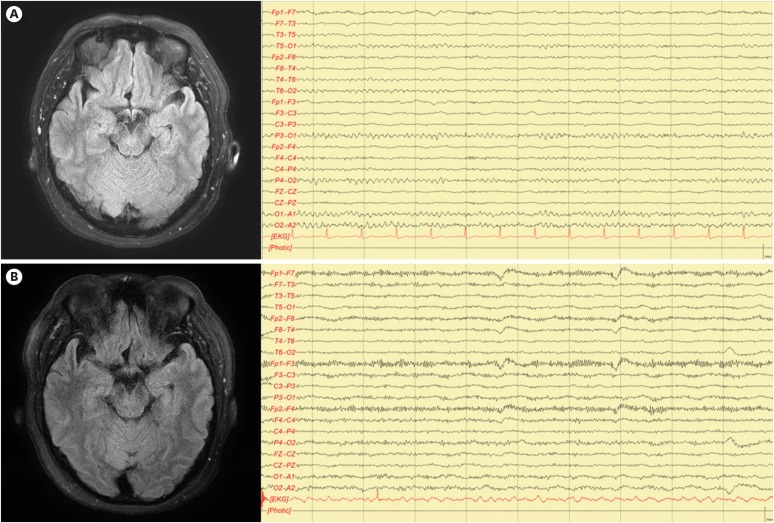
 | Fig. 1Brain MRI analysis. (A) Initial FLAIR enhanced image showed no abnormal lesion. EEG showed well-regulated rhythm without epileptiform discharge. (B) Follow-up FLAIR enhanced image showed no abnormal lesion, but EEG showed a mild, slow, and disorganized pattern.MRI: magnetic resonance imaging, FLAIR: fluid inversion recovery, EEG: electroencephalography.
|
Dear Editor,
Anti-N-methyl-D-aspartate receptor (anti-NMDAR) encephalitis is an immune-mediated disease, more common in females. It is often related to ovarian tumor.1 Clinically, it is characterized by rapid onset (<3 months) of diverse symptoms including abnormal behavioral change, decreased level of consciousness, speech dysfunction, epileptic seizure, autonomic dysfunction, psychosis, rigidity, and dyskinesia.1 The diagnostic criteria for definite anti-NMDAR encephalitis includes the presence of immunoglobulin G (IgG) antibodies against the GluN1 subunit of NMDAR.2 However, test for antibodies is not readily accessible in many institutions and can take weeks to obtain results.2 So diagnostic tests such as cerebrospinal fluid (CSF) analysis, electroencephalogram (EEG), and magnetic resonance imaging (MRI), are used as integral supportive findings, in addition to suggestive clinical symptoms and excluding other disorders. Here, we report a patient who presented with acute onset of psychosis with normal EEG, and normal brain MRI, and non-inflammatory CSF initially.
A previously healthy age 53 female visited the psychiatric department because of behavior change and emotional lability lasting for five days. The psychotic symptoms developed abruptly for the first time. She complained of visual hallucination, with no headache or fever. On neurological examination, she only had mild dysarthria and obtundated mentation. Brain MRI, EEG, and CSF analysis were performed. However, there was no abnormal finding in the brain MRI (Fig. 1A) and CSF analysis. Initial EEG showed well-regulated posterior dominant rhythm without epileptiform discharge or slow activities (Fig. 1A). One week later, her psychotic symptoms were aggravated. She showed generalized rigidity and could not speak coherently. We performed follow-up EEG, brain MRI, and CSF analysis. There were pleocytosis on the CSF analysis (white blood cell 18/mm3, red blood cell 3/mm3, protein 33 mg/dL), and the EEG showed a more slow and disorganized pattern (Fig. 1B). Brain MRI showed no significant abnormal findings. Laboratory tests including, anti-beta2 glycoptotein1 antibody, anti-nuclear antibody, antineutrophilic cytoplasmic antibody, and paraneoplastic antibodies (anti-Hu, anti-Yo, and anti-Ri) were negative. With a possibility of autoimmune or viral encephalitis, tests for anti-NMDAR antibodies were initiated, and steroid (1 g/day) with anti-viral agent were started. As there was no clinical change, intravenous immunoglobulin was initiated and she started to speak with single words one week later. Anti-NMDAR antibody was detected in CSF and serum, but no other infectious sources were detected. Chest and abdomen-pelvis computed tomography scan were performed, and only a uterine myoma was detected. Her psychotic symptoms fully improved 2 months after admission, and she was able to walk and talk as before the ictus.
We reported an uncommon case of anti-NMDAR encephalitis difficult to initially diagnosis. Before detecting anti-NMDAR antibodies, abnormal EEG and/or CSF with pleocytosis or oligoclonal bands are mandatory to diagnose probable anti-NMDAR encephalitis.2 In previous reports, initial non-inflammatory CSF were noted in 15%–96% of the patients.3 EEG could be a diagnostic aid, given that in most case series, it was abnormal in more than 90% of the cases.4 But findings were usually non-specific.5 Initial abnormality on MRI also varied, and was noted in 20%–50% of the cases.5 The absence of CSF pleocytosis and/or increased proteins are known to delay diagnosis, as well as the length of time to initiate immunotherapy in patients with anti-NMDA encephalitis.3 Additionally, EEG and MRI could be a diagnostic aid, but the absence of abnormality of them does not exclude anti-NMDAR encephalitis. In conclusion, follow up tests with close observation may be considered in patients with the atypical psychiatric symptoms, although there are initially no significant abnormal findings on CSF, MRI, and EEG.
References
1. Dalmau J, Armangué T, Planagumà J, Radosevic M, Mannara F, Leypoldt F, et al. An update on anti-NMDA receptor encephalitis for neurologists and psychiatrists: mechanisms and models. Lancet Neurol. 2019; 18:1045–1057. PMID: 31326280.

2. Graus F, Titulaer MJ, Balu R, Benseler S, Bien CG, Cellucci T, et al. A clinical approach to diagnosis of autoimmune encephalitis. Lancet Neurol. 2016; 15:391–404. PMID: 26906964.

3. Espinola-Nadurille M, Bautista-Gomez P, Flores J, Rivas-Alonso V, Perez-Esparza R, Solís-Vivanco R, et al. Non-inflammatory cerebrospinal fluid delays the diagnosis and start of immunotherapy in anti-NMDAR encephalitis. Arq Neuropsiquiatr. 2018; 76:2–5. PMID: 29364387.

4. Dalmau J, Gleichman AJ, Hughes EG, Rossi JE, Peng X, Lai M, et al. Anti-NMDA-receptor encephalitis: case series and analysis of the effects of antibodies. Lancet Neurol. 2008; 7:1091–1098. PMID: 18851928.

5. Lee SK, Lee ST. The laboratory diagnosis of autoimmune encephalitis. J Epilepsy Res. 2016; 6:45–50. PMID: 28101474.

Go to : 




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download