Abstract
Purpose
To evaluate the clinical features and prognosis of a delayed-onset consecutive esotropia (ET) after surgical correction of intermittent exotropia.
Methods
Thirty-four patients who developed consecutive ET after primary bilateral lateral rectus recession for the surgical correction of intermittent exotropia were evaluated retrospectively and were divided into two groups: delayed-onset consecutive ET group and the continuous consecutive ET group. Patients who developed esodeviation after once recovering to orthotropia within 1 month after the operation were included in the delayed-onset consecutive ET group, and patients with continuous esodeviation after the operation were included in the continuous consecutive ET group. We evaluated preoperative and postoperative angle of deviation, suppression, stereopsis, and follow up periods between the two groups and compared re-operation and success following non-surgical treatment between the continuous consecutive ET group and the delayed-onset consecutive ET group.
Results
Among 34 patients with consecutive ET, 27 patients (79.4%) were included in the delayed-onset consecutive ET group, and seven patients (23.3%) were included in the continuous group. Success rate of non-surgical treatment was not statistically significant between two groups (p = 0.55), but it was higher in the delayed-onset group with 37.5%, and 25% of patients in continuous group were successfully recovered to straight alignment. Duration of orthotropia in delayed-onset group was 7.4 ± 6.0 months (range, 2–29 months). Age, sex, preoperative refractive error, preoperative exodeviation, suppression, and near steroacuity were not statistically significant between two groups (p > 0.05, all). In the delayed-onset group, three patients (11.1%) underwent re-operation, while three patients (42.9%) in continuous consecutive ET group underwent re-operation (p = 0.048).
Go to : 
Consecutive esotropia (ET) is a persisting or variable esodeviation after surgery to correct exotropia. The prevalence of such surgical overcorrection in patients with exodeviation ranges from 6% to 20% [12]. Risk factors for consecutive ET include lateral incomitancy [3], high accommodative convergence to accommodation ratio [45], age at surgery [6], and excessive lateral rectus muscle recession. As persisting consecutive ET may cause loss of binocular vision, diplopia, amblyopia, and suppression, several non-surgical treatments, such as optical correction, patching, and prism glasses, can be considered [7]. These conservative treatments of consecutive ET cases generally show a good clinical response [8]. If esodeviation of more than 10 prism diopters (PD) continues for more than six months, surgical management should be considered [7910].
Initial overcorrection is the target of surgical treatment of intermittent exotropia [11]. Comitant consecutive ET with small deviation usually improves spontaneously within one month, but even after recovering to orthotropia, there are some cases that develop esodeviation again. We defined reoccurring esodeviation as delayed-onset consecutive ET. Despite numerous studies that have investigated consecutive ET cases, delayed-onset consecutive ET has not been reported to our knowledge.
The purpose of this study was to evaluate the clinical features and prognosis of a delayed-onset consecutive ET case after surgical correction of intermittent exotropia.
The institutional review board of Korea University Medical Center approved this study (2019AN0176), and we adhered to the tenets of the Declaration of Helsinki. Written informed consent was waived due to the retrospective nature of the study.
A retrospective review was conducted of the clinical records of patients with angle of esodeviation greater than 4 PD at two weeks following bilateral lateral rectus (BLR) muscle recession for treatment of intermittent exotropia between September 2014 and February 2018. Patients with history of strabismus surgery, ocular trauma, neurologic deficits, and ocular disease other than anisometropia, amblyopia, and strabismus were excluded from the study.
Patients with consecutive ET were divided into two groups: a delayed-onset consecutive ET group and a continuous consecutive ET group. Patients with persisting esodeviation of more than 4 PD throughout the follow-up period after surgery despite non-surgical treatment were included in the continuous consecutive ET group, while those who re-developed esodeviation of more than 4 PD after obtaining orthophoria at one month after initial postoperative overcorrection for surgical correction of intermittent exotropia were included in the delayed-onset group.
At the initial visit, all patients underwent best-corrected visual acuity and manifest refraction (Auto refractor RKF1, Canon, Japan), measurement of near and distant angles of exodeviation, ocular motor test, and the suppression test. The angle of deviation (PD) was determined using the prism and alternative cover test at both short (33 cm) and long (6 m) distances. The suppression was measured at distance fixation using a vectrogram (Vectographic Projector Test; Reneau, France). All measurements were obtained by an experienced pediatric ophthalmologist (SHK).
All patients underwent BLR muscle recession as the initial surgery for treatment of intermittent exotropia. BLR recession was performed on stable exodeviation, which was defined as exodeviation that exceeded 25 PD. All surgeries were carried out by one experienced pediatric ophthalmologist (SHK). Surgical correction amount was considered using standard tables [4].
