1. Nakatsuka K, Adachi T, Kato T, Oishi M, Murakami M, Okada Y, et al. Reliability of novel multidirectional lip-closing force measurement system. J Oral Rehabil. 2011; 38:18–26. PMID:
20722773.

2. Kaede K, Kato T, Yamaguchi M, Nakamura N, Yamada K, Masuda Y. Effects of lip-closing training on maximum voluntary lip-closing force during lip pursing in healthy young adults. J Oral Rehabil. 2016; 43:169–175. PMID:
26443933.

3. Weinstein S, Haack DC, Morris LY, Snyder BB, Attaway HE. On an equilibrium theory of tooth position. Angle Orthod. 1963; 33:1–26.
4. Proffit WR. Equilibrium theory revisited: factors influencing position of the teeth. Angle Orthod. 1978; 48:175–186. PMID:
280125.
5. Shaw WC, Addy M, Ray C. Dental and social effects of malocclusion and effectiveness of orthodontic treatment: a review. Community Dent Oral Epidemiol. 1980; 8:36–45. PMID:
6989548.

6. Chen S, Cai Y, Chen F. Lip closing force of Class III patients with mandibular prognathism: a case control study. Head Face Med. 2014; 10:33. PMID:
25159036.

7. Tomiyama N, Ichida T, Yamaguchi K. Electromyographic activity of lower lip muscles when chewing with the lips in contact and apart. Angle Orthod. 2004; 74:31–36. PMID:
15038488.
8. Gamboa NA, Miralles R, Valenzuela S, Santander H, Cordova R, Bull R, et al. Comparison of muscle activity between subjects with or without lip competence: electromyographic activity of lips, supra- and infrahyoid muscles. Cranio. 2017; 35:385–391. PMID:
27997289.

9. Posen AL. The influence of maximum perioral and tongue force on the incisor teeth. Angle Orthod. 1972; 42:285–309. PMID:
4507148.
10. Fındık Y, Baykul T, Aydın MA, Esenlik E, Ordu BN. Evaluation of lip force in patients with unilateral and bilateral cleft lip. Br J Oral Maxillofac Surg. 2017; 55:391–395. PMID:
28087210.

11. Kawabata A, Kobayashi T, Takagi A, Kuroyanagi F, Washino K, Sabashi K, et al. Multidirectional lip-closing force in adults with mandibular deviation. J Oral Rehabil. 2013; 40:664–669. PMID:
23855528.

12. Doto N, Yamada K. The relationship between maximum lip closing force and tongue pressure according to lateral craniofacial morphology. Orthod Waves. 2015; 74:69–75.

13. Takehana Y, Masuda Y, Kageyama T, Okazaki R, Murakami M, Yamada K. The relationship between lip-closing force and dental arch morphology in patient with Angle Class I malocclusion. J Oral Rehabil. 2017; 44:205–212. PMID:
27997984.

14. Young TM, Smith RJ. Effects of orthodontics on the facial profile: a comparison of changes during nonextraction and four premolar extraction treatment. Am J Orthod Dentofacial Orthop. 1993; 103:452–458. PMID:
8480714.

15. Kocadereli I. Changes in soft tissue profile after orthodontic treatment with and without extractions. Am J Orthod Dentofacial Orthop. 2002; 122:67–72. PMID:
12142899.

16. Ueki K, Mukozawa A, Okabe K, Miyazaki M, Moroi A, Marukawa K, et al. Changes in the lip closing force of patients with class III malocclusion before and after orthognathic surgery. Int J Oral Maxillofac Surg. 2012; 41:835–838. PMID:
22398020.

17. Ueki K, Moroi A, Sotobori M, Ishihara Y, Marukawa K, Iguchi R, et al. Evaluation of recovery in lip closing pressure and occlusal force and contact area after orthognathic surgery. J Craniomaxillofac Surg. 2014; 42:1148–1153. PMID:
24559719.

18. Yuce E, Baykul T, Findik Y, Alkis H. Evaluation of changes in lip closing force after surgically assisted rapid maxillary expansion. J Craniofac Surg. 2016; 27:649–653. PMID:
27054425.

