This article has been
cited by other articles in ScienceCentral.
Abstract
Hemifacial microsomia (HFM) patients may experience emotional withdrawal during their growth period due to their abnormal facial appearance. Distraction osteogenesis at an early age to improve their appearance can encourage these patients. Some abnormalities of the affected side can be overcome by distraction osteogenesis at an early age. However, differences in the growth rate between the affected and unaffected sides during the rest of the growth period are inevitable due to the characteristics of HFM. Therefore, re-evaluation should be performed after completion of growth in order to achieve stable occlusion through either orthognathic surgery or camouflage orthodontic treatment. An eight-year-old patient visited the clinic exhibiting features of HFM with slight mandibular involvement. He received phase I treatment with distraction osteogenesis and a functional appliance. Distraction osteogenesis was performed at the right ramus, which resulted in an open bite at the right posterior dentition. After distraction osteogenesis, a functional appliance and partial fixed appliance were used to achieve extrusion of the affected posterior dentition and settlement of the occlusion adjustment on the unaffected posterior dentition. The patient visited the clinic regularly for follow-up assessments, and at the age of 20 years, he showed facial asymmetry of the mandible, which had deviated to the right side. He received orthodontic treatment to improve the occlusion of his posterior dentition after the growth period. Without orthognathic surgery, stable occlusion and a satisfactory facial appearance were obtained through camouflage orthodontic treatment.
Go to :

Keywords: Hemifacial microsomia, Distraction osteogenesis
INTRODUCTION
Hemifacial microsomia (HFM) is the second most common craniofacial disorder after cleft lip and palate. HFM presents as a deformity of the craniofacial part by the first and second branchial arches at the sixth week of fetal life. Although various factors are known to influence these deformities, such as bleeding at the stapedial artery and teratogens like retinoic acid and primidone, the exact cause of HFM is unknown.
1 The incidence of HFM has been reported to vary from one in 3,500 to one in 5,600. Moreover, the condition manifests more frequently in male patients (male:female, 3:2) and in the right side (right side:left side, 3:2).
