1. Kovacs JA, Masur H. Evolving health effects of
Pneumocystis: one hundred years of progress in diagnosis and treatment. JAMA. 2009; 301:2578–2585. PMID:
19549975.
2. Catherinot E, Lanternier F, Bougnoux ME, Lecuit M, Couderc LJ, Lortholary O.
Pneumocystis jirovecii Pneumonia. Infect Dis Clin North Am. 2010; 24:107–138. PMID:
20171548.
3. Maini R, Henderson KL, Sheridan EA, Lamagni T, Nichols G, Delpech V, et al. Increasing
Pneumocystis pneumonia, England, UK, 2000–2010. Emerg Infect Dis. 2013; 19:386–392. PMID:
23622345.
4. Reid AB, Chen SC, Worth LJ.
Pneumocystis jirovecii pneumonia in non-HIV-infected patients: new risks and diagnostic tools. Curr Opin Infect Dis. 2011; 24:534–544. PMID:
21986616.
5. Tasaka S, Tokuda H.
Pneumocystis jirovecii pneumonia in non-HIV-infected patients in the era of novel immunosuppressive therapies. J Infect Chemother. 2012; 18:793–806. PMID:
22864454.
6. Enomoto T, Azuma A, Kohno A, Kaneko K, Saito H, Kametaka M, et al. Differences in the clinical characteristics of
Pneumocystis jirovecii pneumonia in immunocompromized patients with and without HIV infection. Respirology. 2010; 15:126–131. PMID:
19947989.
7. Kovacs JA, Hiemenz JW, Macher AM, Stover D, Murray HW, Shelhamer J, et al.
Pneumocystis carinii pneumonia: a comparison between patients with the acquired immunodeficiency syndrome and patients with other immunodeficiencies. Ann Intern Med. 1984; 100:663–671. PMID:
6231873.
8. Limper AH, Offord KP, Smith TF, Martin WJ 2nd.
Pneumocystis carinii pneumonia: differences in lung parasite number and inflammation in patients with and without AIDS. Am Rev Respir Dis. 1989; 140:1204–1209. PMID:
2817582.
9. Tasaka S, Kobayashi S, Kamata H, Kimizuka Y, Fujiwara H, Funatsu Y, et al. Cytokine profiles of bronchoalveolar lavage fluid in patients with pneumocystis pneumonia. Microbiol Immunol. 2010; 54:425–433. PMID:
20618689.

