Abstract
Moving the mandibular posterior teeth into a severely atrophic edentulous space is a challenge. A carefully designed force-and-moment system that results in bodily protraction of the posterior teeth with balanced bone resorption and apposition is needed in such cases. This report describes the treatment of a 19-year-old woman with missing mandibular first molars due to juvenile periodontitis. Miniscrews were used as absolute anchorage during protraction of the mandibular second and third molars. Bodily mesial movement of the mandibular second and third molars was achieved over a distance of 11 to 17 mm after 39 months of orthodontic treatment.
Bridge or implant-based dentures are common treatment options for the space created by a missing first molar. An alternative treatment is orthodontic movement of the second and third molars into the space, precluding the need for bridge or implant-based dentures and the possible recovery of the deficient alveolar bone.1
However, the mandible has thick cortical bone and the mandibular molar roots are much wider buccolingually than mesiodistally, so the missing mandibular first molar space cannot be closed in some cases.2 Furthermore, safe and effective protraction of the molars is impossible if the alveolar ridge in the edentulous region has collapsed. Additional complications such as pulp vitality, dehiscence and fenestration, and root resorption may also be encountered in such cases.
Although many case reports have described successful protraction of themandibular second molar to close the old space caused by the missing first molar, there are few reports describing the protraction of mandibular second molars through severely atrophic edentulous spaces.13456 We report here the successful orthodontic movement of the second and third molars in a young adult with severely atrophic edentulous spaces caused by missing first molars.
A 19-year-old woman came to our office at the Department of Orthodontics, The Second Affiliated Hospital, Zhejiang University, with complaints of tipping molars, missing teeth, and alveolar atrophy not suitable for dental implant. She had undergone removal of several molars 3 months previously because of severe localized juvenile periodontitis. She had no chronic or systemic disease, and her medical history was unremarkable.
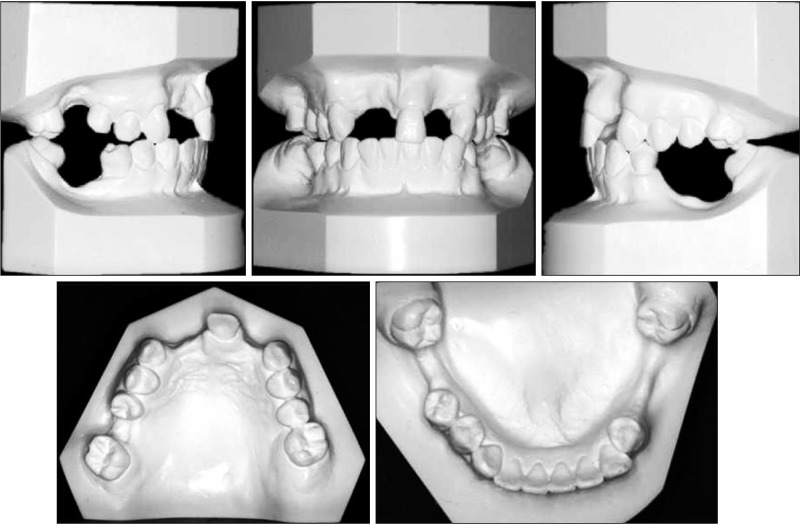
Her pretreatment facial photos demonstrated a mild convex profile with a slightly small chin. Normal overjet and overbite (2 mm and 2 mm, respectively) and a bilateral Class I canine relationship with an unidentified molar relationship were noted. The lower dental midline coincided with the facial midline, whereas the upper dental midline had deviated 1 mm to the right (Figure 1). Slight irregularity of alignment and a moderate curve of Spee were found in the mandibular arch. Eight teeth of #16, 12, 11, 22, 26, 35, 36 and 46 were extracted because of severe periodontal tissue loss, which left approximately 17 mm of space in the lower left side, 11 mm in the lower right side, and 6 mm in the upper right side, into which the second molars were mesially tipped. Severe alveolar atrophy was seen in all the edentulous spaces (Figure 2). A 5-mm probing pocket depth with severe mobility of the mandibular right second premolar was found in the initial periodontal examination.
The panoramic radiograph showed that the remaining teeth had moderate to severe periodontal bone loss. The four third molars were embedded in the bone with a normal shape. The floor of the maxillary sinus on both sides was above the roots of the posterior teeth. The patient showed an asymptomatic temporomandibular joint with normal joint contours.
The lateral cephalometric tracing and analysis showed a skeletal Class II relationship (ANB, 7.8°) with a normally positioned maxilla (SNA, 79.2°), a backward-positioned mandible (SNB, 71.5°), a hyperdivergent growth pattern (SN-MP, 44.2°), retroclined maxillary incisors, and proclined mandibular incisors (U1-SN, 95.4°; IMPA, 94.1°). The soft-tissue analysis showed a retroclined mental (Z-angle, 63.8°) (Figure 3 and Table 1). Description of the variables used in this study are depicted in Table 1.
The treatment objectives for this patient were to (1) align the teeth and assign the space of the missing teeth (#11, 12, 21) for the implant, (2) close the remaining posterior spaces in the maxillary arch and in the mandibular arch, (3) level the curve of Spee, and (4) maintain normal overjet and overbite and Class I canine relationships.
In the mandibular arch, the alternative approach was to upright the second molars. Implant-based prosthodontics would be a practical approach to solve the problem of the missing first molars. The third molars may not have enough space to erupt so that they might have to be removed. Nevertheless, the patient refused to undergo the necessary alveolar augmentation and preferred to reduce the possible surgical procedures and costs. The possibility of using a removable partial denture for restoration of the lower missing teeth was also discussed with the patient, however the patient disliked the prospect of frequently removing the dentures.
