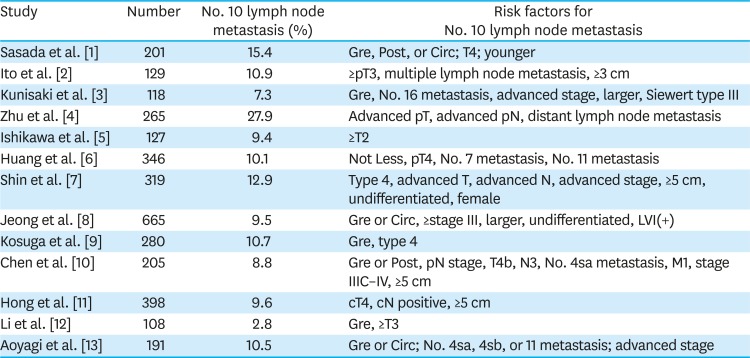
1. Sasada S, Ninomiya M, Nishizaki M, Harano M, Ojima Y, Matsukawa H, et al. Frequency of lymph node metastasis to the splenic hilus and effect of splenectomy in proximal gastric cancer. Anticancer Res. 2009; 29:3347–3351. PMID:
19661354.
2. Ito H, Inoue H, Odaka N, Satodate H, Mukai S, Omoto T, et al. Prognostic impact of prophylactic splenectomy for upper-third gastric cancer: a cohort study. Anticancer Res. 2013; 33:277–282. PMID:
23267157.
3. Kunisaki C, Makino H, Suwa H, Sato T, Oshima T, Nagano Y, et al. Impact of splenectomy in patients with gastric adenocarcinoma of the cardia. J Gastrointest Surg. 2007; 11:1039–1044. PMID:
17514409.

4. Zhu GL, Sun Z, Wang ZN, Xu YY, Huang BJ, Xu Y, et al. Splenic hilar lymph node metastasis independently predicts poor survival for patients with gastric cancers in the upper and/or the middle third of the stomach. J Surg Oncol. 2012; 105:786–792. PMID:
22105768.

5. Ishikawa S, Shimada S, Miyanari N, Hirota M, Takamori H, Baba H. Pattern of lymph node involvement in proximal gastric cancer. World J Surg. 2009; 33:1687–1692. PMID:
19488813.

6. Huang CM, Zhang JR, Zheng CH, Li P, Xie JW, Wang JB, et al. A 346 case analysis for laparoscopic spleen-preserving no.10 lymph node dissection for proximal gastric cancer: a single center study. PLoS One. 2014; 9:e108480. PMID:
25264673.

7. Shin SH, Jung H, Choi SH, An JY, Choi MG, Noh JH, et al. Clinical significance of splenic hilar lymph node metastasis in proximal gastric cancer. Ann Surg Oncol. 2009; 16:1304–1309. PMID:
19241107.

8. Jeong O, Jung MR, Ryu SY. Clinicopathological features and prognostic impact of splenic hilar lymph node metastasis in proximal gastric carcinoma. Eur J Surg Oncol. 2019; 45:432–438. PMID:
30389304.

9. Kosuga T, Ichikawa D, Okamoto K, Komatsu S, Shiozaki A, Fujiwara H, et al. Survival benefits from splenic hilar lymph node dissection by splenectomy in gastric cancer patients: relative comparison of the benefits in subgroups of patients. Gastric Cancer. 2011; 14:172–177. PMID:
21331530.

10. Chen XL, Yang K, Zhang WH, Chen XZ, Zhang B, Chen ZX, et al. Metastasis, risk factors and prognostic significance of splenic hilar lymph nodes in gastric adenocarcinoma. PLoS One. 2014; 9:e99650. PMID:
24915065.

11. Hong ZL, Chen QY, Zheng CH, Li P, Xie JW, Wang JB, et al. A preoperative scoring system to predict the risk of No.10 lymph node metastasis for advanced upper gastric cancer: a large case report based on a single-center study. Oncotarget. 2017; 8:80050–80060. PMID:
29108387.

