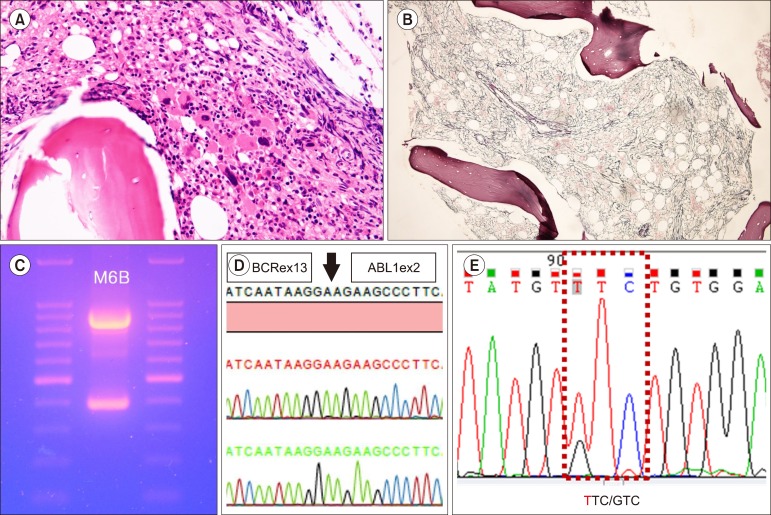
 | Fig. 1Bone marrow biopsy showing (A) hypercellular marrow with increased megakaryocytes and atypia (H&E stain, ×400) and (B) myelofibrosis grade MF-2 demonstrated by reticulin staining (reticulin stain, ×200). Reverse transcriptase (RT)-PCR analysis of BCR-ABL1 translocation using a HemaVision kit showing a single 397 bp band in the M6B split out PCR, indicating a fusion transcript with BCR-ABL1 (C). Sequencing analysis of the RT-PCR product showing breakpoint located at exon 13 in the BCR gene and exon 2 in the ABL gene (D). Sequencing analysis of JAK2V617F showing a heterozygous JAK2V617F mutation (E). |
TO THE EDITOR: It is well known that BCR-ABL1 translocations and JAK2V617F mutations are mutually exclusive events in myeloproliferative neoplasms (MPN) [1]. However, the coexistence of both abnormalities has been reported in several cases [123456]. Until now, two studies have reported the co-occurrence of BCR-ABL1 translocation and JAK2V617F mutation in Korea [34]. Here, we discuss the clinical significance through a literature review, especially focusing on cases reported in Korea with a case presentation.
A 68-year-old woman was admitted with increased hemoglobin (Hb) and leukocyte count. Complete blood count (CBC) at admission showed the following: white blood cells, 17.06×109/L; Hb, 17.3 g/dL; and platelets, 245×109/L. Peripheral blood smear demonstrated leukoerythroblastosis with the presence of few tear drop cells. Differential counts of leukocytes were as follows: myelocytes 1%, metamyelocytes 1%, neutrophil 84%, lymphocytes 9%, monocytes 4%, eosinophil 1%, and rare nucleated red blood cells. Her serum lactate dehydrogenase level was elevated (313 IU/L, reference range, 0–250 IU/L) while her serum erythropoietin level was decreased (3.06 mIU/L, reference range, 3.7–37.5 mIU/L). An abdominopelvic computed tomography showed splenomegaly. We could not acquire sufficient information from the bone marrow aspirate, because it was diluted. However, bone marrow biopsy revealed hypercellularity and a slightly increased number of megakaryocytes (3.4/high power field) with dense clustering and certain degree of atypia (Fig. 1). Diffuse myelofibrosis, with bone marrow fibrosis (MF) grade 2, was detected (Fig. 1). Reverse-transcriptase PCR (RT-PCR) assay for the BCR-ABL1 fusion transcript showed the presence of a major BCR-ABL1 fusion transcript (b13a2 type), which was confirmed by sequencing (Fig. 1). The fusion transcript level was 1.23% on the international scale (IS). An allele-specific PCR assay for the JAK2V617F mutation was positive for a heterozygous type JAK2V617F mutation with an allelic burden of 79.20%, which was confirmed by sequencing (Fig. 1). The chromosomal analysis revealed 46,XX karyotype[20]. Interphase fluorescent in situ hybridization for BCR-ABL1 translocation was nuc ish (ABL1, BCR)×2 (ABL1 con BCR×1) [13/500], representing a normal result (below the cutoff level). The final diagnosis revealed MPN, with concurrent JAK2V617F mutation and major BCR-ABL1 translocation. The patient was only treated with hydroxyurea (500 mg, twice a day). After 10 months of treatment, her CBC became normal (5.35×109/L white blood cells, a Hb of 14.9 g/dL, and 185×109/L platelets) and BCR-ABL1 transcripts level was 0.016% IS.
Detecting BCR-ABL1 translocation and JAK2V617F mutation simultaneously at the time of diagnosis is a rare event. Recent studies have reported that about 0.2–0.5% of MPN patients are positive for both BCR-ABL1 and JAK2V617F [67]. It has been suggested that most MPN cases with concurrent BCR-ABL1 and JAK2V617F consist of two unrelated clones [268].
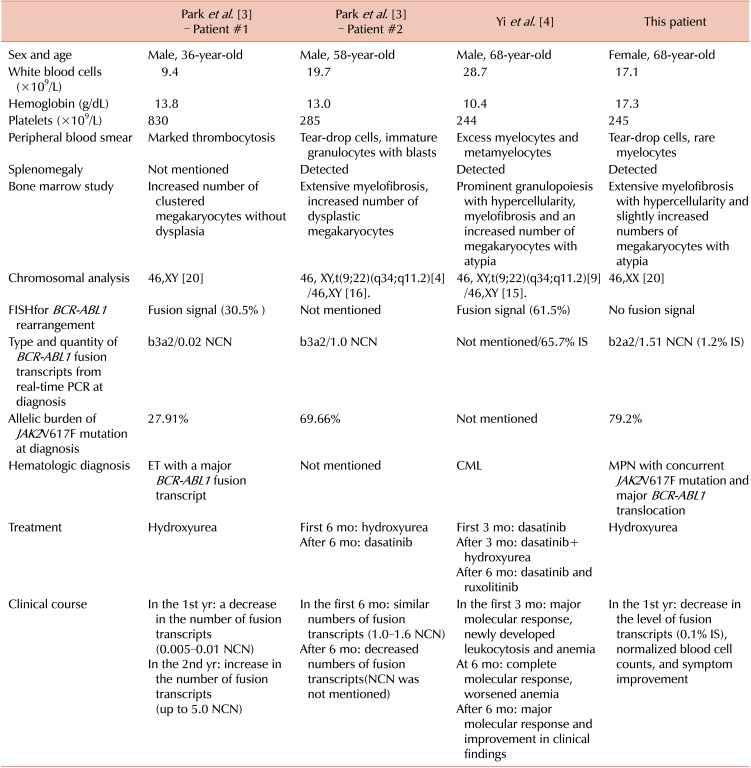