Therefore, the patient chose to undergo mesial movement of the mandibular second and third molars to close the missing spaces. The patient was made aware of all the possible adverse effects and complications and was also explained that a long-term effort would be required to achieve the treatment objectives and that the treatment might not be completely successful. Informed consent was obtained from the patient for publishing the case details and images.
A standard periodontal treatment was performed before orthodontic treatment, and regular periodontal check-ups were carried out throughout the orthodontic treatment. And 0.022 × 0.028-inch (in) slot preadjusted brackets with an MBT prescription (Protect, Hangzhou, China) were bonded on all teeth.
In the maxillary arch, leveling and alignment were initiated using a 0.012-in nickel-titanium archwire and then gradually increased to 0.019 × 0.025-in nickel-titanium. Space closure was performed using slide mechanics on a 0.019 × 0.025-in nickel-titanium archwire with an accentuated curve.
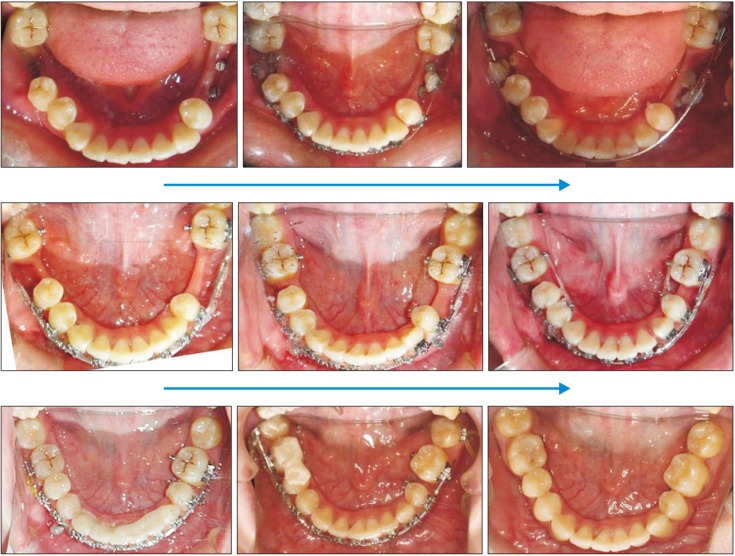
In the mandibular arch, it was very difficult to level and align the second molars by sequential nickel-titanium archwires from the left second molar to the right second molar due to the wide missing space. The archwire over the long gap would easily slip out of the buccal tubes under normal occlusal force. To support the archwires over the long missing space, a “fulcrum” was created at the virtual crown of the first molar. Briefly, in the left edentulous alveolar ridge, two long miniscrews (2.0 mm in diameter, 13-mm length; Cibai, Ningbo, China) were connected by two pieces of 0.019 × 0.025-in stainless steel and flowable light-cured resin to form the “fulcrum.” In the right missing area, one long miniscrew was placed in the severely atrophic edentulous alveolar ridge and two miniscrews (diameter, 1.6 mm; length, 9 mm) were inserted in the interradicular septa between the canine and the second premolars connected by a 0.019 × 0.025-in stainless steel wire and light-cured resin to form the “fulcrum” (Figure 4).
After the mandibular second molars were uprighted, a topical 0.016 × 0.022-in stainless steel sectional archwire in an “L” shape with tip-backs of 20 to 30o and a toe-in bend of 15o was then activated to protract the second molar at the rate of 0.5 mm at each appointment (Figure 5).
When the second molars contacted the “fulcrum” or the miniscrew, all the miniscrews were removed, except the miniscrew in the interradicular septa between the mandibular right canine and the first premolar. Additionally, a miniscrew (diameter, 1.6 mm; length, 9.0 mm) was inserted into the interradicular septa between the mandibular left canine and the first premolar to provide absolute anchorage. The space was closed along a long 0.016 × 0.022-in stainless steel archwire with an “L” loop. A power chain was applied from the miniscrew to the second molars applying approximately 50 cN of force (Figure 6).
The patient came to the office every month to have the chain changed. The treatment took approximately 29 months. During this period, serial panoramic radiographs were obtained to evaluate movement of the second and third molars (Figure 7). After 39 months of active treatment, debonding was performed. Three maxillary incisors (#11, 12, 22) were restored by implants. A clear retainer was given to the patient, and a one-year follow-up appointment was suggested.
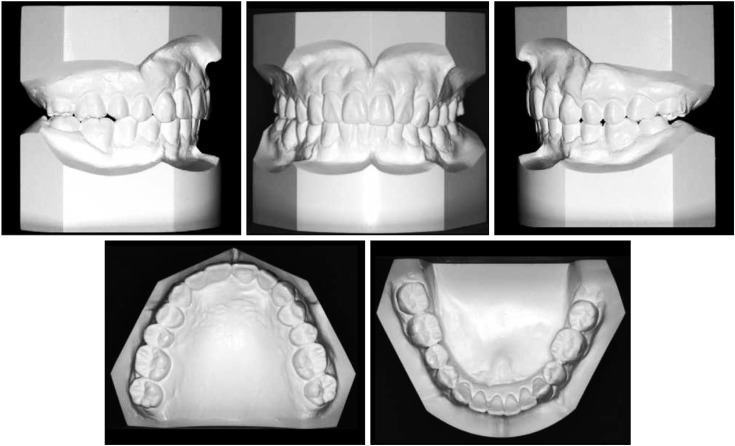
The patient maintained healthy periodontal tissues during the treatment. After 39 months of active orthodontic treatment, the posttreatment records demonstrated Class I molar (right) and Class III (left) molar relationships and bilateral Class I canine relationships, in addition to good overjet and overbite, although the 1-mm deviation of the dental midline remained (Figures 3, 8, and 9). A harmonious facial balance was achieved (Figures 3 and 8).
The posttreatment panoramic radiograph showed that good root parallelism was obtained at the end of orthodontic treatment. The upper left 7-mm space was closed by successful mesial movement of the maxillary second and third molars; the lower right and left space of 11 mm and 17 mm, respectively, were closed by mesial movement of the mandibular second and third molars (Figures 7 and 10). No obvious root resorption was observed on the posttreatment panoramic radiograph. The alveolar bone in the atrophic edentulous ridge was improved to almost normal levels. A 3-mm probing pocket depth with minor mobility of the mandibular right second premolar was noted on periodontal examination. After debonding, gingival recession was seen in the mesial aspect of the mandibular second molars, which was clinically acceptable (Figure 8). Consultation with the patient's periodontist to improve gingival recession was suggested. Probing depths of 2.0 to 3.0 mm were detected around the mandibular right second and third molars.
Complete closure of the atrophic edentulous space by bodily movement of the second and third molars without tipping was successfully achieved, and more importantly, a significant increase in ridge height was seen. In this patient, the compromised periodontium, severe tipping of the second molars, and the long span of missing tooth spaces made the initial alignment and leveling in the mandibular arch very difficult. The bone quantity available for a direct anchorage screw was very limited. To overcome these problems, we created virtual “first molars” with connected miniscrews to act as a “fulcrum” to upright and align the second molars.