12. Li P, Huang CM, Zheng CH, Xie JW, Wang JB, Lin JX, et al. Laparoscopic spleen-preserving splenic hilar lymphadenectomy in 108 consecutive patients with upper gastric cancer. World J Gastroenterol. 2014; 20:11376–11383. PMID:
25170225.

13. Aoyagi K, Kouhuji K, Miyagi M, Imaizumi T, Kizaki J, Shirouzu K. Prognosis of metastatic splenic hilum lymph node in patients with gastric cancer after total gastrectomy and splenectomy. World J Hepatol. 2010; 2:81–86. PMID:
21160977.

14. Kristinsson SY, Gridley G, Hoover RN, Check D, Landgren O. Long-term risks after splenectomy among 8,149 cancer-free American veterans: a cohort study with up to 27 years follow-up. Haematologica. 2014; 99:392–398. PMID:
24056815.

15. Zakeri S, Gorji N, Akhtari M, Moeini R. Splenectomy may have more complications than currently proven. Med Hypotheses. 2018; 112:43–46. PMID:
29447937.

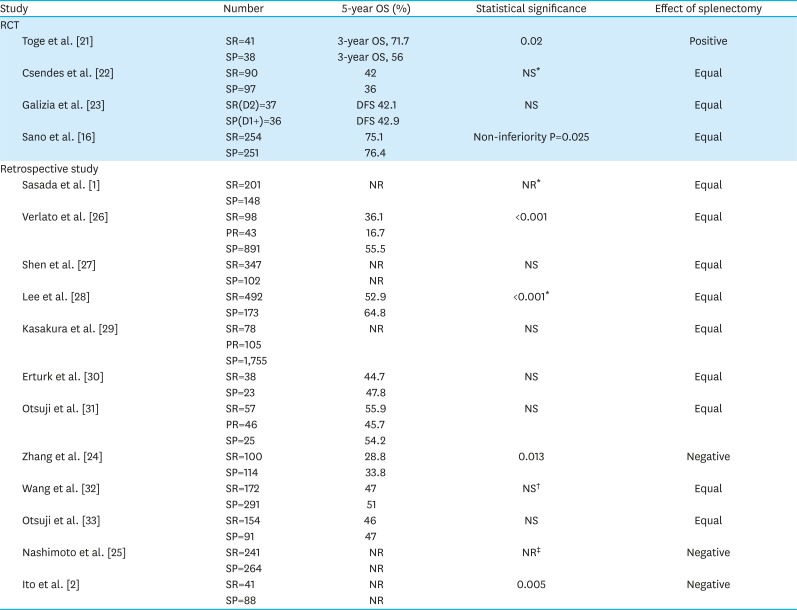
16. Sano T, Sasako M, Mizusawa J, Yamamoto S, Katai H, Yoshikawa T, et al. Randomized controlled trial to evaluate splenectomy in total gastrectomy for proximal gastric carcinoma. Ann Surg. 2017; 265:277–283. PMID:
27280511.

17. Uyama I, Sugioka A, Sakurai Y, Komori Y, Hanai T, Matsui H, et al. Hand-assisted laparoscopic function- preserving and radical gastrectomies for advanced-stage proximal gastric cancer. J Am Coll Surg. 2004; 199:508–515. PMID:
15325625.
18. Huang CM, Chen QY, Lin JX, Zheng CH, Li P, Xie JW. Huang's three-step maneuver for laparoscopic spleen-preserving No. 10 lymph node dissection for advanced proximal gastric cancer. Chin J Cancer Res. 2014; 26:208–210. PMID:
24826062.
19. Kinoshita T, Shibasaki H, Enomoto N, Sahara Y, Sunagawa H, Nishida T. Laparoscopic splenic hilar lymph node dissection for proximal gastric cancer using integrated three-dimensional anatomic simulation software. Surg Endosc. 2016; 30:2613–2619. PMID:
26310530.