10. Thomas CF Jr, Limper AH.
Pneumocystis pneumonia. N Engl J Med. 2004; 350:2487–2498. PMID:
15190141.
11. Carmona EM, Limper AH. Update on the diagnosis and treatment of
Pneumocystis pneumonia. Ther Adv Respir Dis. 2011; 5:41–59. PMID:
20736243.
12. Flori P, Bellete B, Durand F, Raberin H, Cazorla C, Hafid J, et al. Comparison between real-time PCR, conventional PCR and different staining techniques for diagnosing
Pneumocystis jiroveci pneumonia from bronchoalveolar lavage specimens. J Med Microbiol. 2004; 53:603–607. PMID:
15184529.
13. Caliendo AM, Hewitt PL, Allega JM, Keen A, Ruoff KL, Ferraro MJ. Performance of a PCR assay for detection of
Pneumocystis carinii from respiratory specimens. J Clin Microbiol. 1998; 36:979–982. PMID:
9542920.
14. Alvarez-Martinez MJ, Miro JM, Valls ME, Moreno A, Rivas PV, Sole M, et al. Sensitivity and specificity of nested and real-time PCR for the detection of
Pneumocystis jiroveci in clinical specimens. Diagn Microbiol Infect Dis. 2006; 56:153–160. PMID:
16678378.
15. Ribes JA, Limper AH, Espy MJ, Smith TF. PCR detection of
Pneumocystis carinii in bronchoalveolar lavage specimens: analysis of sensitivity and specificity. J Clin Microbiol. 1997; 35:830–835. PMID:
9157136.
16. Fan LC, Lu HW, Cheng KB, Li HP, Xu JF. Evaluation of PCR in bronchoalveolar lavage fluid for diagnosis of
Pneumocystis jirovecii pneumonia: a bivariate meta-analysis and systematic review. PLoS One. 2013; 8:e73099. PMID:
24023814.
17. Nakashima K, Aoshima M, Ohkuni Y, Hoshino E, Hashimoto K, Otsuka Y. Loop-mediated isothermal amplification method for diagnosing
Pneumocystis pneumonia in HIV-uninfected immunocompromised patients with pulmonary infiltrates. J Infect Chemother. 2014; 20:757–761. PMID:
25187511.
18. Obayashi T, Negishi K, Suzuki T, Funata N. Reappraisal of the serum (1-->3)-beta-D-glucan assay for the diagnosis of invasive fungal infections: a study based on autopsy cases from 6 years. Clin Infect Dis. 2008; 46:1864–1870. PMID:
18462174.
19. Onishi A, Sugiyama D, Kogata Y, Saegusa J, Sugimoto T, Kawano S, et al. Diagnostic accuracy of serum 1,3-beta-D-glucan for pneumocystis jiroveci pneumonia, invasive candidiasis, and invasive aspergillosis: systematic review and meta-analysis. J Clin Microbiol. 2012; 50:7–15. PMID:
22075593.
20. Tasaka S, Hasegawa N, Kobayashi S, Yamada W, Nishimura T, Takeuchi T, et al. Serum indicators for the diagnosis of
pneumocystis pneumonia. Chest. 2007; 131:1173–1180. PMID:
17426225.
21. Watanabe T, Yasuoka A, Tanuma J, Yazaki H, Honda H, Tsukada K, et al. Serum (1-->3) beta-D-glucan as a noninvasive adjunct marker for the diagnosis of
Pneumocystis pneumonia in patients with AIDS. Clin Infect Dis. 2009; 49:1128–1131. PMID:
19725788.
22. de Boer MG, Gelinck LB, van Zelst BD, van de Sande WW, Willems LN, van Dissel JT, et al. beta-D-glucan and S-adenosylmethionine serum levels for the diagnosis of
Pneumocystis pneumonia in HIV-negative patients: a prospective study. J Infect. 2011; 62:93–100. PMID:
20970450.
23. Tasaka S, Kobayashi S, Yagi K, Asami T, Namkoong H, Yamasawa W, et al. Serum (1 --> 3) beta-D-glucan assay for discrimination between
Pneumocystis jirovecii pneumonia and colonization. J Infect Chemother. 2014; 20:678–681. PMID:
25066434.
24. Koga M, Koibuchi T, Kikuchi T, Nakamura H, Miura T, Iwamoto A, et al. Kinetics of serum beta-D-glucan after
Pneumocystis pneumonia treatment in patients with AIDS. Intern Med. 2011; 50:1397–1401. PMID:
21720059.
25. Roblot F, Godet C, Le Moal G, Garo B, Faouzi Souala M, Dary M, et al. Analysis of underlying diseases and prognosis factors associated with
Pneumocystis carinii pneumonia in immunocompromised HIV-negative patients. Eur J Clin Microbiol Infect Dis. 2002; 21:523–531. PMID:
12172743.
26. Quist J, Hill AR. Serum lactate dehydrogenase (LDH) in
Pneumocystis carinii pneumonia, tuberculosis, and bacterial pneumonia. Chest. 1995; 108:415–418. PMID:
7634877.
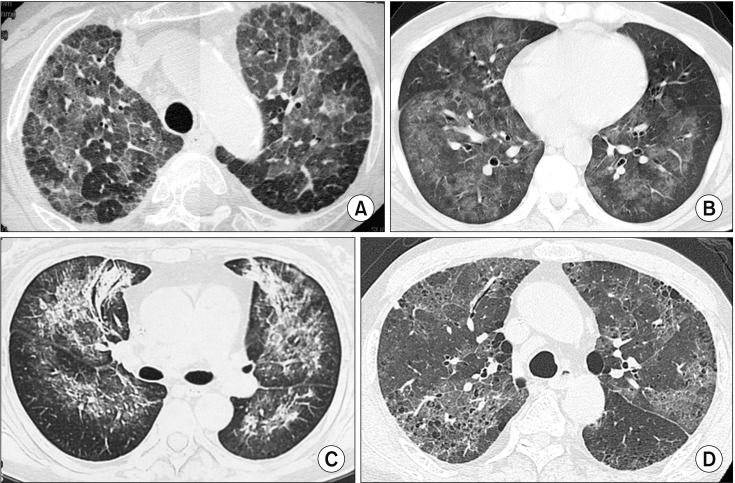
27. Kuhlman JE, Kavuru M, Fishman EK, Siegelman SS.
Pneumocystis carinii pneumonia: spectrum of parenchymal CT findings. Radiology. 1990; 175:711–714. PMID:
2343118.
28. Fujii T, Nakamura T, Iwamoto A.
Pneumocystis pneumonia in patients with HIV infection: clinical manifestations, laboratory findings, and radiological features. J Infect Chemother. 2007; 13:1–7. PMID:
17334722.
29. Tokuda H, Sakai F, Yamada H, Johkoh T, Imamura A, Dohi M, et al. Clinical and radiological features of
Pneumocystis pneumonia in patients with rheumatoid arthritis, in comparison with methotrexate pneumonitis and
Pneumocystis pneumonia in acquired immunodeficiency syndrome: a multicenter study. Intern Med. 2008; 47:915–923. PMID:
18480575.
30. Kameda H, Tokuda H, Sakai F, Johkoh T, Mori S, Yoshida Y, et al. Clinical and radiological features of acute-onset diffuse interstitial lung diseases in patients with rheumatoid arthritis receiving treatment with biological agents: importance of
Pneumocystis pneumonia in Japan revealed by a multicenter study. Intern Med. 2011; 50:305–313. PMID:
21325762.
31. Tasaka S, Tokuda H, Sakai F, Fujii T, Tateda K, Johkoh T, et al. Comparison of clinical and radiological features of pneumocystis pneumonia between malignancy cases and acquired immunodeficiency syndrome cases: a multicenter study. Intern Med. 2010; 49:273–281. PMID:
20154431.