2 The clinical features of HFM involves the mandible, maxilla, orbit, ear, cranial nerves, and facial soft tissues.
3 In 1969, Pruzansky classified HFM into three types based on the mandibular deformity, and Kaban et al.
4 modified the classification system. Prada Madrid et al.
5 suggested distraction osteogenesis and the use of an autogenous bone graft from the ilium and rib for patients in their growth period. Mielnik-Błaszczak and Olszewska
6 suggested distraction osteogenesis or autogenous bone graft for young HFM patients in their growth period, and orthognathic surgery or bimaxillary distraction osteogenesis in adult patients.
Distraction osteogenesis, which has several advantages such as increasing the volume of the soft tissue as well as skeletal change
7 to correct the asymmetry in growing HFM patients, has been described in several publications. However, continued asymmetrical growth pattern during the residual growth period
8 makes it difficult to predict the final skeletal relationship and occlusion. Thus, to ensure appropriate orthodontic treatment and/or orthognathic surgery, it is necessary to observe and reassess the case after the growth period is complete.
In this case, distraction osteogenesis was performed on an 8-year-old male HFM patient. After distraction osteogenesis, the asymmetrical growth of the mandible progressed during the growing period. However, after completion of growth, stable occlusion was established only by camouflage treatment without orthognathic surgery.
Go to :

DIAGNOSIS AND ETIOLOGY
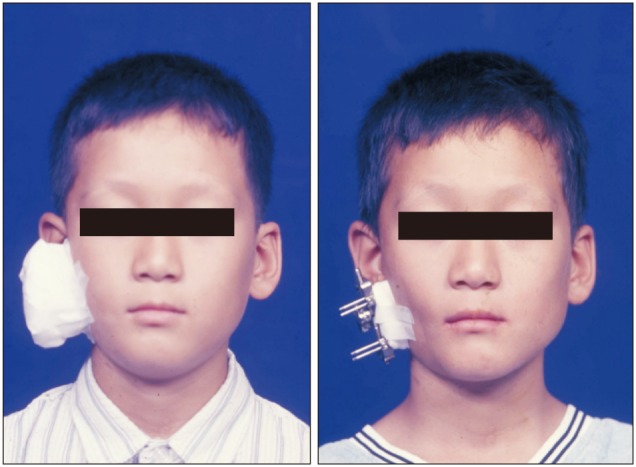
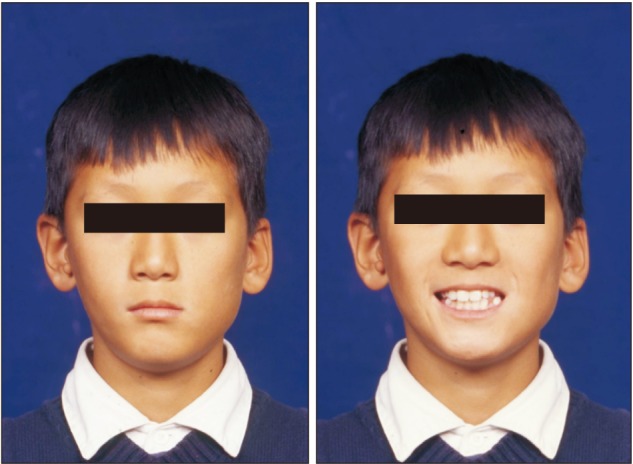
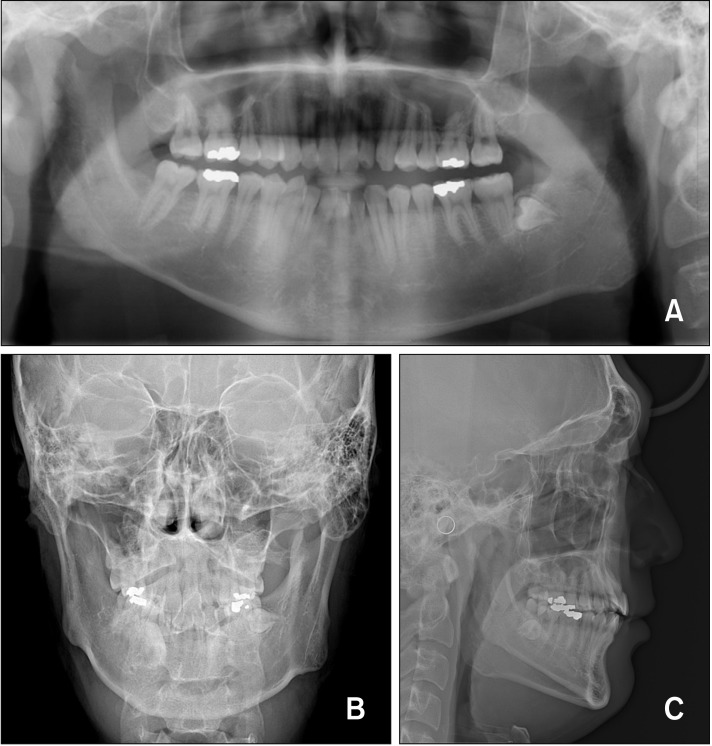
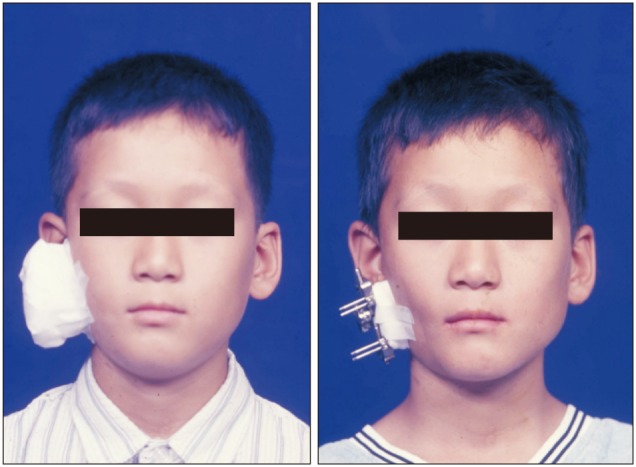
Written informed consent was obtained from the patient for publication of this case report with images. An 8-year-old male patient visited the clinic due to facial asymmetry. The extraoral examination showed a soft tissue tag at the right preauricular region and mandibular deviation to the right (
Figure 1). In contrast, the intraoral examination showed Angle's Class I molar relationship on the right side and Angle's Class II relationship on the left side. The patient showed mild crowding at the lower anterior dentition and open bite at the left anterior dentition. The upper left lateral incisors were pegshaped (
Figure 2).
 | Figure 1First phase pretreatment facial photographs.
|
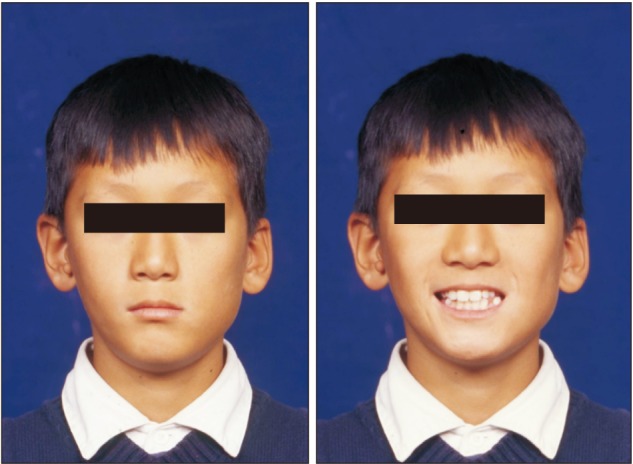
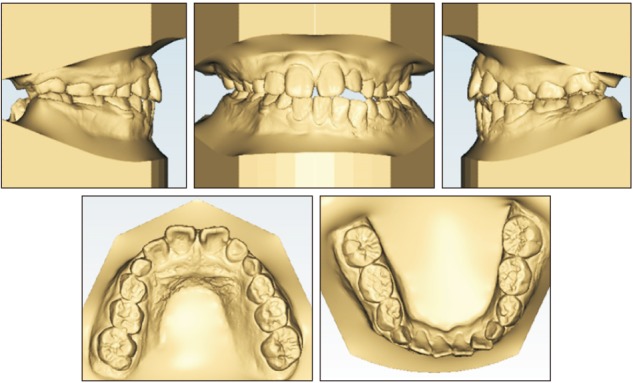 | Figure 2First phase pretreatment 3-dimensional dental models.