20. Japanese Gastric Cancer Association. Japanese classification of gastric carcinoma: 3rd English edition. Gastric Cancer. 2011; 14:101–112. PMID:
21573743.
21. Toge T, Kameda A, Kuroi K, Seto Y, Yamada H, Hattori T. The role of the spleen in immunosuppression and the effects of splenectomy on prognosis in gastric cancer patients. Nippon Geka Gakkai Zasshi. 1985; 86:1120–1123. PMID:
4088224.
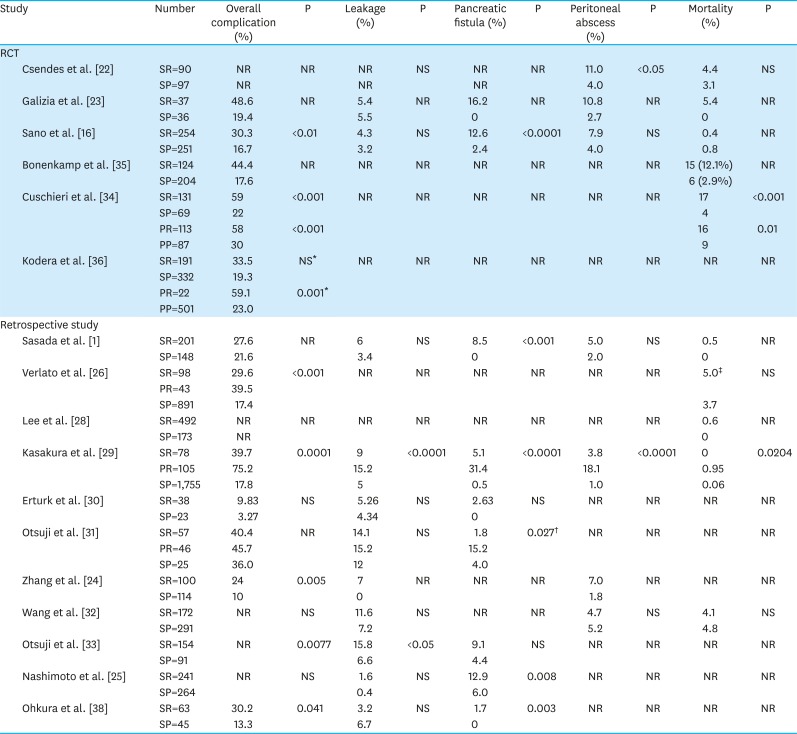
22. Csendes A, Burdiles P, Rojas J, Braghetto I, Diaz JC, Maluenda F. A prospective randomized study comparing D2 total gastrectomy versus D2 total gastrectomy plus splenectomy in 187 patients with gastric carcinoma. Surgery. 2002; 131:401–407. PMID:
11935130.

23. Galizia G, Lieto E, De Vita F, Castellano P, Ferraraccio F, Zamboli A, et al. Modified versus standard D2 lymphadenectomy in total gastrectomy for nonjunctional gastric carcinoma with lymph node metastasis. Surgery. 2015; 157:285–296. PMID:
25532433.

24. Zhang H, Pang D, Xu H, Ren Y, Liu C. Is concomitant splenectomy beneficial for the long-term survival of patients with gastric cancer undergoing curative gastrectomy? A single-institution study. World J Surg Oncol. 2014; 12:193. PMID:
24969079.

25. Nashimoto A, Yabusaki H, Matsuki A. The significance of splenectomy for advanced proximal gastric cancer. Int J Surg Oncol. 2012; 2012:301530. PMID:
22685639.

26. Verlato G, Roviello F, Marchet A, Giacopuzzi S, Marrelli D, Nitti D, et al. Indexes of surgical quality in gastric cancer surgery: experience of an Italian network. Ann Surg Oncol. 2009; 16:594–602. PMID:
19118437.