The threshold value of three-dimensional bone volumes for successful protraction of the second molar to close the mandibular first molar space had been initially thought to be 7 mm for buccolingual length and 6 mm for mesiodistal width.7 Recently, several authors have reported that mandibular spaces larger than 7 mm (from 8 to 12 mm) can be closed by protracting posterior teeth.18 It had also been believed that the decreased bone support will compromise molars that were protracted into an atrophic edentulous space. However, an increasing number of case reports have shown that this may not be the case.38 The thin resorbed edentulous alveolar ridge width will increase because of the protracted molars. In the case presented by Nagaraj et al.,8 alveolar ridge width and height increased. In our case, the mesiodistal extraction spaces were 11 mm on the right side and 17 mm on the left side. After treatment, the alveolar bone height and width increased although gingival recession was noticed on the mesial aspect of the second lower molars.
It has been well established that mechanotransduction of mechanical stress leads to osteogenic differentiation of the stem cells in the periodontal ligament91011 and that teeth can be moved by the action of osteoclasts induced in the pressure side and osteoblasts induced in the strain side.12 Healthy periodontal ligaments that may have large amounts of healthy periodontal stem cells are crucial to bodily tooth movement.13 Therefore, careful clinical monitoring and good periodontal plaque control throughout the orthodontic treatment are needed. In terms of periodontal regenerative ability, initiation of treatment at a younger age may be advantageous.5 Fortunately, our patient was only 19 years old, and the regenerative ability of the periodontal ligament was strong, which contributed to the successful bodily movement of the second molars.
Initial leveling and aligning of the arch are predominantly practiced in orthodontics. With the advent of the miniscrew, almost all forms of tooth movements such as intrusion, extrusion, retraction, protraction, and expansion can be easily achieved with direct or indirect anchorage using miniscrews.
Light forces or a force system and movement at low speeds were required throughout tooth movement. It is important to avoid heavy forces to prevent any hyalinization, which can cause unwanted indirect resorption without apposition.41415 When teeth are moved under heavy forces, resorption and apposition become unbalanced and no adequate bone regeneration in the direction of the tooth movement may be achieved.12 External apical root resorption (EARR) and alveolar bone loss, which are correlated with tooth movement under heavy forces should also be taken into consideration during protraction of the molars.5 In Kim et al.' study,5 average root length decreased significantly by 0.8 mm and EARR greater than 2 mm occurred in only 4.0% of the molars. Although root movement was at least 11 mm, EARR was not obvious in our case, partially due to the patient's young age. In our case, the alveolar bone height and width increased as those reported by Nagaraj et al.8 However, alveolar bone height loss of more than 2 mm was evident in 2% of the molars in Kim et al.'s study. The increased gingival recession seen in our case may be due to the severely atrophic alveolar ridge.
Additionally, the proper moment-to-force ratio is important for bodily protraction of the second molar.14 A high moment-to-force ratio was important to achieve bodily movement of the teeth.414 Kulhberg and Burstone16 demonstrated that central positioning of a T-loop produces equal and opposite moments, while an off-centered T-loop produces differential moments. An increased beta moment was generated by more posterior positioning and an increased alpha moment generated by more anterior positioning. Other modified loops, such as the helical loop, L loop, and reversed curve, also had similar force mechanics. On the basis of this reasoning, in our case, light continuous forces with a stainless steel archwire with “L” loops or a reversed curve were applied to allow distal crown moment and mesial root moment of the mandibular second molars. However, measurement of the force levels and moment-to-force ratios accurately at each adjustment is unpractical.12
In our patient, large lower posterior extraction spaces were closed by mesial movement of the second and third molars through a severely atrophic alveolar ridge without noticeable complications. The clinician and the patient should bear in mind the advantages and disadvantages of this approach when deciding on a treatment option.
ACKNOWLEDGEMENTS
The authors would like to thank Dr. Li hong Lei for her support during the diagnostic procedures.
Notes
References
1. Baik UB, Chun YS, Jung MH, Sugawara J. Protraction of mandibular second and third molars into missing first molar spaces for a patient with an anterior open bite and anterior spacing. Am J Orthod Dentofacial Orthop. 2012; 141:783–795. PMID: 22640680.