|
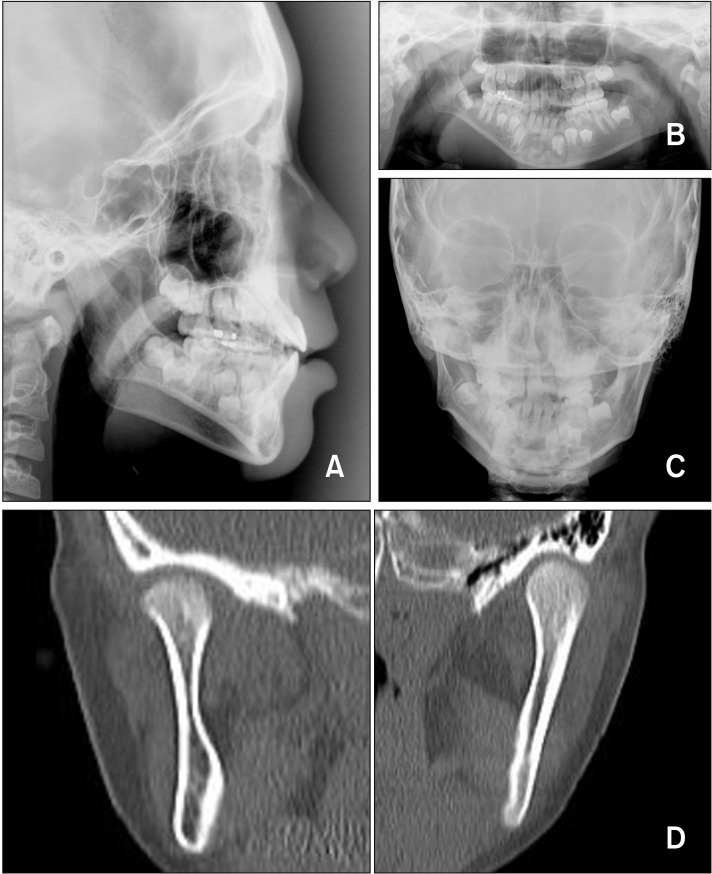
The patient showed a hyperdivergent growth pattern, and his anteroposterior skeletal discrepancy was within the normal range (
Table 1 and
Figure 3A). Panoramic radiographs showed that the vertical height of the right ramus was significantly shorter than that on of the left side (
Figure 3B). The posteroanterior cephalometric view showed a 4-mm left downward canting at the maxillary posterior dentition, but the vertical difference between the left and right jugular points was within the normal range. The vertical distance from the jugular point to the antegonial notch of the right side and left side showed a difference of 13 mm (
Figure 3C). In the computed tomography view, the shape and position of the mandibular condyle to the glenoid fossa were relatively good (
Figure 3D). A deviation to the right was observed at mouth opening, but no limitation of mouth opening movement was observed. In summary, the patient had HFM and showed normal facial features, except in the mandible. He was diagnosed with Type IIA HFM according to the classification system proposed by Pruzansky and Kaban et al.
4
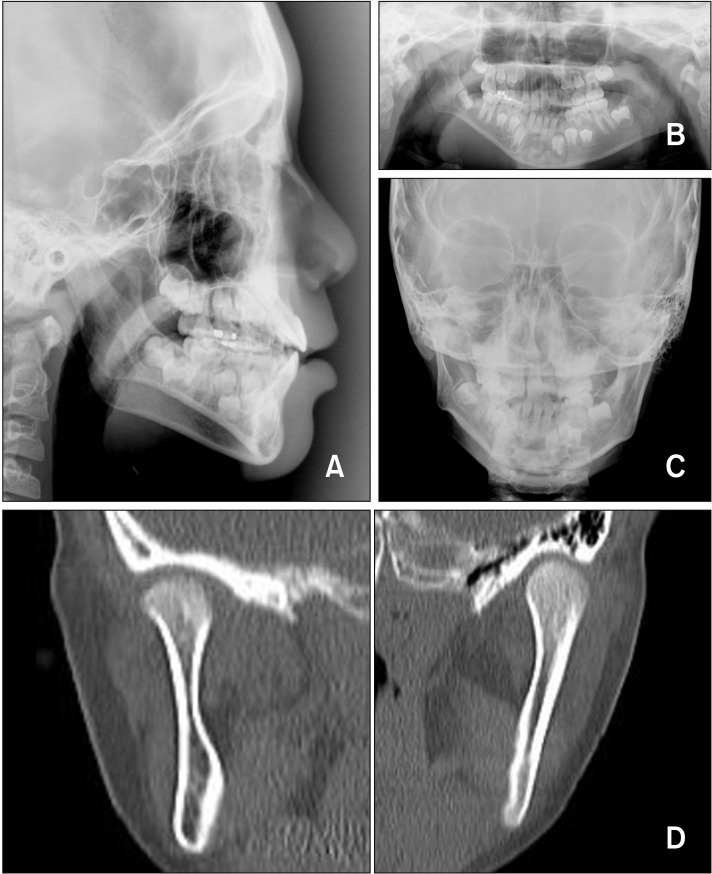 | Figure 3First phase pretreatment. A, Lateral cephalogram; B, panoramic radiograph; C, posteroanterior cephalogram; D, computed tomography image.
|
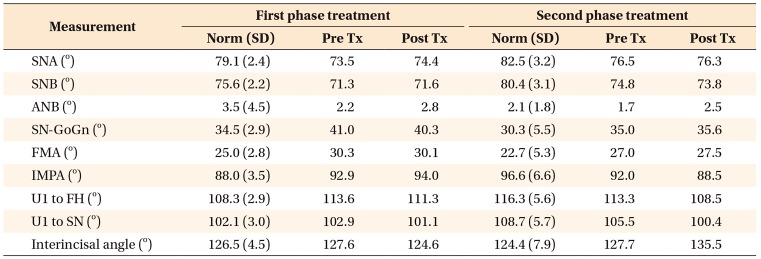
Table 1
Cephalometric summary
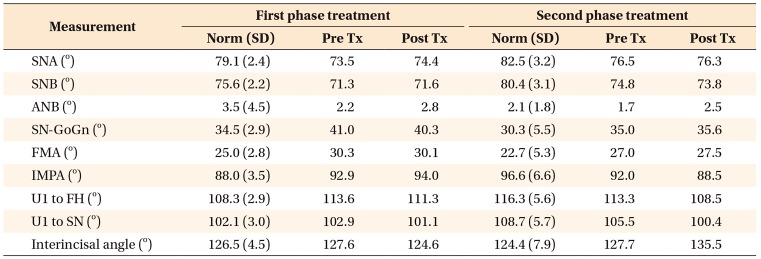

Go to :

TREATMENT OBJECTIVES
The treatment objectives were as follows: to increase the vertical height of the right ramus through distraction osteogenesis to improve severe asymmetry of the mandible, and to promote extrusion of right posterior dentition by using a functional appliance.
