaccination records when entering primary school, starting from 2005, to maintain the secondary MMR vaccination rate at ≥ 95%.
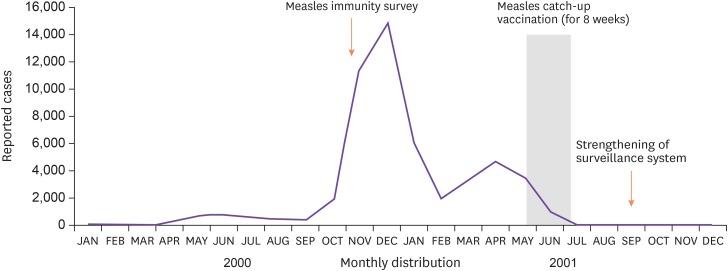 | Figure 32000-2001 measles pandemic and changes after catch-up vaccination.
|
3. Period after the national measles catch-up vaccination
In order to maintain the secondary measles vaccination rate at ≥95% after the national measles catch-up vaccination program, the measles vaccination confirmation project for all pre-primary school-aged children in March 2001, and as a result, the vaccination rate for two rounds of measles vaccinations was maintained at 95 – 99% in all 7-year-old children before they entered primary school. In order to eliminate measles, the measles surveillance system was strengthened starting from 2003 to eradicate indigenous outbreaks. Clinical samples were also collected from patients suspected of having measles to enable accurate diagnosis and active investigation. As a result, Korea was able to satisfy all the criteria for the Declaration of Measles Elimination by the World Health Organization (WHO) from 2002 to 2006 [
11]. During this period, the number of confirmed measles patients per one million people was below 1 (excluding imported cases) annually. Additionally, all measles patients and routes of transmission were actively investigated and reported.
Moreover, by maintaining the rate of vaccination with 2 rounds of measles-containing vaccine at ≥95%, the vaccination rates in all regions were maintained at ≥95%. Even outbreaks involving imported cases were small-scale outbreaks that were eventually eliminated. A small outbreak occurred in 2006 and another one in 2007. The outbreak in 2006 involved 15 children from a single kindergarten in Incheon. The genotype of the virus detected in the confirmed patients was identified as H1. The outbreak in 2007 involved in-hospital infection mostly among unvaccinated infants (0 - 1-year-old) in the Seoul and Geyongin areas. Among all the confirmed measles patients from 6 hospitals, 81 patients were confirmed to have been infected by in-hospital transmission. Among them, 76 patients were hospitalized during the same period as measles patients; two patients were family members of hospitalized patients, who were suspected to have been infected while visiting the hospital; and 3 patients were medical professionals. In 2007, the number of measles patients was 194. Subsequently, the number of measles patients in 2008, 2009, and 2010 was 2, 17, and 114, respectively [
12]. In 2009, there was no outbreak, but measles occurred sporadically in 17 patients (6 suspected cases). In 2010, there was an outbreak in one schools in the Incheon area, affecting 114 patients (3 suspected cases). In 2011, small outbreaks occurred mostly in the Gyeongsangnam-do region, where a total of 42 patients out of 287 suspected of having measles were confirmed to have measles. There were 3 imported cases (2 from the Philippines and 1 from Thailand). In 2012, a total of 125 cases were reported through the passive measles surveillance system and 2 cases were reported through the active measles surveillance system. There were 2 cases with confirmed diagnosis based on laboratory test results and the case classification criteria of the regional office for the Western Pacific (WPRO) of the WHO, and both cases were imported cases. In 2013, a total of 107 patients in the Gyeongsangnam-do and Gyeonggi regions were confirmed to have measles. These patients were infected either at the hospital, at school, in their community, or by family members. In 2014, imported cases caused secondary transmission in Korea, mostly through hospitals. The outbreak affected 442 patients, including children with a weak immune system and unvaccinated adolescents and college students in group-living conditions. This resulted in a 4-fold increase as compared to the previous year. Among the 421 domestic cases reported, the highest number of cases was reported in the Gyeonggi region (n = 141), followed by Seoul (n = 94), Incheon (n = 52), and Jeollanam-do (n = 44). In terms of age, it was most common among those < 10 years of age (n = 191, 43.2%), followed by those between the ages of 10 and 19 years (n = 142, 32.1%). It was also more common among males (n = 261) than females (n = 181) [
13]. Since 2006, the genotypes of measles viruses identified in Korea were mostly B3, D5, D8, D9, and H1. As shown, Korea has continued to face the need to maintain its surveillance system in preparation for possible re-outbreaks. Additionally, Korea has continued to manage imported cases; manage transmission within schools, kindergartens, and medical institutions; and educate local response personnel, including epidemiological investigation teams. Based on its efforts, Korea was re-verified with a measles elimination status by the WHO WPRO in March 2014. However, sporadic outbreaks of measles have repeatedly occurred even after the declaration of measles elimination. This indicates the need for continued control of imported cases and possible re-outbreaks.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download