INTRODUCTION
The craniofacial structures are physiologically connected to each other, and their coordinated growth is essential for normal craniofacial development. Growth and function of the pharyngeal airway space (PAS) are especially intimately related to the normal development of the maxillofacial structures.
1 Due to the importance of the PAS, various studies have assessed its growth and development.
2 For example, narrowed dimensions of the PAS may cause breathing difficulties. Subsequent mouth breathing due to pharyngeal obstruction may also present symptoms like an “adenoid face” or a short, retracted mandible.
The pharynx is the main anatomical structure that constitutes the PAS and is an organ composed of muscles that originate from the adjacent skeletal structures. Its size and shape are affected by the surrounding skeletal structure.
3 The nasopharynx and the oropharynx form a functional unit involved in breathing, swallowing, and pronunciation.
The dimensions of the PAS are affected by factors such as head posture, tongue position, age, body mass index (BMI),
4 as well as by alterations in mandibular position. When the mandibular position is altered, subsequent changes occur in the positions of the hyoid bone, the tongue, and the soft palate, ultimately altering the dimensions of the PAS. For example, repositioning the mandible anteriorly or posteriorly in an orthognathic surgery,
56 or using an intraoral device that advances the mandible forward,
7 may alter the dimensions of the PAS. Thus, we should consider the dimensional changes in the PAS when designing an orthodontic intraoral appliance.
Since multiple factors contribute to the dimensional changes in the PAS, it is difficult to properly predict the changes exclusively affected by mandibular displacement. Thus, in order to eliminate other undesired factors affecting the PAS, the data must be taken at the same time and posture, only making modifications in the mandibular position. Previous studies,
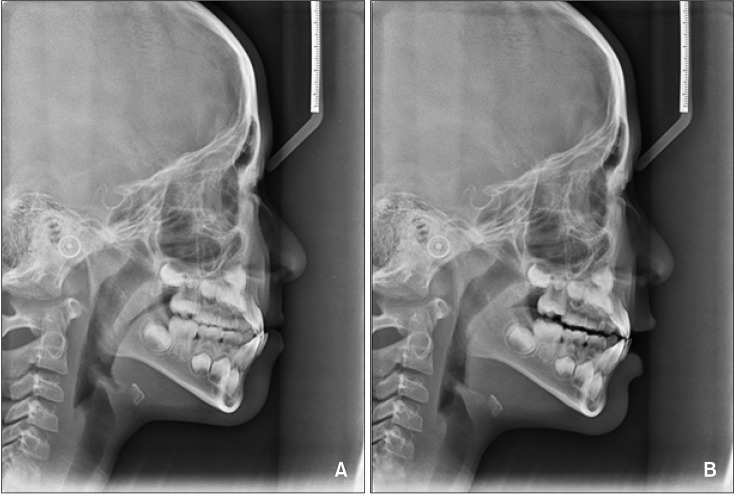
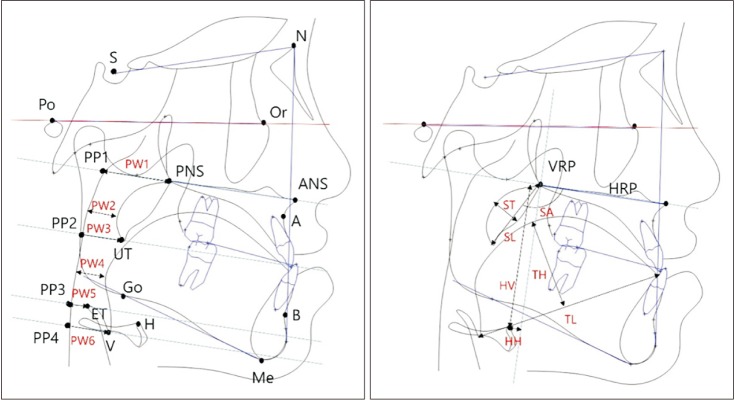
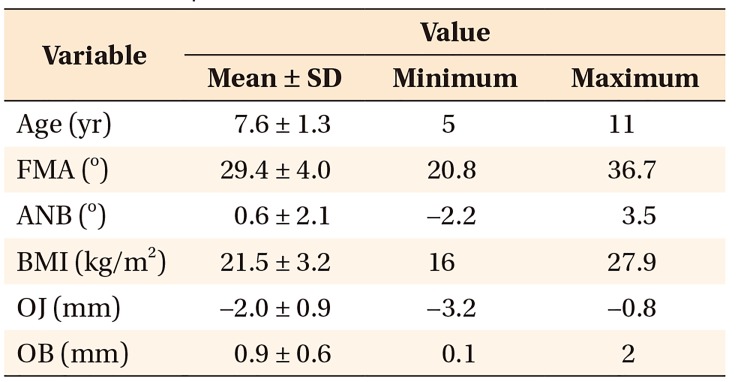
567 however, have used measurements taken from before and after orthodontic treatment, or while wearing a device, all of which presented limitations in maintaining consistent conditions with respect to growth, tongue position, and head posture. Thus, studies pertaining to changes in the PAS following mandibular posterior displacement that is unaffected by factors such as growth, tongue position, and head posture are unprecedented. The availability of two lateral cephalograms taken to diagnose functional Class III malocclusions may facilitate such studies.