27. Shen JG, Cheong JH, Hyung WJ, Kim J, Choi SH, Noh SH. Adverse effect of splenectomy on recurrence in total gastrectomy cancer patients with perioperative transfusion. Am J Surg. 2006; 192:301–305. PMID:
16920422.

28. Lee KY, Noh SH, Hyung WJ, Lee JH, Lah KH, Choi SH, et al. Impact of splenectomy for lymph node dissection on long-term surgical outcome in gastric cancer. Ann Surg Oncol. 2001; 8:402–406. PMID:
11407513.

29. Kasakura Y, Fujii M, Mochizuki F, Kochi M, Kaiga T. Is there a benefit of pancreaticosplenectomy with gastrectomy for advanced gastric cancer? Am J Surg. 2000; 179:237–242. PMID:
10827328.

30. Erturk S, Ersan Y, Cicek Y, Dogusoy G, Senocak M. Effect of simultaneous splenectomy on the survival of patients undergoing curative gastrectomy for proximal gastric carcinoma. Surg Today. 2003; 33:254–258. PMID:
12707818.
31. Otsuji E, Yamaguchi T, Sawai K, Okamoto K, Takahashi T. Total gastrectomy with simultaneous pancreaticosplenectomy or splenectomy in patients with advanced gastric carcinoma. Br J Cancer. 1999; 79:1789–1793. PMID:
10206294.

32. Wang F, Chang YC, Chen TH, Hsu JT, Kuo CJ, Lin CJ, et al. Prognostic significance of splenectomy for patients with gastric adenocarcinoma undergoing total gastrectomy: a retrospective cohort study. Int J Surg. 2014; 12:557–565. PMID:
24793232.

33. Otsuji E, Yamaguchi T, Sawai K, Ohara M, Takahashi T. End results of simultaneous splenectomy in patients undergoing total gastrectomy for gastric carcinoma. Surgery. 1996; 120:40–44. PMID:
8693421.

34. Cuschieri A, Fayers P, Fielding J, Craven J, Bancewicz J, Joypaul V, et al. Postoperative morbidity and mortality after D1 and D2 resections for gastric cancer: preliminary results of the MRC randomised controlled surgical trial. Lancet. 1996; 347:995–999. PMID:
8606613.

35. Bonenkamp JJ, Songun I, Hermans J, Sasako M, Welvaart K, Plukker JT, et al. Randomised comparison of morbidity after D1 and D2 dissection for gastric cancer in 996 Dutch patients. Lancet. 1995; 345:745–748. PMID:
7891484.

36. Kodera Y, Sasako M, Yamamoto S, Sano T, Nashimoto A, Kurita A. Identification of risk factors for the development of complications following extended and superextended lymphadenectomies for gastric cancer. Br J Surg. 2005; 92:1103–1109. PMID:
16106493.

37. Sano T, Sasako M, Yamamoto S, Nashimoto A, Kurita A, Hiratsuka M, et al. Gastric cancer surgery: morbidity and mortality results from a prospective randomized controlled trial comparing D2 and extended para-aortic lymphadenectomy--Japan Clinical Oncology Group study 9501. J Clin Oncol. 2004; 22:2767–2773. PMID:
15199090.

38. Ohkura Y, Haruta S, Shindoh J, Tanaka T, Ueno M, Udagawa H. Efficacy of prophylactic splenectomy for proximal advanced gastric cancer invading greater curvature. World J Surg Oncol. 2017; 15:106. PMID:
28545537.

39. Holdsworth RJ, Irving AD, Cuschieri A. Postsplenectomy sepsis and its mortality rate: actual versus perceived risks. Br J Surg. 1991; 78:1031–1038. PMID:
1933181.

40. Theilacker C, Ludewig K, Serr A, Schimpf J, Held J, Bögelein M, et al. Overwhelming postsplenectomy infection: a prospective multicenter cohort study. Clin Infect Dis. 2016; 62:871–878. PMID:
26703862.