Go to :

TREATMENT ALTERNATIVES
The treatment of patients with HFM is complicated and a long-term process because of the congenital growth potential difference between the two sides of the mandible. Therefore, co-operation among various departments from the medical and dental fields is essential. Patients with facial asymmetry need occlusal plane correction and surgical intervention to lengthen the mandibular ramus and/or corpus depending on the affected area.
Treatment options are as follows: 1) Orthopedic management, 2) distraction osteogenesis + orthopedic management, 3) iliac or costochondral bone grafts + distraction osteogenesis, and 4) orthognathic surgery in adulthood.
The patient was classified as showing type IIA HFM according to the classification system proposed by Pruzansky and Kaban et al.,
4 wherein his right mandible had a hypoplastic and malformed condyle. His joint function remained normal. However, he exhibited severe facial asymmetry. His right ramus and the vertical height of the posterior dentition were short, which needed substantial extrusion. To achieve this treatment goal, we decided to use distraction osteogenesis and a functional appliance. After phase I treatment, orthodontic treatment and reassessment for orthognathic surgery were planned after completion of the patient's growth period.
Go to :

TREATMENT PROGRESS
During the surgical procedure, osteotomy was performed on the ramus parallel to the occlusal plane, and the extraoral distraction device was placed vertical to the osteotomy line. In the frontal view, the distraction device was placed along the slope of the ramus, which showed an inclination of 71.5° to the horizontal plane.
After a 5-day lag period, the device was activated 1 mm daily. The 0.5 mm activation was performed twice a day, but if there was pain, 0.25 mm of activation was performed four times a day. Total activation was 19.5 mm (
Figure 4). At the end of distraction activation, the right antegonial notch, which was previously 12 mm above, was relocated 6 mm below to the left antegonial notch. The menton, which had deviated to the right, was over-corrected to the left after the distraction, and the facial asymmetry was greatly improved (
Figure 5). The vertical bite opening of the right first molar was about 10 mm while that of the left side did not change significantly.
 | Figure 4Panoramic radiograph obtained after termination of activation.
|
 | Figure 5Facial photographs obtained before and after activation.
|
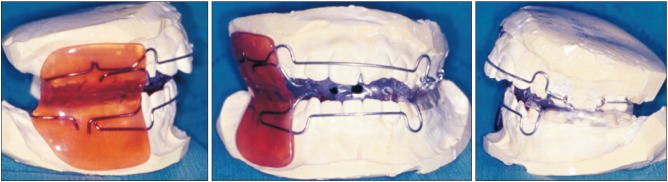
After distraction, a functional appliance containing a posterior bite block on the left side was used to allow extrusion of right posterior teeth and to promote settlement of the occlusion for the 2-month consolidation period (
Figure 6). After the consolidation period, a unilateral bite block appliance was attached with glass ionomer cement on the lower left posterior teeth, a partial fixed appliance was directly bonded to the right posterior teeth, and extrusion of the posterior teeth was performed by using vertical elastic (
Figure 7). Settlement of occlusion was continued for 6 months. Phase I treatment was terminated after 8 months, and the changes induced by growth were monitored (
Figures 8 and
9).
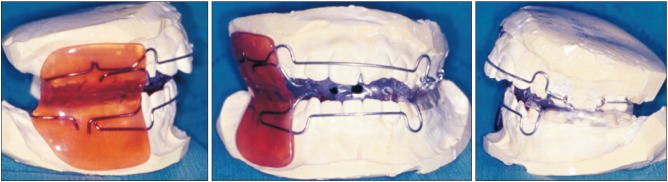 | Figure 6Functional appliance used after distraction, containing a unilateral posterior bite block on the left side to allow extrusion of the right posterior teeth.
|
 | Figure 7Partial fixed appliance and vertical elastics used to extrude of the right posterior teeth after consolidation period. A bite block was bonded with glass ionomer cement on the lower left posterior teeth.
|
 | Figure 8First phase posttreatment facial photographs.
|
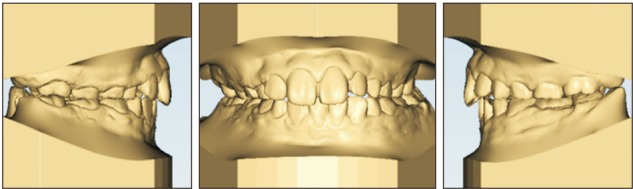 | Figure 9First phase posttreatment 3-dimensional dental models.