2. Roberts WE. Bone physiology, metabolism and biomechanics in orthodontic practice. In : Graber TM, Vanarsdall RL, editors. Orthodontics: current principles and techniques. St Louis: Mosby;1994.
3. Baik UB, Kim MR, Yoon KH, Kook YA, Park JH. Orthodontic uprighting of a horizontally impacted third molar and protraction of mandibular second and third molars into the missing first molar space for a patient with posterior crossbites. Am J Orthod Dentofacial Orthop. 2017; 151:572–582. PMID: 28257742.

4. Cacciafesta V, Melsen B. Mesial bodily movement of maxillary and mandibular molars with segmented mechanics. Clin Orthod Res. 2001; 4:182–188. PMID: 11553103.

5. Kim SJ, Sung EH, Kim JW, Baik HS, Lee KJ. Mandibular molar protraction as an alternative treatment for edentulous spaces: focus on changes in root length and alveolar bone height. J Am Dent Assoc. 2015; 146:820–829. PMID: 26514887.
6. Saga AY, Maruo IT, Maruo H, Guariza Filho O, Camargo ES, Tanaka OM. Treatment of an adult with several missing teeth and atrophic old mandibular first molar extraction sites. Am J Orthod Dentofacial Orthop. 2011; 140:869–878. PMID: 22133953.