32. Hardak E, Brook O, Yigla M. Radiological features of
Pneumocystis jirovecii pneumonia in immunocompromised patients with and without AIDS. Lung. 2010; 188:159–163. PMID:
20049469.
33. Kaplan JE, Benson C, Holmes KK, Brooks JT, Pau A, Masur H, et al. Guidelines for prevention and treatment of opportunistic infections in HIV-infected adults and adolescents: recommendations from CDC, the National Institutes of Health, and the HIV Medicine Association of the Infectious Diseases Society of America. MMWR Recomm Rep. 2009; 58:1–207.

34. Thomas M, Rupali P, Woodhouse A, Ellis-Pegler R. Good outcome with trimethoprim 10 mg/kg/day-sulfamethoxazole 50 mg/kg/day for Pneumocystis jirovecii pneumonia in HIV infected patients. Scand J Infect Dis. 2009; 41:862–868. PMID:
19922070.

35. Nakashima K, Aoshima M, Nakashita T, Hara M, Otsuki A, Noma S, et al. Low-dose trimethoprim-sulfamethoxazole treatment for pneumocystis pneumonia in non-human immunodeficiency virus-infected immunocompromised patients: a single-center retrospective observational cohort study. J Microbiol Immunol Infect. 2018; 51:810–820. PMID:
28779879.

36. Limper AH, Knox KS, Sarosi GA, Ampel NM, Bennett JE, Catanzaro A, et al. An official American Thoracic Society statement: treatment of fungal infections in adult pulmonary and critical care patients. Am J Respir Crit Care Med. 2011; 183:96–128. PMID:
21193785.

37. Helweg-Larsen J, Benfield T, Atzori C, Miller RF. Clinical efficacy of first- and second-line treatments for HIV-associated
Pneumocystis jirovecii pneumonia: a tri-centre cohort study. J Antimicrob Chemother. 2009; 64:1282–1290. PMID:
19858161.
38. Nahimana A, Rabodonirina M, Bille J, Francioli P, Hauser PM. Mutations of
Pneumocystis jirovecii dihydrofolate reductase associated with failure of prophylaxis. Antimicrob Agents Chemother. 2004; 48:4301–4305. PMID:
15504856.
39. Huang L, Cattamanchi A, Davis JL, den Boon S, Kovacs J, Meshnick S, et al. HIV-associated
Pneumocystis pneumonia. Proc Am Thorac Soc. 2011; 8:294–300. PMID:
21653531.
40. Briel M, Boscacci R, Furrer H, Bucher HC. Adjunctive corticosteroids for
Pneumocystis jiroveci pneumonia in patients with HIV infection: a meta-analysis of randomised controlled trials. BMC Infect Dis. 2005; 5:101. PMID:
16271157.