The aim was to investigate the changes in the PAS following posterior displacement of the mandible by using cephalometric evaluations and to assess the interrelationships with the surrounding structures.
Go to :

DISCUSSION
The growth and development of the oral and maxillofacial system must be closely monitored before the growth rate reaches its peak in the adolescence period. In particular, it is very important to recognize and identify patients who have difficulty in nose-breathing in their early childhood. Orthodontists are responsible for preventing and eliminating any predisposing factors that may have adverse effects on growth direction and craniofacial patterns in the maxillofacial region. Since the mandible and the pharynx are closely interrelated, prediction of PAS changes that might interfere with breathing is crucial while designing intraoral devices for orthodontic or orthopedic treatments.
Since the pharynx is known to undergo rapid growth until 13 years of age,
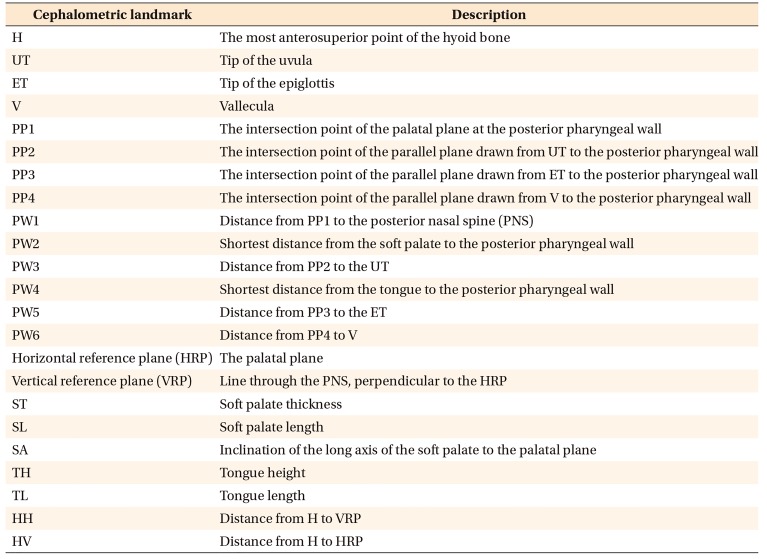
9 it is necessary to take into account developmental changes in order to accurately understand the dimensional changes in the PAS following mandibular displacement. Moreover, dimensional changes in the PAS may be biased by time discrepancies, resulting in discrepancies in head posture, tongue position, and so on. Therefore, it was difficult to clearly identify the changes exclusively pertaining to mandibular posterior displacement. In this study, we evaluated the changes in the PAS following mandibular posterior displacement at the same point in time in the same posture of the same patient, to accurately understand the correlations with the surrounding structures.