7. Hom BM, Turley PK. The effects of space closure of the mandibular first molar area in adults. Am J Orthod. 1984; 85:457–469. PMID: 6587780.

8. Nagaraj K, Upadhyay M, Yadav S. Titanium screw anchorage for protraction of mandibular second molars into first molar extraction sites. Am J Orthod Dentofacial Orthop. 2008; 134:583–591. PMID: 18929277.

9. Kim HJ, Choi YS, Jeong MJ, Kim BO, Lim SH, Kim DK, et al. Expression of UNCL during development of periodontal tissue and response of periodontal ligament fibroblasts to mechanical stress in vivo and in vitro. Cell Tissue Res. 2007; 327:25–31. PMID: 17004066.

10. Bolcato-Bellemin AL, Elkaim R, Abehsera A, Fausser JL, Haikel Y, Tenenbaum H. Expression of mRNAs encoding for alpha and beta integrin subunits, MMPs, and TIMPs in stretched human periodontal ligament and gingival fibroblasts. J Dent Res. 2000; 79:1712–1716. PMID: 11023268.
11. Basdra EK, Papavassiliou AG, Huber LA. Rab and rho GTPases are involved in specific response of periodontal ligament fibroblasts to mechanical stretching. Biochim Biophys Acta. 1995; 1268:209–213. PMID: 7662710.

12. Oh H, Herchold K, Hannon S, Heetland K, Ashraf G, Nguyen V, et al. Orthodontic tooth movement through the maxillary sinus in an adult with multiple missing teeth. Am J Orthod Dentofacial Orthop. 2014; 146:493–505. PMID: 25263152.

13. Kessler M. Interrelationships between orthodontics and periodontics. Am J Orthod. 1976; 70:154–172. PMID: 1066052.

14. Melsen B. Biological reaction of alveolar bone to orthodontic tooth movement. Angle Orthod. 1999; 69:151–158. PMID: 10227556.
15. Giancotti A, Greco M, Mampieri G, Arcuri C. The use of titanium miniscrews for molar protraction in extraction treatment. Prog Orthod. 2004; 5:236–247. PMID: 15546014.
16. Kuhlberg AJ, Burstone CJ. T-loop position and anchorage control. Am J Orthod Dentofacial Orthop. 1997; 112:12–18. PMID: 9228836.

Figure 3
Lateral cephalogram, tracing, and superimpositions. A, Immediately after attaching the orthodontic appliances; B, posttreatment; C, one-year posttreatment; D, superimposition on sella-nasion plane at sella; E, on palatal plane at anterior nasal spine and on mandibular plane at menton.
Black, Immediately after attaching the orthodontic appliances; red, posttreatment; green, 1-year follow-up.
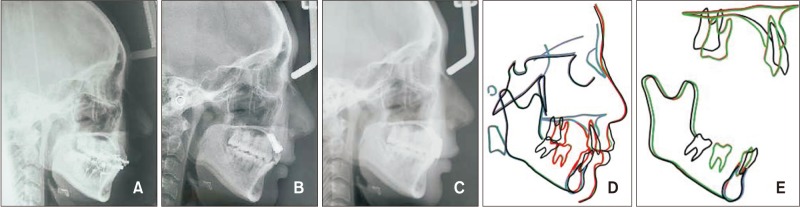
Figure 4
“Fulcrums” at the virtual position of the mandibular first molar composed of stainless steel wire, bracket, and resin on the base of miniscrews. A, Right fulcrums; B, left fulcrums; C, panoramic radiograph.
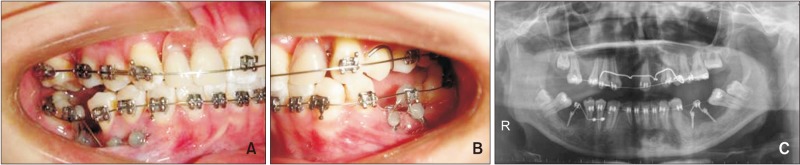
Figure 5
A photo showing progress of 6 months into treatment and a diagram of the applied mechanics of mandibular second molar uprighting and protraction.
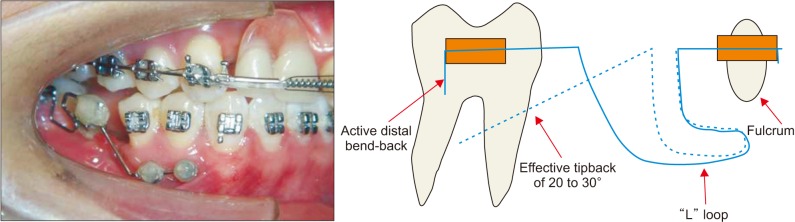
Figure 6
Photos showing progress at 17 months into treatment. Miniscrews were used in the mandibular arch to provide maximum anchorage.