|
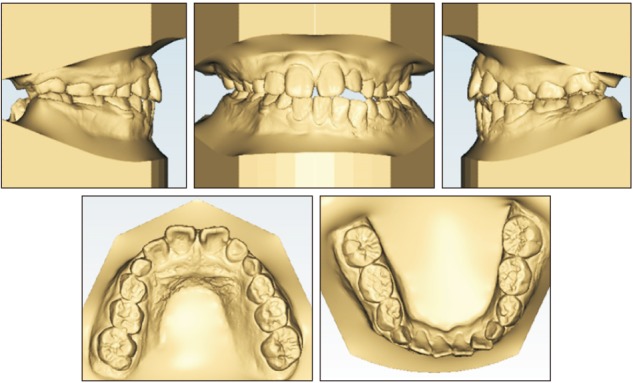
Second diagnosis and treatment plan
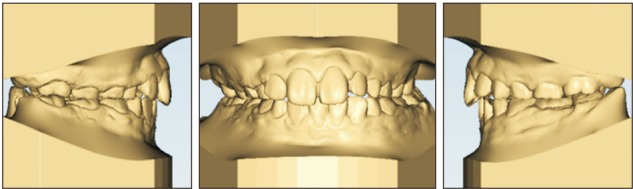
The patient regularly visited the clinic and received follow-up assessments. When he turned 20 years of age, open bite of the left posterior dentition was recognized. Both sides showed an Angle Class I molar relationship. The left posterior dentition showed poor interdigitation with slight crowding at both the upper and lower anterior dentition (
Figure 10).
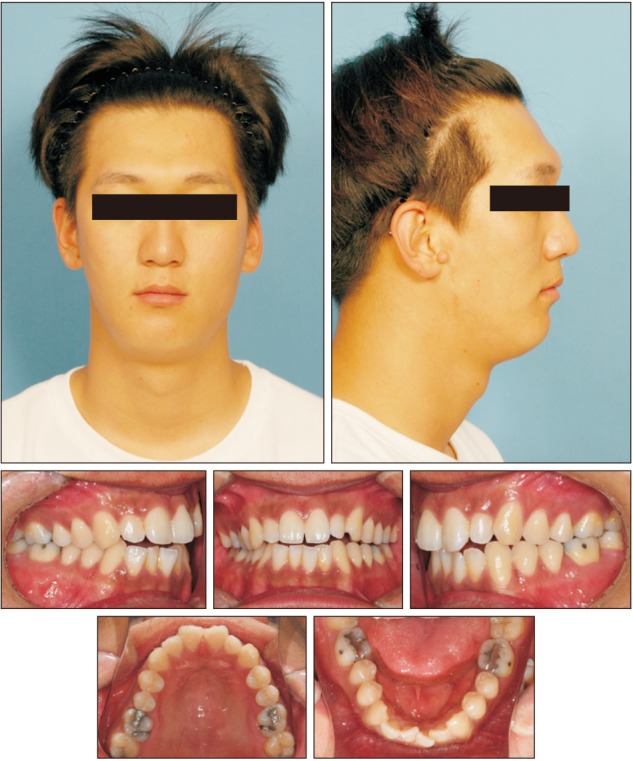 | Figure 10Second phase pretreatment facial and intraoral photographs.
|
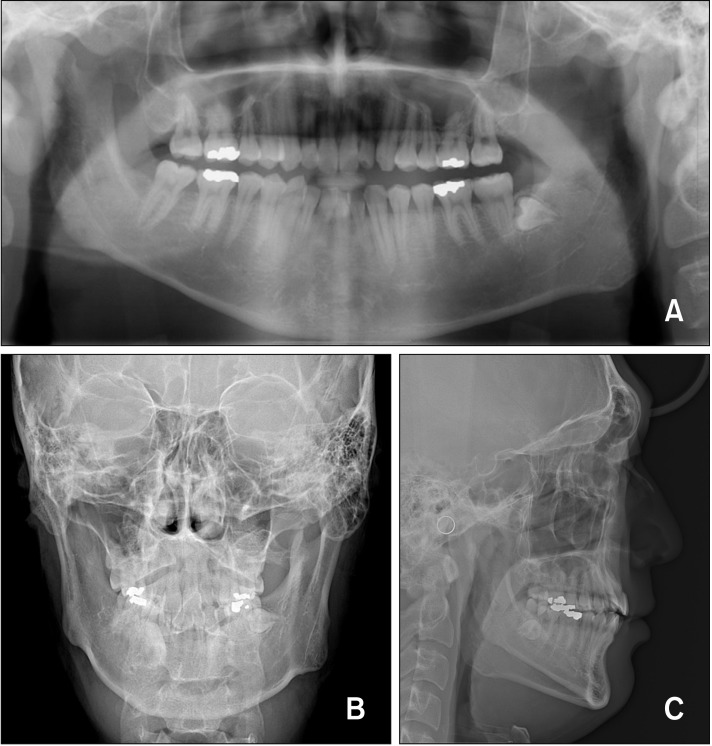
Radiographic examination showed that the heights of the left and right ramus were different and that the menton had deviated to the right side. The right antegonial notch was located 11.3 mm above the notch on the left side, and occlusal plane canting was not severe. Lateral cephalometric analysis revealed a skeletal Class I relationship, with other factors within the normal range (
Figure 11).
 | Figure 11Second phase pretreatment. A, Panoramic radiograph; B, posteroanterior cephalogram; C, lateral cephalogram.
|
The patient was diagnosed as skeletal Class I relationship with facial asymmetry caused by HFM, and comprehensive orthodontic treatment was planned without orthognathic surgery. After gaining space for alignment through expansion of both arches, occlusion was improved through the use of intermaxillary elastics.