Non-surgical treatment for consecutive ET before considering surgical treatment consisted of part-time patching and prism glasses therapy. Alternate full-time patching was applied to all patients from postoperative day one for treatment of surgical overcorrection. Patients with esodeviation of more than 4 PD or who complained of diplopia despite alternate full-time patching were treated with prism glasses. These conservative management strategies were applied in both groups. Surgery for consecutive ET was performed on patients who persisted more than 10 PD of esodeviation for a minimum of six months, who had suppression in one eye, who had diplopia, and cases that did not achieve fine stereopsis.
Age at exotropia surgery, sex, visual acuity, spherical equivalent, preoperative and postoperative angles of deviation, suppression, stereopsis, and follow-up periods were compared between the two groups.
Statistical analysis was performed using the IBM SPSS Statistics ver. 24.0 (IBM Corp., Armonk, NY, USA). The clinical characteristics of the two groups were compared using the Mann-Whitney U-test and Pearson chi-square tests. A p-value <0.05 was considered statistically significant.
Go to : 
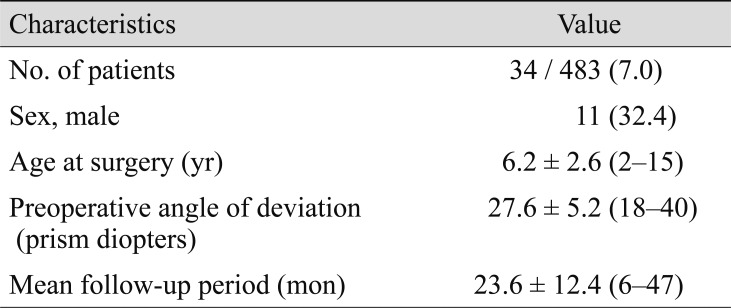
Among 483 patients who underwent BLR recession for surgical treatment of intermittent exotropia during the study period, 34 (7.0%) were diagnosed with consecutive ET (Table 1). Eleven patients (32.4%) were male; the mean age at surgery was 6.2 ± 2.6 years (range, 2–15 years), while the average preoperative exodeviation was 27.6 ± 5.2 PD (range, 18–40 PD). The mean follow-up period was 23.6 ± 12.4 months (range, 6–47 months).
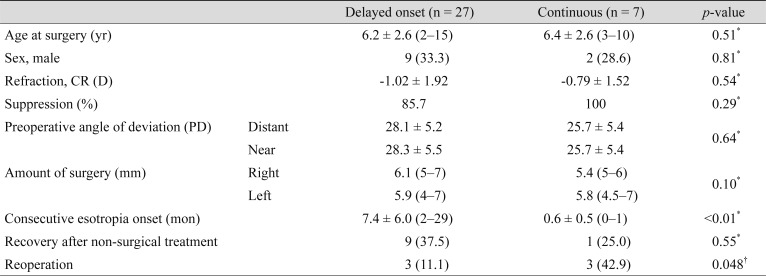
Twenty-seven patients were in the delayed-onset consecutive ET group, and 7 patients were in the continuous consecutive ET group. Baseline characteristics of age at operation, sex, spherical equivalent, suppression, preoperative angle of exodeviation, and surgical amount were comparable between the two groups (Table 2).
In the delayed-onset consecutive ET group, 37.5% of the patients recovered to orthotropia, compared to 25% of patients in the continuous consecutive ET group. The re-operation rate of consecutive ET patients was 11.1% in the delayed-onset group, and 42.9% of patients in the continuous group underwent reoperation for ET (p = 0.048).
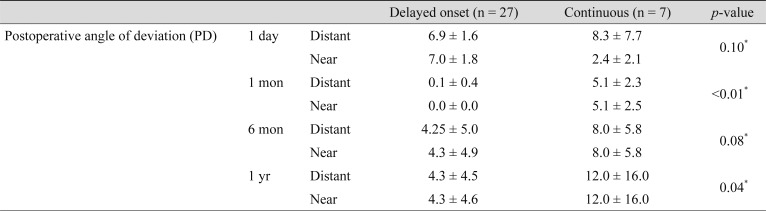
There were no statistically significant differences in postoperative angle of deviation at postoperative day one or six months (p = 0.10 and p = 0.08, respectively), but the amount of distant exodeviation at one month postoperatively was 0.1 ± 0.4 PD (range, 0–2 PD) in the delayed-onset group and 5.1 ± 2.3 PD (range, 4–10 PD) in the continuous group (p < 0.01). The amount of distant deviation at one year postoperatively was 4.3 ± 4.5 PD (range, 0–18 PD) in the delayed-onset group and 12.0 ± 16.0 PD (range, 0–40 PD) in the continuous group (p = 0.04) (Table 3).
Go to : 
Previous studies have reported the incidence of consecutive ET to range from 6% [12] to 15% [13]. Our study showed that 7% of intermittent exotropia patients who underwent BLR recession developed consecutive ET. The increase in medial rectus muscle tone after BLR recession may play a role in development of consecutive ET following BLR recession, but there is no consensus on the pathogenic mechanism [1415]. Known risk factors for consecutive ET are high accommodative convergence/accommodation ratio [45], lateral incomitancy [3], and age at surgery [6]; a previous study showed that larger esodeviation at postoperative one month was more likely to proceed to secondary surgery [16].
Recently, we have noticed an increase in patients who develop esodeviation after surgery, even after recovering to orthotropia. We defined this type of consecutive ET cases as delayed-onset consecutive ET. The cause of this increase is unknown, but an increase of “near work” in the current generation during the unstable postoperative period within several early months after surgery may have played a role [17].
In this study, patients with continuous consecutive ET were compared to patients who experienced delayed development of esodeviation after recovering to orthotropia within one month of BLR recession. As fewer patients with delayed-onset ET required a second operation and responded well to conservative treatment, the prognosis of delayed-onset consecutive ET was more favorable compared to that of continuous consecutive ET. A larger percentage of patients with continuous consecutive ET failed conservative treatment, such as part-time patching and prism glasses, and had to undergo a second procedure. The mechanism that causes this difference in prognosis is not fully understood, but recovery to orthotropia may be a factor in prognosis of consecutive ET.
The limitations of this study are its retrospective design, non-randomized and uncontrolled structure, and small number of cases.
The re-operation rate of delayed-onset consecutive ET after surgical correction of intermittent exotropia was lower than the re-operation rate of persistent consecutive ET.
Go to : 
References
1. Burian HM, Spivey BE. The surgical management of exodeviations. Am J Ophthalmol. 1965; 59:603–620. PMID: 14270998.
2. Hardesty HH, Boynton JR, Keenan JP. Treatment of intermittent exotropia. Arch Ophthalmol. 1978; 96:268–274. PMID: 629674.