The coexistence of these abnormalities may affect laboratory findings and patient diagnosis. Park et al. [3] reported two cases of MPN, with a relative JAK2V617F dominancy over BCR-ABL1 transcripts. Their laboratory findings resembled essential thrombocythemia (ET) and primary myelofibrosis (PMF). Our patient showed a relative dominancy of JAK2V617F, with the laboratory diagnosis resembling PMF. In contrast, the case reported by Yi and Kim [4] showed relatively high levels of BCR-ABL1 transcripts. Laboratory features of both CML and PMF were detected (Table 1). Soderquist et al. [8] have reported that coexistence cases show mixed megakaryocytes characteristics that include both dwarf megakaryocytes, seen in CML, and bulbous megakaryocytes, seen in PMF. Therefore, it is essential to perform tests for BCR-ABL1 and JAK2V617F simultaneously with quantitation, in order to avoid misinterpretation and obtain an accurate diagnosis of MPN.
The molecular abnormality profile can influence the choice of treatment modalities. Cases reported by Park et al. [3] and our patient showed acceptable responses to hydroxyurea. However, the case reported by Yi and Kim [4] showed treatment responses to dasatinib (a tyrosine kinase inhibitor), hydroxyurea, and ruxolitinib (a JAK1/2 tyrosine kinase inhibitor) (Table 1). Other studies [69] have reported successful responses to the simultaneous use of tyrosine kinase inhibitors and hydroxyurea or ruxolitinib in patients with concomitant BCR-ABL1 and JAK2V617F. Therefore, detection of molecular abnormalities is important for appropriate treatment, especially when a decision must be made in the event of therapeutic failure and drug replacement.
Another issue is the impact of molecular abnormalities on patient outcomes. Soderquist et al. [8] have reported that seven of 11 MPN patients with concurrent BCR-ABL1 and JAK2V617F showed progression to myelofibrosis, suggesting that these patients are more prone to disease progression. The coexistence of two molecular abnormalities might accelerate the progression. Nevertheless, cases reported in Korea have shown successful responses without death, at the time of publication [34]. However, data concerning the progression rate and survival of patients with concomitant BCR-ABL1 and JAK2V617F mutations are currently insufficient.
In summary, it is important to recognize the possibility of the coexistence of a BCR-ABL1 translocation and JAK2V617F mutation in MPN, because they can affect hematologic features and treatment strategy. However, it is unclear if MPNs with concomitant BCR-ABL1 translocations and JAK2V617F mutations reflect a novel clinical entity with distinct features and outcomes. Further investigation with a large cohort is needed.
Notes
Authors' Disclosures of Potential Conflicts of Interest: No potential conflicts of interest relevant to this article were reported.
Go to : 
References
1. Xiao X, Zhang Y, Zhang GS, Zheng WL, Xiao L, Liu SF. Coexistence of JAK2V617F mutation and BCR-ABL1 transcript in two Chinese patients with chronic myelogenous leukemia. Acta Haematol. 2012; 127:47–49. PMID: 22025110.
2. Martin-Cabrera P, Haferlach C, Kern W, Schnittger S, Haferlach T. BCR-ABL1-positive and JAK2 V617F-positive clones in 23 patients with both aberrations reveal biologic and clinical importance. Br J Haematol. 2017; 176:135–139. PMID: 26847954.
3. Park SH, Chi HS, Cho YU, et al. Two cases of myeloproliferative neoplasm with a concurrent JAK2 (V617F) mutation and BCR/ABL translocation without chronic myelogenous leukemia phenotype acquisition during hydroxyurea treatment. Ann Lab Med. 2013; 33:229–232. PMID: 23667855.
4. Yi JH, Kim HR. Coexistence of BCR/ABL1-positive chronic myeloid leukemia and JAK2 V617F-mutated myelofibrosis successfully treated with dasatinib and ruxolitinib. Blood Res. 2019; 54:77–79. PMID: 30956968.