Both dentitions were banded and bracketed using an 0.022-inch Roth prescription preadjusted brackets (Tomy Inc, Tokyo, Japan). Space was secured for alignment and leveling by using a precision lingual arch of 0.32 × 0.32-inch titanium molybdenum alloy archwire. After alignment, lateral vertical elastic was used for the stabilization of the posterior occlusion and anterior vertical elastic for the formation of overbite (
Figure 12). Consideration of the Bolton tooth ratio was necessary due to the existence of peg lateralis. For this, proper overjet was obtained through angulation control of the maxillary anterior incisor instead of stripping of the mandibular anterior teeth.
 | Figure 12Second phase treatment progress.
|
Go to :

RESULTS
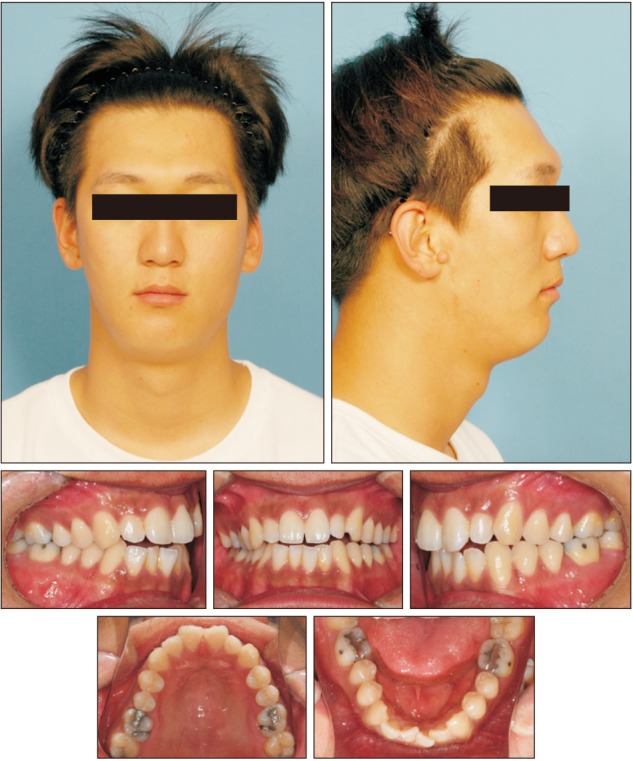
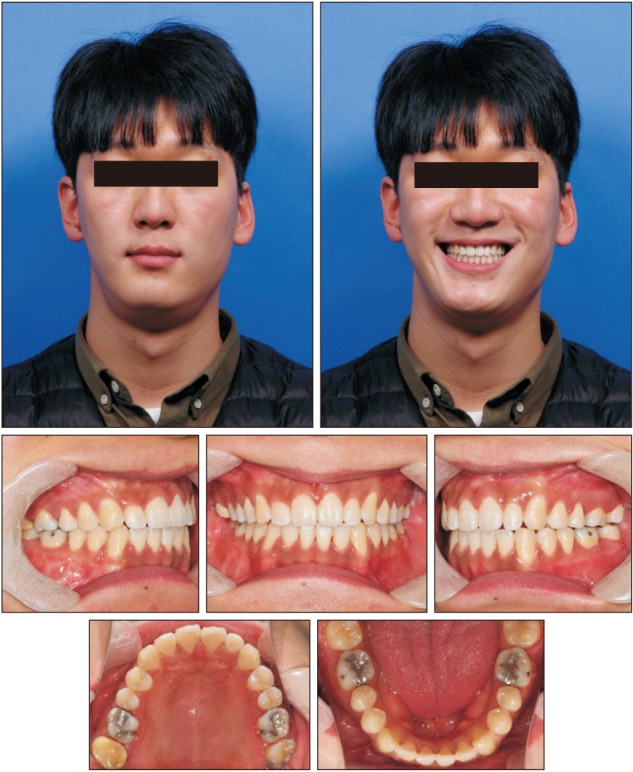
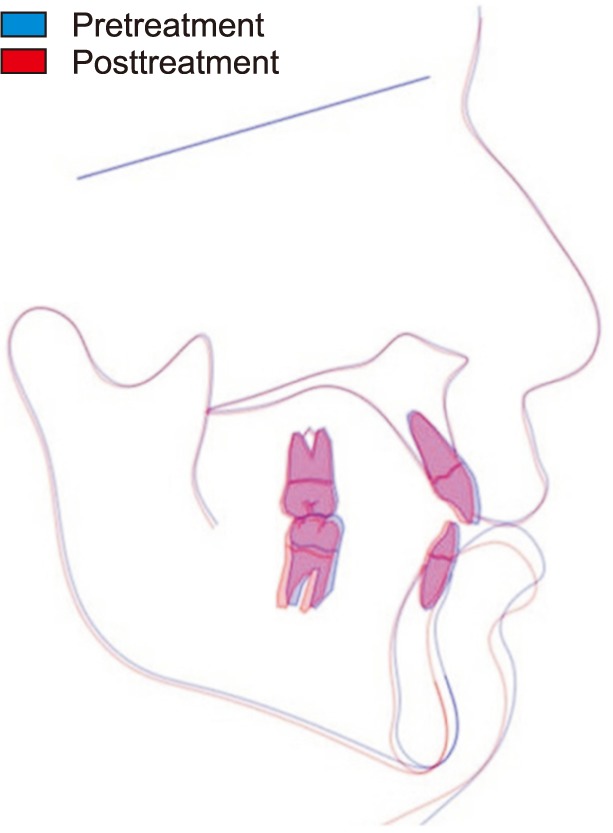
Phase II treatment of this patient lasted for total of 1 year and 7 months. The treatment was completed with Angle's Class I molar relationship and stable occlusion of the left posterior dentition. The facial asymmetry remained, but the patient had a harmonious profile with a natural smile line (
Figure 13). There was no remarkable change except for the slight clockwise rotation of the mandible based on cephalometric superimposition (
Figure 14 and
Table 1).
