Dear Editor,
Ocular hypotony is a rare complication of cataract surgery. We encountered a case of transient hypotony and subsequent intraocular pressure (IOP) elevation after uneventful phacoemulsification and intraocular lens implantation in an eye with prior trabeculectomy. In this report, we describe the clinical findings of the case and discuss a possible mechanism for ocular hypotony.
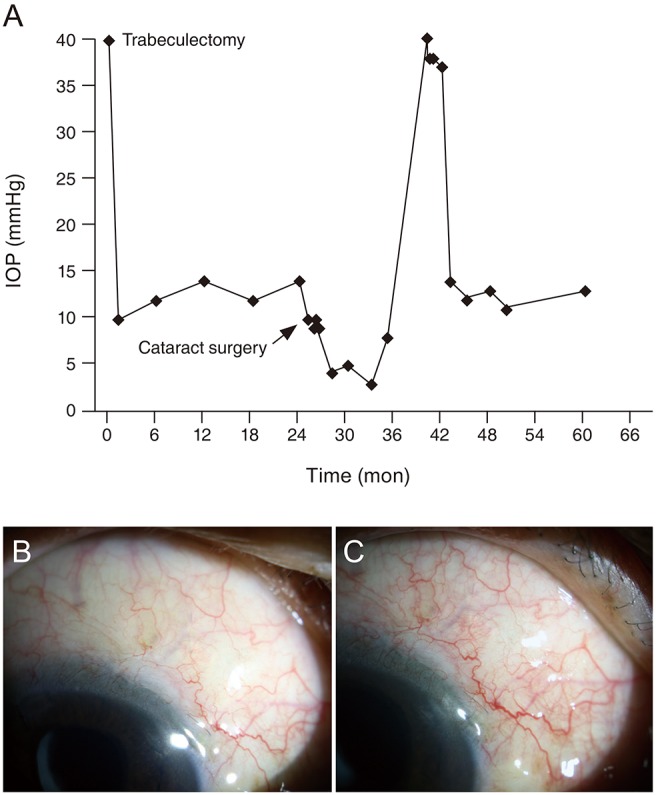
A 63-year-old man underwent trabeculectomy with 0.4 mg/mL of mitomycin C (MMC) for uncontrolled IOP (above 40 mmHg with three eye drops to lower IOP) due to neovascular glaucoma accompanied by proliferative diabetic retinopathy. After the trabeculectomy, his IOP ranged from 10 to 14 mmHg with one eye drop to lower IOP (fixed combination of dorzolamide/timolol). At that time, his best-corrected visual acuity was hand motion because of severe visual field defect and diabetic retinopathy. Two years after the trabeculectomy, the patient underwent uneventful phacoemulsification and intraocular lens implantation with a clear corneal incision. A topical eye drop containing 0.1% fluorometholone and a fluoroquinolone antibacterial eye drop were administered 4 times daily for one postoperative month. An eye drop to lower the IOP was continuously administered after the cataract surgery. Between postoperative day 1 and the following 2 months, the IOP ranged from 9 to 10 mmHg. Three months after the operation, the IOP decreased to 4 mmHg (Fig. 1A). Ophthalmic examination revealed mild corneal edema and mild inflammation (1+ cells) in the anterior chamber. Choroidal detachment was found on fundus examination and B-scan ultrasonography. There were no changes in a pre-existing filtering bleb appearance (Fig. 1B, 1C). On gonioscopy and ultrasound biomicroscopy, cyclodialysis cleft was not found. The eye drop to lower IOP was discontinued, and topical 0.1% fluorometholone was administered four times daily. Nevertheless, the IOP ranged from 4 to 6 mmHg. Seven months after the onset of ocular hypotony, the IOP spontaneously increased to 8 mmHg and then further increased to 40 mmHg 2 months thereafter. The patient's elevated IOP could not be controlled, despite the use of three eye drops, so an Ahmed glaucoma valve (New World Medical, Rancho Cucamonga, CA, USA) was implanted. After an Ahmed glaucoma valve implantation, the IOP ranged from 12 to 14 mmHg with one eye drop to lower the IOP for 2 years, and the best-corrected visual acuity remained hand motion.
Previous studies reported surgical wound leak, occult cyclodialysis cleft, and persistent inflammation as possible causes of hypotony after cataract surgery [12]. In the present case, surgical wound leakage or cyclodialysis cleft were not found. Although a small cyclodialysis cleft might be missed on gonioscopy and ultrasound biomicroscopy, wound leakage or cyclodialysis cleft could not have been the chief cause of hypotony in this case because hypotony occurred 3 months after surgery. The eye had filtering blebs, so excessive aqueous drainage through the bleb might have happened after the cataract surgery. However, this mechanism could only explain hypotony in the early postoperative period.
Another possible cause of hypotony is ocular inflammation after cataract surgery. The case showed mild inflammation at the onset of hypotony. Persisting subclinical inflammation induced by cataract surgery might have caused hypotony by either decreasing aqueous humor production or increasing uveoscleral outflow, as seen in eyes with uveitis [3]. In this case, it is not clear why inflammation was found 3 months after cataract surgery and whether it was the cause of ocular hypotony.
It has been reported that the use of aqueous suppressants, such as dorzolamide [4], and application of MMC during trabeculectomy may affect the ability of the ciliary body to produce aqueous humor. In the present study, a fixed combination of dorzolamide/timolol eye drops was used before the onset of ocular hypotony and MMC was applied during the trabeculectomy. Therefore, these may have acted as causes or aggravating factors of ocular hypotony.
Notably, after the improvement of hypotony, the IOP was substantially elevated compared to the preoperative IOP level. Decreased aqueous flow in the bleb and increased inflammatory mediators in the aqueous humor during the hypotony were the likely causes of subconjunctival scarring and subsequent failure [5].
To the best of our knowledge, this is the first report of transient ocular hypotony with subsequent elevation of IOP after cataract surgery in an eye with prior trabeculectomy. When hypotony occurs, the function of the filtering bleb might decrease, which might lead to substantial elevation in IOP after the recovery of hypotony. Close observation is needed to prevent the progression of glaucoma by sudden substantial IOP elevation.
References
1. Schubert HD. Postsurgical hypotony: relationship to fistulization, inflammation, chorioretinal lesions, and the vitreous. Surv Ophthalmol. 1996; 41:97–125. PMID: 8890437.

2. Mushtaq B, Chiang MY, Kumar V, et al. Phacoemulsification, persistent hypotony, and cyclodialysis clefts. J Cataract Refract Surg. 2005; 31:1428–1432. PMID: 16105618.

3. Sen HN, Drye LT, Goldstein DA, et al. Hypotony in patients with uveitis: the Multicenter Uveitis Steroid Treatment (MUST) trial. Ocul Immunol Inflamm. 2012; 20:104–112. PMID: 22409563.

4. Sharma T, Salmon JF. Hypotony and choroidal detachment as a complication of topical combined timolol and dorzolamide. J Ocul Pharmacol Ther. 2007; 23:202–205. PMID: 17444809.

5. Khaw PT, Chang L, Wong TT, et al. Modulation of wound healing after glaucoma surgery. Curr Opin Ophthalmol. 2001; 12:143–148. PMID: 11224722.

Fig. 1
(A) Changes in intraocular pressure (IOP) and filtering bleb appearance (B) 3 months before and (C) 5 months after cataract surgery. Ocular hypotony developed 3 months after the cataract surgery and improved after 7 months. However, the IOP was still substantially increased, and additional glaucoma surgery was needed to control the patient's elevated IOP.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download