41. Davidson RN, Wall RA. Prevention and management of infections in patients without a spleen. Clin Microbiol Infect. 2001; 7:657–660. PMID:
11843905.

42. Davies JM, Lewis MP, Wimperis J, Rafi I, Ladhani S, Bolton-Maggs PH. Review of guidelines for the prevention and treatment of infection in patients with an absent or dysfunctional spleen: prepared on behalf of the British Committee for Standards in Haematology by a working party of the Haemato-Oncology task force. Br J Haematol. 2011; 155:308–317. PMID:
21988145.

43. Mellemkjoer L, Olsen JH, Linet MS, Gridley G, McLaughlin JK. Cancer risk after splenectomy. Cancer. 1995; 75:577–583. PMID:
7812926.

44. Linet MS, Nyrén O, Gridley G, Mellemkjaer L, McLaughlin JK, Olsen JH, et al. Risk of cancer following splenectomy. Int J Cancer. 1996; 66:611–616. PMID:
8647621.

45. Sun LM, Chen HJ, Jeng LB, Li TC, Wu SC, Kao CH. Splenectomy and increased subsequent cancer risk: a nationwide population-based cohort study. Am J Surg. 2015; 210:243–251. PMID:
25986002.

46. Saji S, Sakamoto J, Teramukai S, Kunieda K, Sugiyama Y, Ohashi Y, et al. Impact of splenectomy and immunochemotherapy on survival following gastrectomy for carcinoma: covariate interaction with immunosuppressive acidic protein, a serum marker for the host immune system. Surg Today. 1999; 29:504–510. PMID:
10385364.

47. Cho MY, Kroh MD, Joh YG, Suh SO. Impact of splenectomy on circulating T-lymphocyte subsets in stage III gastric cancer. ANZ J Surg. 2002; 72:411–416. PMID:
12121160.

48. Pan D, Chen H, Li LQ, Li ZF. Effect of splenectomy combined with resection for gastric carcinoma on patient prognosis. Med Sci Monit. 2016; 22:4205–4209. PMID:
27816984.

49. Pommerening MJ, Rahbar E, Minei K, Holcomb JB, Wade CE, Schreiber MA, et al. Splenectomy is associated with hypercoagulable thrombelastography values and increased risk of thromboembolism. Surgery. 2015; 158:618–626. PMID:
26209572.

50. Mukherjee D, Lidor AO, Chu KM, Gearhart SL, Haut ER, Chang DC. Postoperative venous thromboembolism rates vary significantly after different types of major abdominal operations. J Gastrointest Surg. 2008; 12:2015–2022. PMID:
18668299.

51. Boyle S, White RH, Brunson A, Wun T. Splenectomy and the incidence of venous thromboembolism and sepsis in patients with immune thrombocytopenia. Blood. 2013; 121:4782–4790. PMID:
23637127.

52. Han JW, Kong SH, Shin CI, Min SK, Min SI, Kim TH, et al. Portomesenteric vein thrombosis after gastric surgery. Gastric Cancer. 2016; 19:1135–1143. PMID:
26541767.

53. Kang CM, Chung YE, Jung MJ, Hwang HK, Choi SH, Lee WJ. Splenic vein thrombosis and pancreatic fistula after minimally invasive distal pancreatectomy. Br J Surg. 2014; 101:114–119. PMID:
24327328.

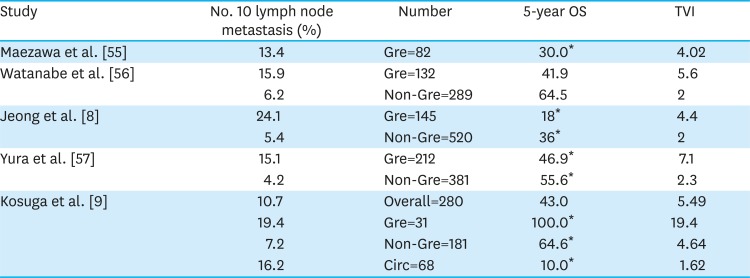
54. Huang CM, Wang JB, Lu HS, Zheng CH, Li P, Xie JW, et al. Prognostic impact of splenectomy on advanced proximal gastric cancer with No. 10 lymph node metastasis. Chin Med J (Engl). 2009; 122:2757–2762. PMID:
19951610.
55. Maezawa Y, Aoyama T, Yamada T, Kano K, Hayashi T, Sato T, et al. Priority of lymph node dissection for proximal gastric cancer invading the greater curvature. Gastric Cancer. 2018; 21:569–572. PMID:
29119277.