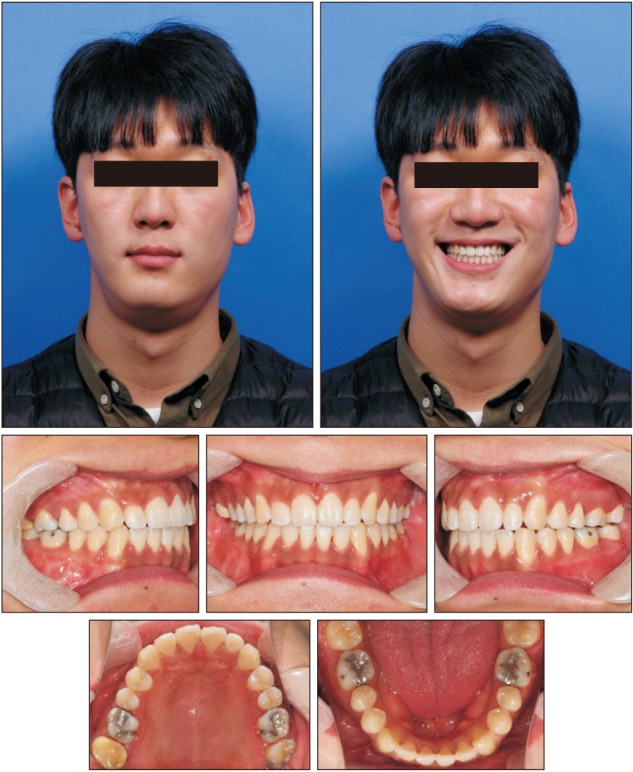 | Figure 13Second phase posttreatment facial and intraoral photographs.
|
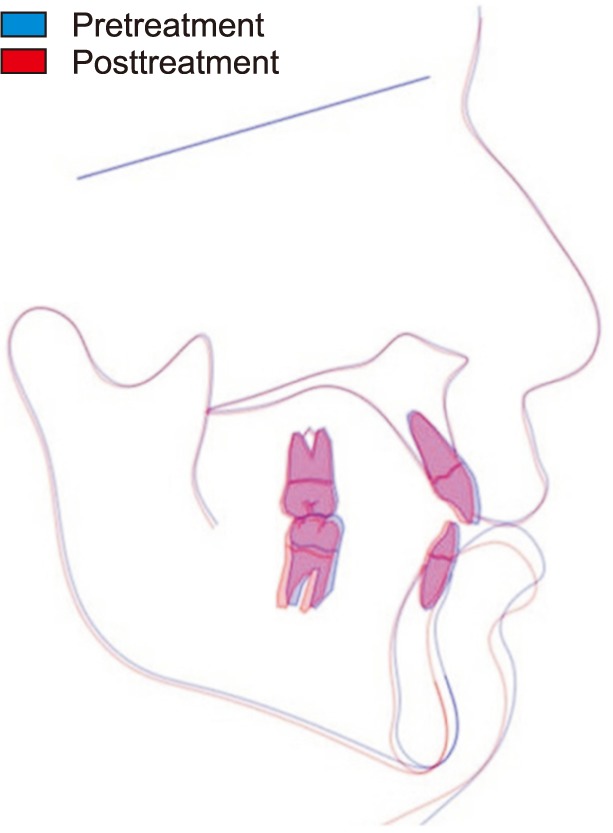 | Figure 14Superimposition of the second phase pretreatment (blue) and posttreatment (red) lateral cephalometric tracings.
|
Go to :

DISCUSSION
Kaban et al.
4 classified HFM into three types based on the degree of deformity by modifying the Pruzansky classification. In type I, all temporomandibular joint components are present and have a normal shape but are hypoplastic to various degrees. In this type, the glenoid fossa has a normal shape and the masticatory muscles are normally developed. Type II involves a functional temporomandibular joint, but the forms of the condylar head and glenoid fossa are abnormal. In type IIA, the temporomandibular joint, condylar head, and glenoid fossa are hypoplastic, deformed, and malpositioned. However, the malpositioning is not severe, allowing symmetrical mouth opening movement of the mandible. In type IIB, the mandibular ramus is hypoplastic and markedly abnormal in form and location. As a result, the temporomandibular joint does not function properly. In Type III, the mandibular ramus, condyle, and temporomandibular joint are absent and the masticatory muscles are not attached to the mandible.
Some publications suggested that early distraction osteogenesis is needed in HFM patients with obstructive sleep apnea and severe facial asymmetry.
7 The indication for early distraction osteogenesis is not clear, but it can be helpful for the psychological welfare of young patients who might experience distress because of their abnormal appearance.
910 However, due to the nature of growth in HFM, growth differences in the contracted and non-contracted site can still occur. Therefore, reassessment for orthognathic surgery or camouflage orthodontic treatment are needed for improvement of occlusion after patient growth is complete.
In distraction osteogenesis, the position and orientation of the osteotomy line and the direction of activation have important effects on the final results, so careful evaluation and planning is essential before distraction surgery. Since the main difference between the right and the left sides of the mandible was the vertical length of the ramus and anteroposterior skeletal discrepancy was not noticeable, the osteotomy was performed at the upper level of mandibular foramen on the ramus parallel to the occlusal plane in order to increase the vertical height of the ramus. The extraoral distraction device was placed perpendicular to the osteotomy line.