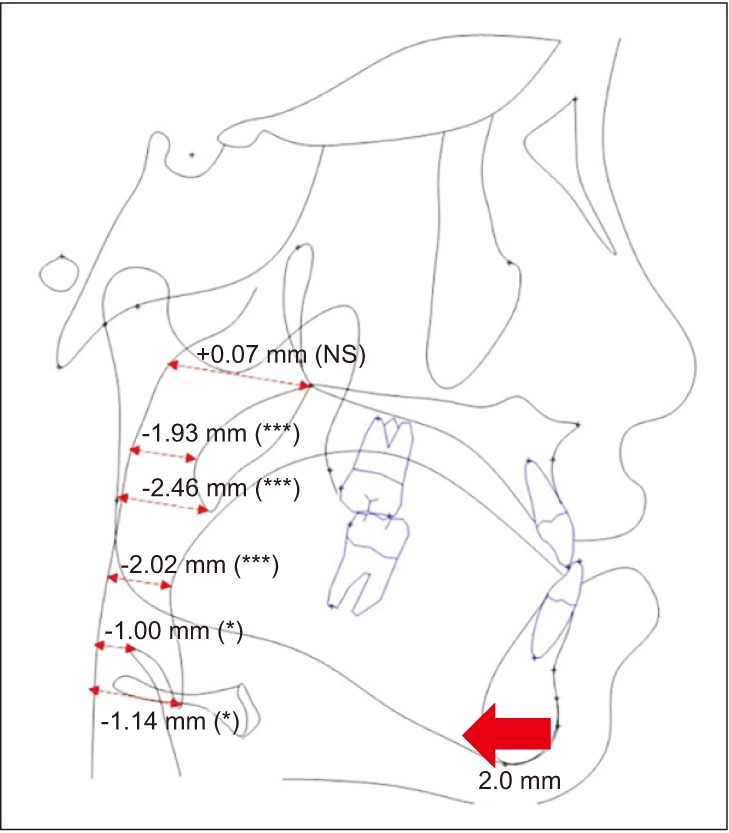
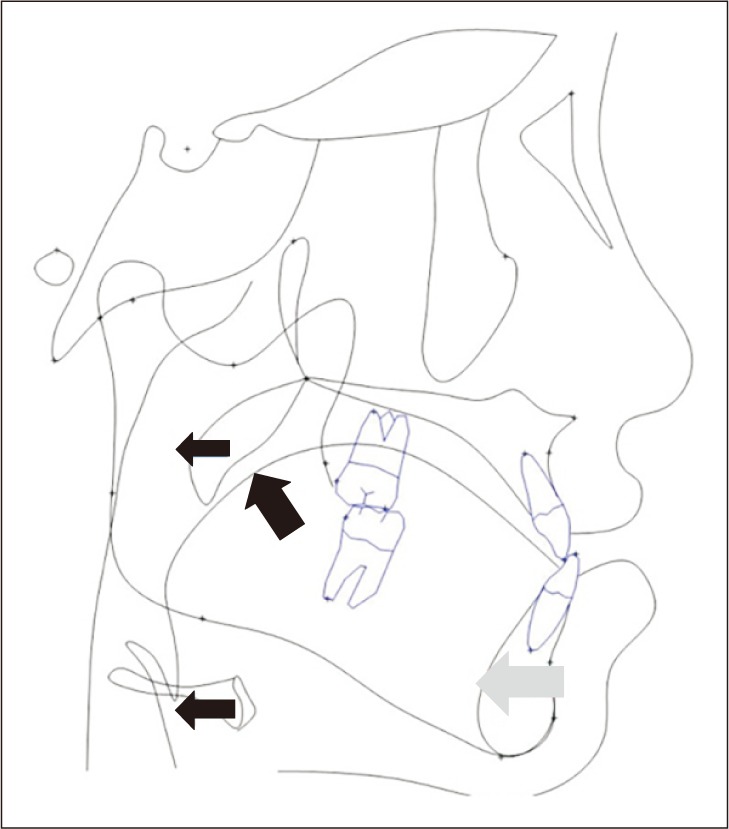
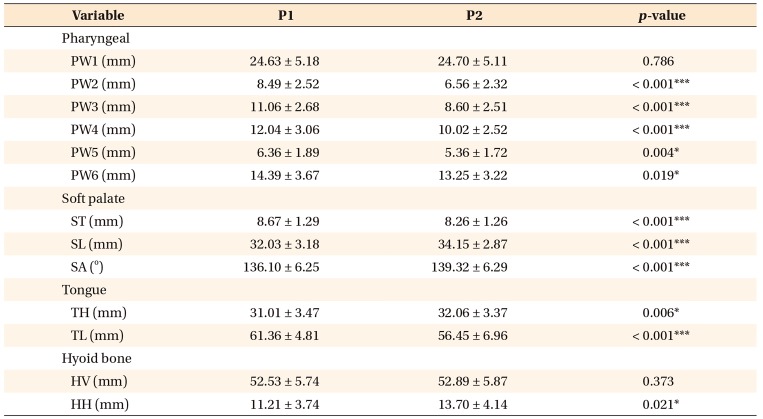
Statistical analysis showed reductions in the dimensional values in all regions of the PAS except the PW1 region since the mandible was posteriorly displaced. As the tongue is posteriorly displaced, the contact area between the tongue base and the soft palate increases, and accordingly, the soft palate is displaced posteriorly. No significant change was observed in PW1 presumably because PW1 is not affected by the surrounding structures. These results are similar to those obtained with mandibular setback surgery (MSS). Previous studies
610 showed that the PAS was narrowed immediately after MSS, and the tongue was displaced posteriorly.