Figure 7
Serial panoramic photograph showing protraction of the mandibular second molars.
0M, 0 month; 4M, 4 months; 7M, 7 months; 13M, 13 months; 25M, 25 months; 29M, 29 months; 39M, 39 months; 51M, 51 months.
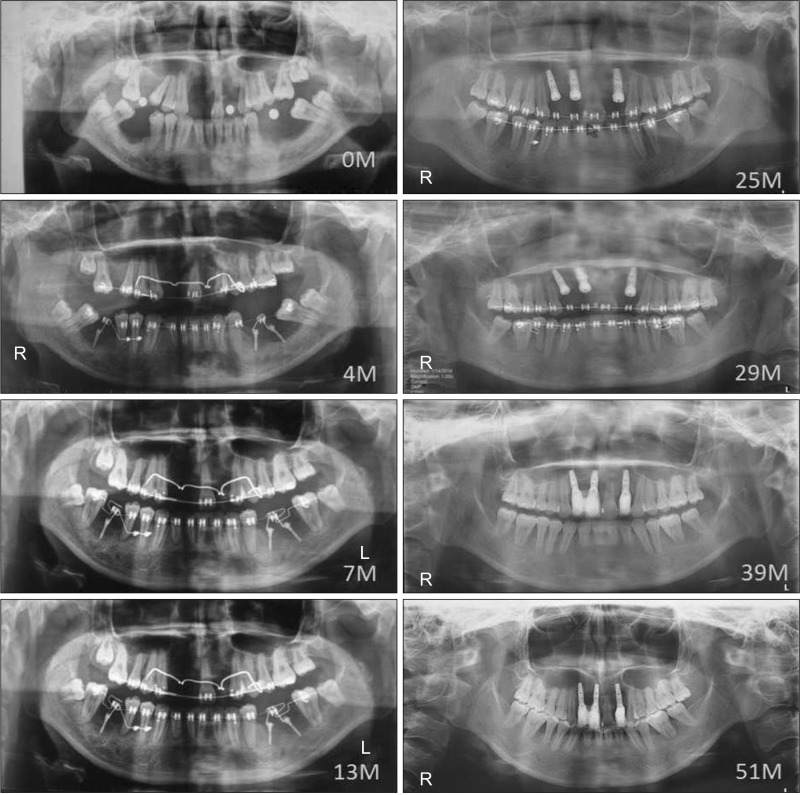
Table 1
Cephalometric measurements
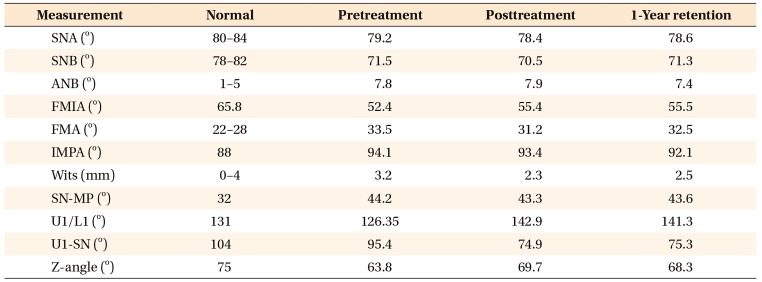
SNA, Sella-nasion-A point; SNB, sella-nasion-B point; ANB, A point-nasion-B point; FMIA, mandibular incisor to Frankfurt horizontal (FH) line angle; FMA, FH line to mandibular plane angle; IMPA, mandibular incisor to mandibular plane angle; Wits, distance between points of contact of perpendiculars dropped for point A and B onto occlusal plane; SN-MP, sella-nasion-mandibular plane angle; U1/L1, upper incisor to lower incisor angle; U1 to SN, upper incisor to sella-nasion plane angle; Z-angle, soft pogonion-lower lip-FH line.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download