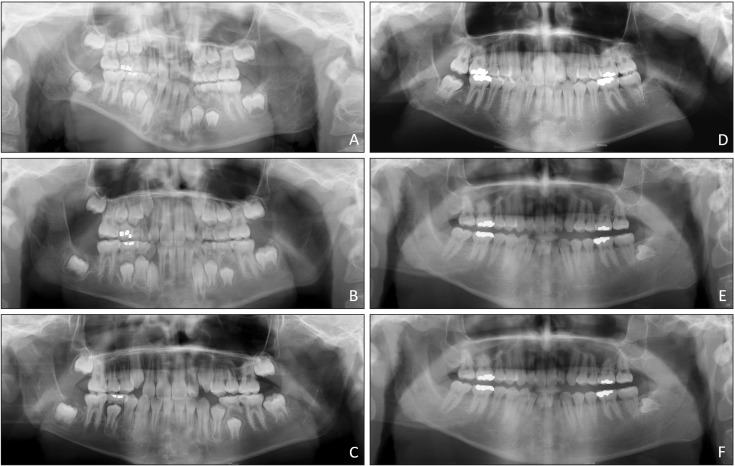
The vertical height of the ramus that showed a significant difference between the right and left sides before treatment was improved through distraction osteogenesis. However, the difference started to increase again as the patient grew up. When the locations of the antegonial notch were compared through the posteroanterior cephalogram, the difference, which was 1 mm after the first treatment at the age of 9, increased gradually and became similar to the value before treatment. Even though linear measurements in posteroanterior cephalogram are not reliable, the height change in the right and left ramus during the growth period after distraction osteogenesis showed a clear difference. Despite the asymmetry in the radiograph (
Figure 11A and 11B), it appears to be relatively symmetrical in clinical photography (
Figure 10), which is thought to be the effect of the soft tissue volume.
In assessments of the alveolar vertical height, before distraction osteogenesis, the right posterior alveolar height of the patient was severely underdeveloped, and after distraction, the posterior occlusion was opened about 10 mm vertically at the right first molar. In patients with HFM, orthodontic extrusion of the posterior teeth using a functional appliance has been generally applied after distraction osteogenesis, and in this case, functional and orthodontic appliances were used for this purpose. After the extrusion and settling of right posterior teeth, the occlusion was stabilized and the canting of the upper dentition was also improved. To evaluate the result of posterior teeth extrusion, we measured the distance from the mandibular first molar to the mandibular inferior border in panoramic radiographs. The 7.5-mm difference between right and left sides at the initial stage was improved by the orthodontic extrusion and occlusal settlement of the distraction side. The difference in the height of the alveolar bone in the mandibular molar during the growing period tended to increase gradually and became 4 mm at the age of 15 years and beyond (
Figure 15). Generally, unlike in adults, the vertical dimension is relatively well adapted in growing children, and skeletal change can be induced from alveolar vertical alteration if proper vertical height is secured.
1112 The growth rate of the affected side in HFM patients may differ from normal, but the results of vertical development of the alveolar bone obtained by orthodontic treatment after distraction osteogenesis appear to be relatively stable.
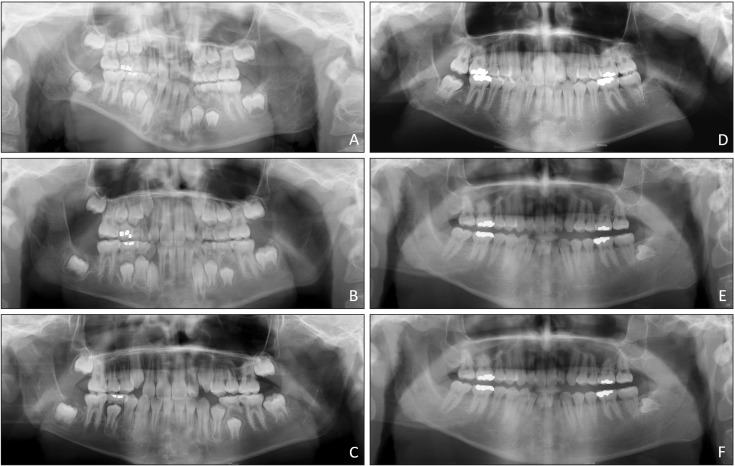 | Figure 15Panoramic radiographs from first phase to second phase treatment. A, 8 years and 11 months, before distraction osteogenesis; B, 9 years and 7 months, after distraction osteogenesis; C, 10 years and 7 months; D, 12 years and 6 months; E, 15 years and 4 months; F, 20 years and 9 months.
|
In addition, overcorrection is generally recommended for early distraction osteogenesis patients
1314 when the difference in growth between the left and right sides is likely to persist for the remaining growth period due to the characteristics of HFM.
8 This case also involved overcorrection, but special care is required because it is impossible to accurately predict the outcome of growth in children.
There was scar at the right mandibular angle due to the use of the extraoral distraction device. The scar faded gradually but it did not disappear completely. Even with the scar, the patient was satisfied with the facial appearance resulting from distraction osteogenesis during the growth period, and the treatment could be completed with simple comprehensive orthodontic treatment without orthognathic surgery in his adulthood.
Go to :

CONCLUSION
Growing HFM patients require interdisciplinary treatment. Although facial asymmetry can improved through early surgical interventions, the possibility of asymmetric growth still exists. Distraction osteogenesis can be invasive in growing HFM patients, but if the treatment is performed under appropriate case selection and with a well-designed treatment plan, sufficient advantages can be obtained. The possibility of final orthodontic treatment or orthognathic surgery cannot be disregarded in growing HFM patients. Better facial appearance during the growing period may provide better quality of life for patients. Once the patient's growth stops, the improved oral condition will provide a more acceptable environment for all dental managements.
Go to :





 PDF
PDF ePub
ePub Citation
Citation Print
Print







 XML Download
XML Download