A middle-aged man presented with dyspnea for 1 month. His medical history included familial hypertrophic cardiomyopathy and implantable cardioverter-defibrillator implantation for sinus bradycardia and advanced atrioventricular (AV) block and to prevent sudden cardiac death. DDD pacing was set to 60 bpm with postventricular atrial refractory period (PVARP) of 350 ms. Prolonged AV delay of 350 ms was needed because of severe atrial conduction delay. Physical examination showed signs of heart failure—peripheral edema and S3 gallop. Echocardiography showed reduced left ventricular systolic function; however, transmitral flow was not of restrictive pattern (Figure 1A). Atrial contraction due to ventriculoatrial (VA) conduction during systole was suspected based on the pulmonary venous (PV) flow and verified on intracardiac electrocardiogram (Figure 1B, C). We thought that heart failure was caused by masked systolic atrial contraction. An accessory pathway, which was elucidated electrophysiologically via an implantable cardioverter-defibrillator, caused VA conduction (Figure 2A, B). The patient refused curative abolition of the pathway. VA conduction disappeared in an AV delay of 150 ms, but diastolic atrial contraction also disappeared (Figure 3A) and delayed systolic atrial contraction appeared by the PV flow (Figure 3B). The AV delay of 280 ms caused preserved diastolic atrial contraction without VA conduction (Figure 4). Follow-up after 1 year showed resolution of heart failure symptoms.