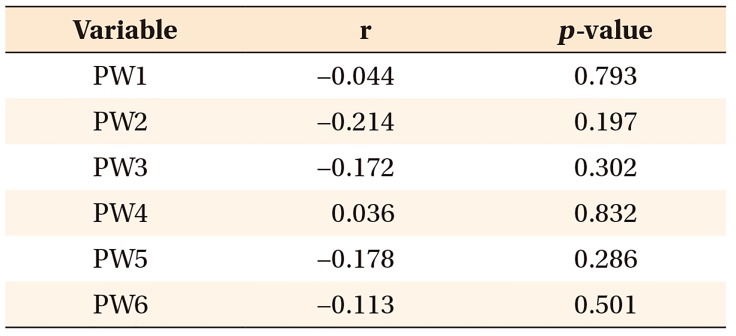
However, no correlation was found between the amount of mandibular posterior displacement and the dimensional change in the PAS. Thus, it is difficult to assume that the amount of decrease in the PAS corresponds to the degree of mandibular posterior displacement. This indicates limitations related to the inter-personal bias in the responses of the surrounding structures. In addition, the lateral cephalogram could not be used to obtain measurements of the horizontal dimensional change in the PAS. This resembles the results of previous studies on changes in the PAS after MSS. Panou et al.
11 found no correlation between the amount of surgical setback and the amount of dimensional change in the PAS in their study using cone-beam computed tomography (CBCT).
The effect of the hyoid bone on the dimensions of the PAS is still controversial.
1213 The hyoid bone is a mobile hard tissue that is largely affected by the surrounding structures. Thus, its position is determined by the equilibrium of the surrounding muscles—including the suprahyoid and infrahyoid muscles. According to this trial, the hyoid bone was displaced only in the posterior direction following mandibular posterior displacement. However, in 36.8% (14 of 38 patients), the hyoid bone showed upward displacement following posterior displacement, which is a result different from the posterior-inferior displacement of the hyoid bone after MSS. This is presumably attributable to the opening of the bite since the mandible is moved posteriorly into the edge-to-edge position. Theoretically, the hyoid bone is fixed in place by infrahyoid muscles during opening of the mouth, while the suprahyoid muscles pull the mandible toward the hyoid bone. However, as a matter of fact, true fixation of the hyoid bone is not actually seen during mandibular movement. This is because there is a time discrepancy in the actions of the supra- and infrahyoid muscles. The action of the infrahyoid muscles does not occur in the early phase of the opening of the mouth, and it is unable to counteract the action of the suprahyoid muscles.
14 For this reason, when the bite is opened, the hyoid is pulled superiorly by the suprahyoid muscles, such as the geniohyoid muscle. In this study, subjects with overbite greater than 2 mm, which was larger than average mandibular posterior displacement, were excluded in order to minimize this bite-opening effect. However, limitations still exist in that we could not completely eradicate the bite-opening effect.
Based on the study by Wright et al.,
15 we checked the normal tongue position in the lateral cephalogram taken for habitual occlusion. Mouth-breathers who tend to have tongue positions lower than the normal range and subjects with BMI over 30 kg/m
2 were excluded from the study to eliminate any bias that could reduce the dimensions of the PAS.
4 Moreover, subjects who showed changes in the cranio-cervical angle in the second vertebrae while taking two cephalograms were excluded because these changes influenced the dimensions of the PAS.
16
When lateral cephalograms are used to measure the dimensions of the PAS, extra caution is required to keep the same posture and head position for accurate measurement. Moreover, measurements using lateral cephalograms are insufficient to obtain information on the horizontal length or the three-dimensional volume of the PAS. Furthermore, the lateral cephalogram cannot be used for diagnosis of OSAS because OSAS occurs when the patient is sleeping and the lateral cephalogram is taken while the patient is standing. However, the previous study
17 showed a significant relationship between the dimensions of the PAS on lateral cephalograms and those on CBCT. Moreover, dimensional analysis of the PAS using the lateral cephalogram is practically convenient, cost-efficient, and beneficial in obtain quantitative information about the pharyngeal dimensions.
This study also has some limitations, which need to be considered when interpreting the data. First, the analysis using the lateral cephalogram was in two dimensions; three-dimensional analyses would be required in the future. Second, guidance to anterior edge-to-edge bite induces the bite-opening effect, thus leading to the inevitable incorporation of the effect of bite-opening in the data and not just the effect of mandibular posterior displacement. Because of ethical concerns, we could not conduct the prospective studies that consider two lateral cephalograms in altered mandibular positions in order to eliminate the bite-opening effect. Third, the results only showed the immediate effects of mandibular posterior displacement. Although immediate effects do not necessarily correspond to long-term effects, they can be used as a reference when designing intraoral devices. Fourth, the amount of mandibular posterior displacement was very small. Large-scale studies are needed. Lastly, there was a lack of control over the tongue position while taking lateral cephalograms. The tongue is the most versatile soft tissue. Control over the individual variables must be enhanced to obtain stronger results.
Go to :





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download