3. Jang JH, Park JM, Lee SJ. Factors predisposing to consecutive esotropia after surgery to correct intermittent exotropia. Graefes Arch Clin Exp Ophthalmol. 2012; 250:1485–1490. PMID: 22450527.

4. Raab EL, Parks MM. Recession of the lateral recti. Early and late postoperative alignments. Arch Ophthalmol. 1969; 82:203–208. PMID: 5796092.
5. Edelman PM, Brown MH, Murphree AL, Wright KW. Consecutive esodeviation…then what? Am Orthopt J. 1988; 38:111–116.
6. Keech RV, Stewart SA. The surgical overcorrection of intermittent exotropia. J Pediatr Ophthalmol Strabismus. 1990; 27:218–220. PMID: 2391624.

7. von Noorden GK. Binocular vision and ocular motility. 6th ed. St. Louis: Mosby;2002. p. 371–372.
8. Choi YJ, Kim DH. Clinical course of consecutive esotropia after surgery to correct recurrent intermittent exotropia. J Korean Ophthalmol Soc. 2016; 57:1625–1630.

9. Hardesty HH. Treatment of overcorrected intermittent exotropia. Am J Ophthalmol. 1968; 66:80–86. PMID: 5659315.

11. Santiago AP, Ing MR, Kushner BJ, et al. Intermittent exotropia. In : Rosenbaum A, Santiago AP, editors. Clinical strabismus management: principles and surgical techniques. Philadelphia: Saunders;1999. p. 163–175.
12. Richard JM, Parks MM. Intermittent exotropia. Surgical results in different age groups. Ophthalmology. 1983; 90:1172–1177. PMID: 6657192.
13. Pratt-Johnson JA, Barlow JM, Tillson G. Early surgery in intermittent exotropia. Am J Ophthalmol. 1977; 84:689–694. PMID: 930997.

14. Lee TE, Kim SH. Accommodative and tonic convergence and anatomical contracture in partially accommodative and non-accommodative esotropia. Ophthalmic Physiol Opt. 2012; 32:535–538. PMID: 22804623.

15. Cho YA, Kim SH. Role of the equator in the early overcorrection of intermittent exotropia. J Pediatr Ophthalmol Strabismus. 2009; 46:30–34. PMID: 19213274.

16. Choi YM, Lee JY, Jung JH, et al. Risk factors predicting the need for additional surgery in consecutive esotropia. J Pediatr Ophthalmol Strabismus. 2013; 50:335–339. PMID: 24024671.

17. Lee JY, Ko SJ, Baek SU. Survival analysis following early surgical success in intermittent exotropia surgery. Int J Ophthalmol. 2014; 7:528–533. PMID: 24967204.
Go to : 




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download