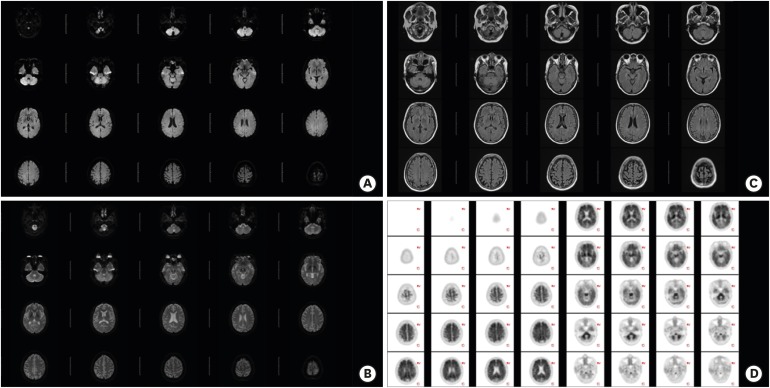
 | Fig. 1Brain magnetic resonance images. (A) Diffusion weighted image did not show abnormal findings. (B) Apparent diffusion coefficient image did not show abnormal findings. (C) Fluid-attenuated inversion recovery image showed mild periventricular leukoaraiosis. (D) Flutemetamol (18F) PET showed elevated cortical amyloid uptake.PET: positron emission tomography.
|
Dear Sir,
Creutzfeldt-Jakob disease (CJD) is the most common prion disease in humans. Once formed by unknown cause, PrPsc can make the normal cellular PrP (PrPc) transform into the pathogenic PrPsc in a cascade. Consequent extensive neuronal loss causes dementia, involuntary movement, psychosis, and incoordination. The criteria for clinical diagnosis include cerebrospinal fluid (CSF) biomarkers (e.g., 14-3-3 protein and t-tau), specific magnetic resonance image (MRI) finding, electroencephalography (EEG), and clinical symptoms.1 Recently, in vitro protein misfolding amplification system, the real-time quaking-induced conversion assay (RT-QuIC), for the detection of PrPsc in CSF was developed and showed ultra-high sensitivity and specificity, amending the diagnostic criteria.2 Here, we report the case of a patient without obvious clinical symptoms of sporadic Creutzfeldt-Jakob disease (sCJD) except rapidly progressive cognitive decline and a positive RT-QuIC assay who was not CJD.
An age 54 Korean female visited the clinic with progressive cognitive decline for 2 months. Her daughter noticed this when the patient, who is a storekeeper, had problems with calculations at the register. She also misplaced things and spent time searching for them. Also, she had difficulty verbally expressing herself and sometimes could not understand what others were saying. She graduated from high school in 12 years. Her medical history was unremarkable. A month ago, she was admitted to a university hospital for evaluation. On neuropsychological evaluation, visual and verbal memory, frontal/executive function and calculation impairment were noted. Her Mini-Mental State Examination was 23, Clinical Dementia Rating scale 1 (sum of box 4). Brain MRI did not show any lesion even on diffusion-weighted images (DWIs) (Fig. 1A). EEG showed mild cerebral dysfunction but no periodic sharp wave complexes. CSF analysis showed five white blood cells with normal chemistry. Autoimmune antibodies and tumor markers were negative. CSF 14-3-3 protein was weakly positive; and total tau (t-tau) level was elevated to 1,206 pg/mL. Additionally, RT-QuIC assay tested positive. Flutemetamol (18F) positron emission tomography showed elevated cortical amyloid uptake (Fig. 1B). She was discharged with a diagnosis of sCJD with superimposed Alzheimer's disease. Donepezil 5 mg was started. However, a month after discharge, she was stable without signs of aggravation. For a second opinion, she visited Asan Medical Center. EEG, and brain MRI DWI did not show abnormal findings. In CSF analysis, 14-3-3 protein was weakly positive, t-tau level increased to 1,336 pg/mL, p-tau to 144.7 pg/mL, and amyloid beta decreased to 116.7 pg/mL. Surprisingly, RT-QuIC assay tested negative at this time. The genetic testing for early onset Alzheimer's disease was all negative. Up to four months after discharge, she has remained cognitively stable. Together, the patient was diagnosed with Alzheimer's disease only, not related to sCJD.
The RT-QuIC exploits the ability of PrPsc to seed the polymerization of protease sensitive recombinant PrP into amyloid fibrils detectable by thioflavin-T fluorescence.3 This assay identifies cases of prion disease with a sensitivity of 80%–95% and a specificity of 99% when applied in symptomatic CJD patients. Amended criteria indicates probable sCJD when CSF RT-QuIC assay is positive and only one clinical symptom is present. Up to now, only eight cases have rendered a false positive RT-QuIC globally.4 If the prevalence of a disease is low, the positive predictive value will be low, although the specificity and sensitivity are high. As such, since CJD is a rare disease, the false positive rate may be higher than thought.
In our case, the patient had no symptoms other than dementia or signs of progression. CSF RT-QuIC was positive initially but was negative the second time. The current measurement system may not be entirely reliable. If an automated quantitative system is available, we may avoid even the remote possibility of false positive RT-QuIC test.5 Caution should be practiced in rendering a fatal diagnosis of sCJD, particularly in the patient with atypical clinical features. We should be mindful that even a highly specific diagnostic tool such as RT-QuIC test does not guarantee the diagnosis of sCJD and that it is safe to double check and repeat the test to allow for an alternative diagnosis until proven otherwise.
ACKNOWLEDGEMENTS
We thank the patient described for allowing us to share his medical details.
Go to : 
References
1. McGuire LI, Peden AH, Orrú CD, Wilham JM, Appleford NE, Mallinson G, et al. Real time quaking-induced conversion analysis of cerebrospinal fluid in sporadic Creutzfeldt-Jakob disease. Ann Neurol. 2012; 72:278–285. PMID: 22926858.

2. Franceschini A, Baiardi S, Hughson AG, McKenzie N, Moda F, Rossi M, et al. High diagnostic value of second generation CSF RT-QuIC across the wide spectrum of CJD prions. Sci Rep. 2017; 7:10655. PMID: 28878311.

3. Kang HE, Mo Y, Abd Rahim R, Lee HM, Ryou C. Prion diagnosis: application of real-time quaking-induced conversion. BioMed Res Int. 2017; 2017:5413936. PMID: 28596963.

5. Shi S, Mitteregger-Kretzschmar G, Giese A, Kretzschmar HA. Establishing quantitative real-time quaking-induced conversion (qRT-QuIC) for highly sensitive detection and quantification of PrPSc in prion-infected tissues. Acta Neuropathol Commun. 2013; 1:44. PMID: 24252329.

Go to : 




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download