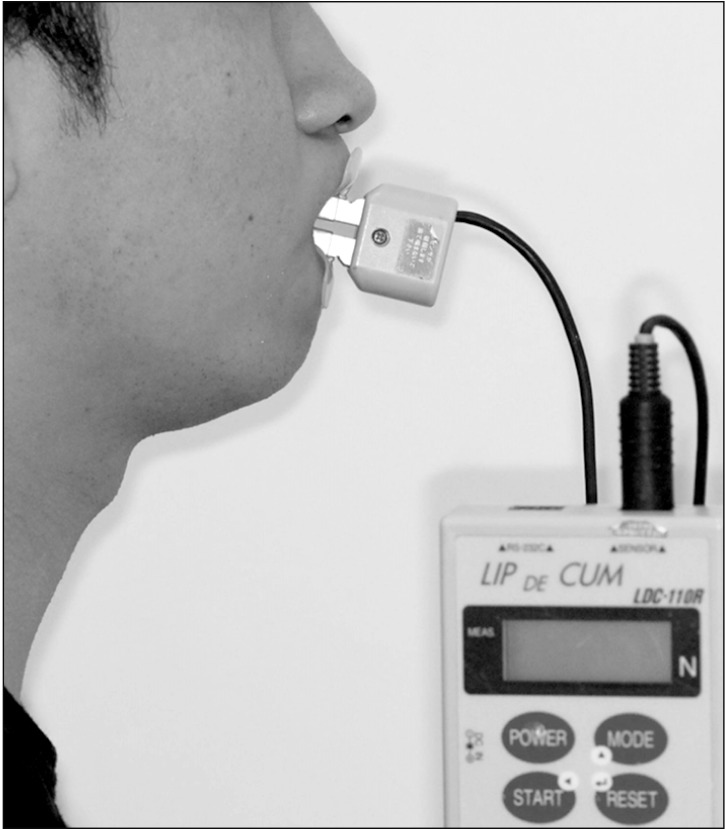
19. Ono T, Hori K, Masuda Y, Hayashi T. Recent advances in sensing oropharyngeal swallowing function in Japan. Sensors (Basel). 2010; 10:176–202. PMID:
22315534.

20. Jung MH, Yang WS, Nahm DS. Effects of upper lip closing force on craniofacial structures. Am J Orthod Dentofacial Orthop. 2003; 123:58–63. PMID:
12532064.

21. Thüer U, Ingervall B. Pressure from the lips on the teeth and malocclusion. Am J Orthod Dentofacial Orthop. 1986; 90:234–242. PMID:
3463198.

22. Posen AL. The application of quantitative perioral assessment to orthodontic case analysis and treatment planning. Angle Orthod. 1976; 46:118–143. PMID:
1064341.
23. Kato Y, Kuroda T, Togawa T. Perioral force measurement by a radiotelemetry device. Am J Orthod Dentofacial Orthop. 1989; 95:410–414. PMID:
2718971.

24. Jung MH, Yang WS, Nahm DS. Maximum closing force of mentolabial muscles and type of malocclusion. Angle Orthod. 2010; 80:72–79. PMID:
19852643.

25. Ingervall B, Janson T. The value of clinical lip strength measurements. Am J Orthod. 1981; 80:496–507. PMID:
6946706.

26. Partal I, Aksu M. Changes in lips, cheeks and tongue pressures after upper incisor protrusion in Class II division 2 malocclusion: a prospective study. Prog Orthod. 2017; 18:29. PMID:
28944417.

27. Lambrechts H, De Baets E, Fieuws S, Willems G. Lip and tongue pressure in orthodontic patients. Eur J Orthod. 2010; 32:466–471. PMID:
20089572.

28. Drobocky OB, Smith RJ. Changes in facial profile during orthodontic treatment with extraction of four first premolars. Am J Orthod Dentofacial Orthop. 1989; 95:220–230. PMID:
2923102.

29. Aksu M, Kocadereli I. Arch width changes in extraction and nonextraction treatment in class I patients. Angle Orthod. 2005; 75:948–952. PMID:
16448236.
30. Herzog C, Konstantonis D, Konstantoni N, Eliades T. Arch-width changes in extraction vs nonextraction treatments in matched Class I borderline malocclusions. Am J Orthod Dentofacial Orthop. 2017; 151:735–743. PMID:
28364897.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download