5. Bader G, Dreiling B. Concurrent JAK2-positive myeloproliferative disorder and chronic myelogenous leukemia: a novel entity? A case report with review of the literature. J Investig Med High Impact Case Rep. 2019; 7:2324709619832322.

6. Lewandowski K, Gniot M, Wojtaszewska M, et al. Coexistence of JAK2 or CALR mutation is a rare but clinically important event in chronic myeloid leukemia patients treated with tyrosine kinase inhibitors. Int J Lab Hematol. 2018; 40:366–371. PMID: 29508552.
7. Agarwal R, Blombery P, McBean M, et al. Clinicopathological differences exist between CALR- and JAK2-mutated myeloproliferative neoplasms despite a similar molecular landscape: data from targeted next-generation sequencing in the diagnostic laboratory. Ann Hematol. 2017; 96:725–732. PMID: 28161773.

8. Soderquist CR, Ewalt MD, Czuchlewski DR, et al. Myeloproliferative neoplasms with concurrent BCR-ABL1 translocation and JAK2 V617F mutation: a multi-institutional study from the bone marrow pathology group. Mod Pathol. 2018; 31:690–704. PMID: 29327708.

9. Zhou A, Knoche EM, Engle EK, Fisher DA, Oh ST. Concomitant JAK2 V617F-positive polycythemia vera and BCR-ABL-positive chronic myelogenous leukemia treated with ruxolitinib and dasatinib. Blood Cancer J. 2015; 5:e351. PMID: 26430722.

Go to : 




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download