VA conduction can be managed electrophysiologically by PVARP prolongation; however, atrial contraction during systole affects hemodynamics.1) PV flow using echocardiography could detect VA conduction. Thus, besides electrophysiological monitoring, we recommend echocardiographic resolution to treat heart failure with ventricular pacing and VA conduction.
References
1. Tabata T, Grimm RA, Bauer FJ, et al. Giant flow reversal in pulmonary venous flow as a possible mechanism for asynchronous pacing-induced heart failure. J Am Soc Echocardiogr. 2005; 18:722–728. PMID: 16003269.
Figure 1
Echocardiography and intracardiac electrocardiography during atrioventricular delay of 350 ms. (A) The patient exhibited heart failure symptoms; however, transmitral flow was not a restrictive pattern. (B) By pulmonary venous flow, systolic reversal flow (arrow) due to ventriculoatrial conduction is noted. (C) Constant ventriculoatrial conduction (arrow) is shown using intracardiac electrocardiography. AR represents successfully masked ventriculoatrial conduction by prolonged postventricular atrial refractory period. Ab: atrial blanking period, AP: atrial pacing, AR: atrial refractory period, ICD: implantable cardioverter-defibrillator, ICE: intracardiac electrocardiogram, VP: ventricular pacing, VS: ventricular sensing.