56. Watanabe M, Kinoshita T, Enomoto N, Shibasaki H, Nishida T. Clinical significance of splenic hilar dissection with splenectomy in advanced proximal gastric cancer: an analysis at a single institution in Japan. World J Surg. 2016; 40:1165–1171. PMID:
26630939.

57. Yura M, Yoshikawa T, Otsuki S, Yamagata Y, Morita S, Katai H, et al. The therapeutic survival benefit of splenic hilar nodal dissection for advanced proximal gastric cancer invading the greater curvature. Ann Surg Oncol. 2019; 26:829–835. PMID:
30569298.

58. Son SY, Kong SH, Ahn HS, Park YS, Ahn SH, Suh YS, et al. The value of N staging with the positive lymph node ratio, and splenectomy, for remnant gastric cancer: a multicenter retrospective study. J Surg Oncol. 2017; 116:884–893. PMID:
28650587.

59. Honda S, Bando E, Makuuchi R, Tokunaga M, Tanizawa Y, Kawamura T, et al. Effects of initial disease status on lymph flow following gastrectomy in cases of carcinoma in the remnant stomach. Gastric Cancer. 2017; 20:457–464. PMID:
27638289.

60. Sugita H, Oda E, Hirota M, Ishikawa S, Tomiyasu S, Tanaka H, et al. Significance of lymphadenectomy with splenectomy in radical surgery for advanced (pT3/pT4) remnant gastric cancer. Surgery. 2016; 159:1082–1089. PMID:
26497772.

61. Ohashi M, Morita S, Fukagawa T, Kushima R, Katai H. Surgical treatment of non-early gastric remnant carcinoma developing after distal gastrectomy for gastric cancer. J Surg Oncol. 2015; 111:208–212. PMID:
25175816.

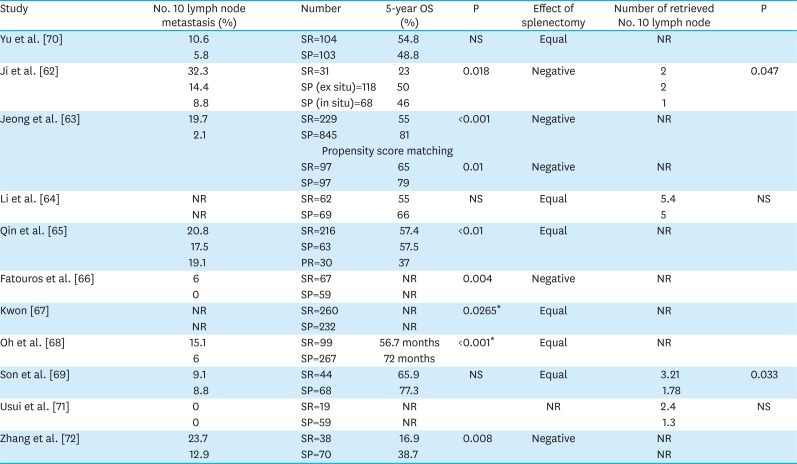
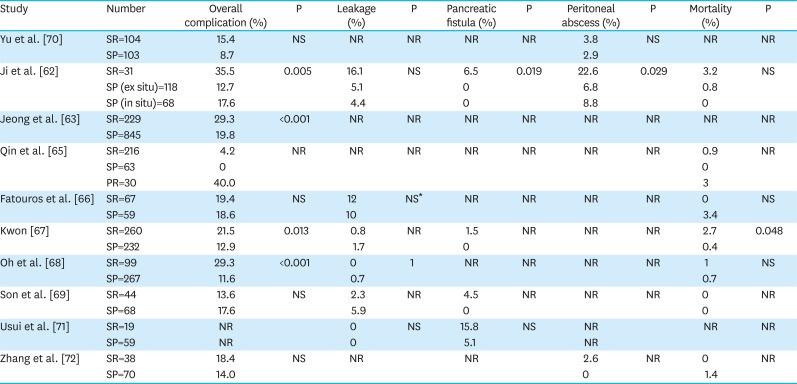
62. Ji X, Fu T, Bu ZD, Zhang J, Wu XJ, Zong XL, et al. Comparison of different methods of splenic hilar lymph node dissection for advanced upper- and/or middle-third gastric cancer. BMC Cancer. 2016; 16:765. PMID:
27716191.