41. Pareja JG, Garland R, Koziel H. Use of adjunctive corticosteroids in severe adult non-HIV
Pneumocystis carinii pneumonia. Chest. 1998; 113:1215–1224. PMID:
9596297.
42. Moon SM, Kim T, Sung H, Kim MN, Kim SH, Choi SH, et al. Outcomes of moderate-to-severe
Pneumocystis pneumonia treated with adjunctive steroid in non-HIV-infected patients. Antimicrob Agents Chemother. 2011; 55:4613–4618. PMID:
21788460.
43. Delclaux C, Zahar JR, Amraoui G, Leleu G, Lebargy F, Brochard L, et al. Corticosteroids as adjunctive therapy for severe
Pneumocystis carinii pneumonia in non-human immunodeficiency virus-infected patients: retrospective study of 31 patients. Clin Infect Dis. 1999; 29:670–672. PMID:
10530464.
44. Segal BH, Freifeld AG, Baden LR, Brown AE, Casper C, Dubberke E, et al. Prevention and treatment of cancer-related infections. J Natl Compr Canc Netw. 2008; 6:122–174. PMID:
18319048.

45. Centers for Disease Control and Prevention. Infectious Disease Society of America. American Society of Blood and Marrow Transplantation. Guidelines for preventing opportunistic infections among hematopoietic stem cell transplant recipients. MMWR Recomm Rep. 2000; 49:1–125.
46. Kasiske BL, Zeier MG, Chapman JR, Craig JC, Ekberg H, Garvey CA, et al. KDIGO clinical practice guideline for the care of kidney transplant recipients: a summary. Kidney Int. 2010; 77:299–311. PMID:
19847156.

47. Martin SI, Fishman JA. AST Infectious Diseases Community of Practice. Pneumocystis pneumonia in solid organ transplant recipients. Am J Transplant. 2009; 9 Suppl 4:S227–S233. PMID:
20070684.

48. Hughes WT, Rivera GK, Schell MJ, Thornton D, Lott L. Successful intermittent chemoprophylaxis for
Pneumocystis carinii pneumonitis. N Engl J Med. 1987; 316:1627–1632. PMID:
3495732.
49. Utsunomiya M, Dobashi H, Odani T, Saito K, Yokogawa N, Nagasaka K, et al. Optimal regimens of sulfamethoxazoletrimethoprim for chemoprophylaxis of
Pneumocystis pneumonia in patients with systemic rheumatic diseases: results from a non-blinded, randomized controlled trial. Arthritis Res Ther. 2017; 19:7. PMID:
28100282.

50. Mizushina K, Hirata A, Hayashi N, Takenaka S, Ito H, Ogura T, et al. Possible preventive effect of salazosulfapyridine against development of
Pneumocystis pneumonia in methotrexate-receiving patients with rheumatoid arthritis. Mod Rheumatol. 2016; 26:976–978. PMID:
26565613.
51. Nunokawa T, Yokogawa N, Shimada K, Sugii S, Nishino J, Gosho M, et al. Prophylactic effect of sulfasalazine against
Pneumocystis pneumonia in patients with rheumatoid arthritis: a nested case-control study. Semin Arthritis Rheum. 2019; 48:573–578. PMID:
30057321.
52. Wang J, Gigliotti F, Bhagwat SP, George TC, Wright TW. Immune modulation with sulfasalazine attenuates immunopathogenesis but enhances macrophage-mediated fungal clearance during Pneumocystis pneumonia. PLoS Pathog. 2010; 6:e1001058. PMID:
20808846.

53. Anand S, Samaniego M, Kaul DR. Pneumocystis jirovecii pneumonia is rare in renal transplant recipients receiving only one month of prophylaxis. Transpl Infect Dis. 2011; 13:570–574. PMID:
22093215.

54. Le Gal S, Pougnet L, Damiani C, Frealle E, Gueguen P, Virmaux M, et al.
Pneumocystis jirovecii in the air surrounding patients with
Pneumocystis pulmonary colonization. Diagn Microbiol Infect Dis. 2015; 82:137–142. PMID:
25801779.
55. Yazaki H, Goto N, Uchida K, Kobayashi T, Gatanaga H, Oka S. Outbreak of
Pneumocystis jiroveci pneumonia in renal transplant recipients:
P. jiroveci is contagious to the susceptible host. Transplantation. 2009; 88:380–385. PMID:
19667941.
56. de Boer MG, de Fijter JW, Kroon FP. Outbreaks and clustering of
Pneumocystis pneumonia in kidney transplant recipients: a systematic review. Med Mycol. 2011; 49:673–680. PMID:
21453224.
57. Matsumura Y, Shindo Y, Iinuma Y, Yamamoto M, Shirano M, Matsushima A, et al. Clinical characteristics of
Pneumocystis pneumonia in non-HIV patients and prognostic factors including microbiological genotypes. BMC Infect Dis. 2011; 11:76. PMID:
21439061.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download