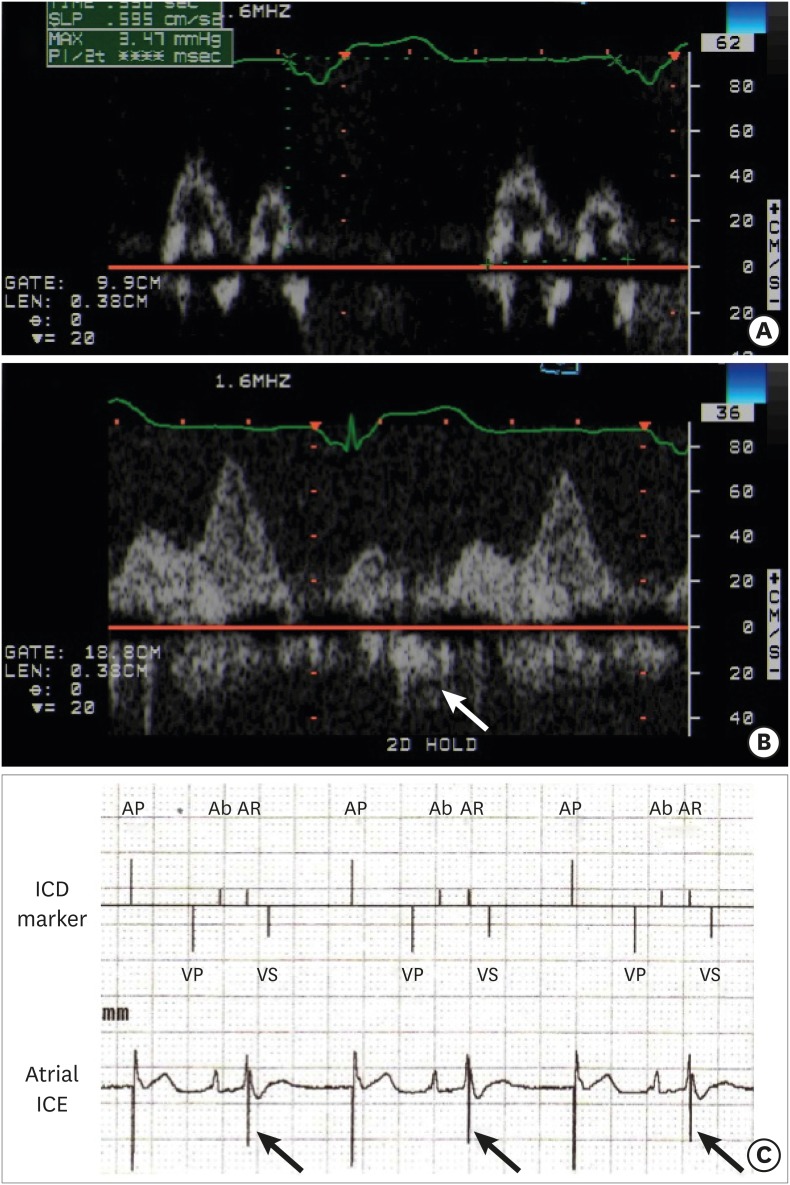
Figure 2
Electrophysiological study via ICD. (A) Ventricular pacing of 100 bpm demonstrated constant VA conduction. (B) Ventricular pacing of 120 bpm demonstrated refractory period of VA conduction. No decrement represented VA conduction via accessory pathway. AS: atrial sensing, ICD: implantable cardioverter-defibrillator, TP: tachypacing, VA: ventriculoatrial.
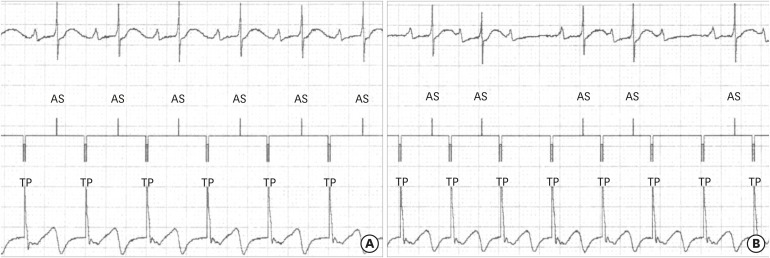
Figure 3
Echocardiography during atrioventricular delay of 150 ms. (A) Atrial contraction disappeared by transmitral flow. (B) By pulmonary venous flow, systolic reversal flow (arrow) due to delayed atrial conduction is noted.
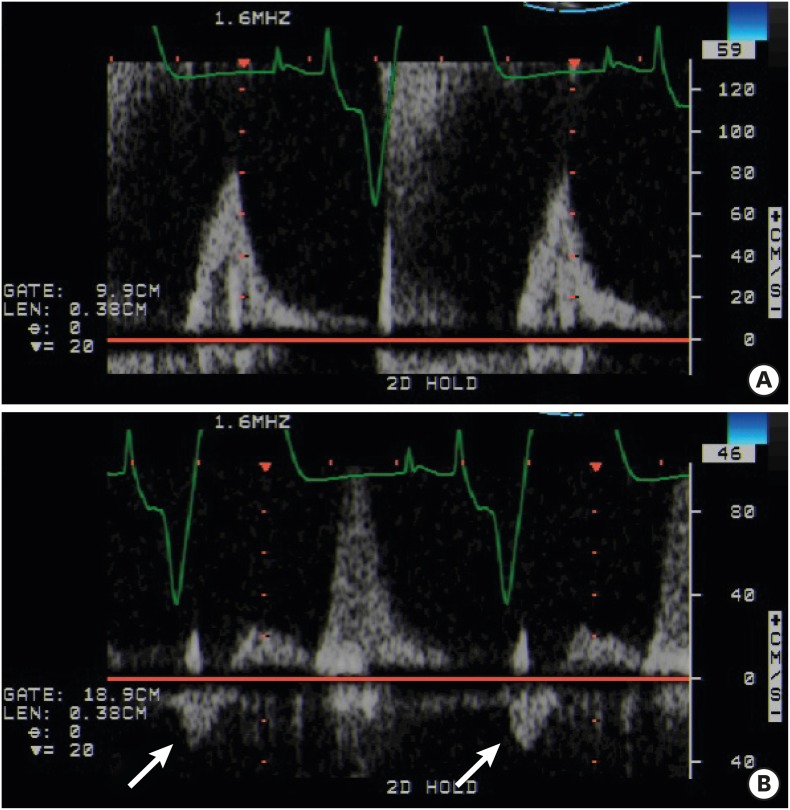
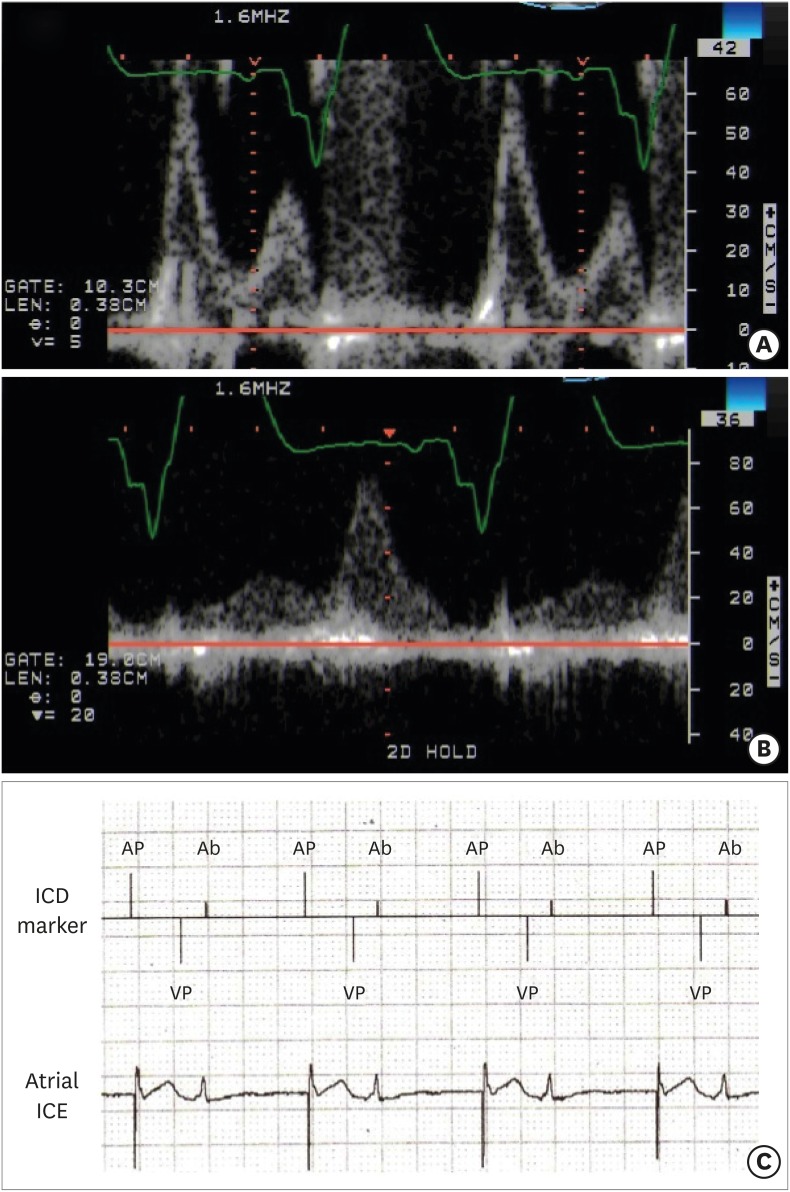
Figure 4
Echocardiography and intracardiac electrocardiography during atrioventricular delay of 280 ms. (A) Atrial contraction appeared by transmitral flow. (B) By pulmonary venous flow, systolic reversal flow disappeared. (C) No constant ventriculoatrial conduction is detected using intracardiac electrocardiography. Atrial sensing during atrial blanking is detected due to far-field potential of ventricular pacing. Ab: atrial blanking period, AP: atrial pacing, ICD: implantable cardioverter-defibrillator, ICE: intracardiac electrocardiogram, VP: ventricular pacing.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download