63. Jeong O, Kim HG, Ryu SY, Park YK, Jung MR. Adverse prognostic impact of splenectomy on survival in gastric carcinoma patients: regression and propensity score matching analysis of 1074 patients. PLoS One. 2018; 13:e0203820. PMID:
30204783.

64. Li C, Kim S, Lai JF, Oh SJ, Hyung WJ, Choi WH, et al. Lymph node dissection around the splenic artery and hilum in advanced middle third gastric carcinoma. Eur J Surg Oncol. 2009; 35:709–714. PMID:
18455906.

65. Qin H, Lin C. Radical resection of gastric carcinoma with pancreas and spleen preservation and functional cleaning of lymph nodes. Chin Med J (Engl). 2002; 115:736–739. PMID:
12133545.
66. Fatouros M, Roukos DH, Lorenz M, Arampatzis I, Hottentrott C, Encke A, et al. Impact of spleen preservation in patients with gastric cancer. Anticancer Res. 2005; 25:3023–3030. PMID:
16080561.
67. Kwon SJ. Prognostic impact of splenectomy on gastric cancer: results of the Korean Gastric Cancer Study Group. World J Surg. 1997; 21:837–844. PMID:
9327675.

68. Oh SJ, Hyung WJ, Li C, Song J, Kang W, Rha SY, et al. The effect of spleen-preserving lymphadenectomy on surgical outcomes of locally advanced proximal gastric cancer. J Surg Oncol. 2009; 99:275–280. PMID:
19152367.

69. Son SY, Shin DJ, Park YS, Oo AM, Jung DH, Lee CM, et al. Spleen-preserving lymphadenectomy versus splenectomy in laparoscopic total gastrectomy for advanced gastric cancer. Surg Oncol. 2017; 26:207–211. PMID:
28577727.

70. Yu W, Choi GS, Chung HY. Randomized clinical trial of splenectomy versus splenic preservation in patients with proximal gastric cancer. Br J Surg. 2006; 93:559–563. PMID:
16607678.

71. Usui S, Tashiro M, Haruki S, Arita K, Ito K, Matsumoto A, et al. Spleen preservation versus splenectomy in laparoscopic total gastrectomy with D2 lymphadenectomy for gastric cancer: a comparison of short-term outcomes. Asian J Endosc Surg. 2016; 9:5–13. PMID:
26551257.

72. Zhang CH, Zhan WH, He YL, Chen CQ, Huang MJ, Cai SR. Spleen preservation in radical surgery for gastric cardia cancer. Ann Surg Oncol. 2007; 14:1312–1319. PMID:
17265118.

73. Huang CM, Chen T, Lin JX, Chen QY, Zheng CH, Li P, et al. The effects of laparoscopic spleen-preserving splenic hilar lymphadenectomy on the surgical outcome of proximal gastric cancer: a propensity score-matched, case-control study. Surg Endosc. 2017; 31:1383–1392. PMID:
27450211.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download