1. Sandstrom I. Omen ny Kortel hos mennisken och atskilige baggdjur. Upsala: Lakarefore rings;1880.
2. Gley E. Sur les fonctions du corps thyroïde. C R Soc Biol (Paris). 1891; 43:841–847.
3. Erdheim J. Ueber tetania parathyreopriva. Wien Klin Wochenschr. 1906; 19:716–717.
4. Collip JB. The extraction of a parathyroid hormone which will prevent or control parathyroid tetany and which regulates the level of blood calcium. J Biol Chem. 1925; 63:395–438.

5. Aurbach GD. Isolation of parathyroid hormone after extraction with phenol. J Biol Chem. 1959; 234:3179–3181. PMID:
13848891.

6. Rasmussen H, Craig L. Purification of parathyroid hormone by use of counter-current distribution. J Am Chem Soc. 1959; 81:5003.

7. Keutmann HT, Sauer MM, Hendy GN, O'Riordan LH, Potts JT Jr. Complete amino acid sequence of human parathyroid hormone. Biochemistry. 1978; 17:5723–5729. PMID:
728431.

8. Antonarakis SE, Phillips JA 3rd, Mallonee RL, Kazazian HH Jr, Fearon ER, Waber PG, et al. Beta-globin locus is linked to the parathyroid hormone (PTH) locus and lies between the insulin and PTH loci in man. Proc Natl Acad Sci U S A. 1983; 80:6615–6619. PMID:
6314332.

9. Bai M, Quinn S, Trivedi S, Kifor O, Pearce SH, Pollak MR, et al. Expression and characterization of inactivating and activating mutations in the human Ca2+o-sensing receptor. J Biol Chem. 1996; 271:19537–19545. PMID:
8702647.
10. Ding C, Buckingham B, Levine MA. Familial isolated hypoparathyroidism caused by a mutation in the gene for the transcription factor GCMB. J Clin Invest. 2001; 108:1215–1220. PMID:
11602629.

11. Nesbit MA, Hannan FM, Howles SA, Babinsky VN, Head RA, Cranston T, et al. Mutations affecting G-protein subunit α11 in hypercalcemia and hypocalcemia. N Engl J Med. 2013; 368:2476–2486. PMID:
23802516.
12. Ahn TG, Antonarakis SE, Kronenberg HM, Igarashi T, Levine MA. Familial isolated hypoparathyroidism: a molecular genetic analysis of 8 families with 23 affected persons. Medicine (Baltimore). 1986; 65:73–81. PMID:
3005800.
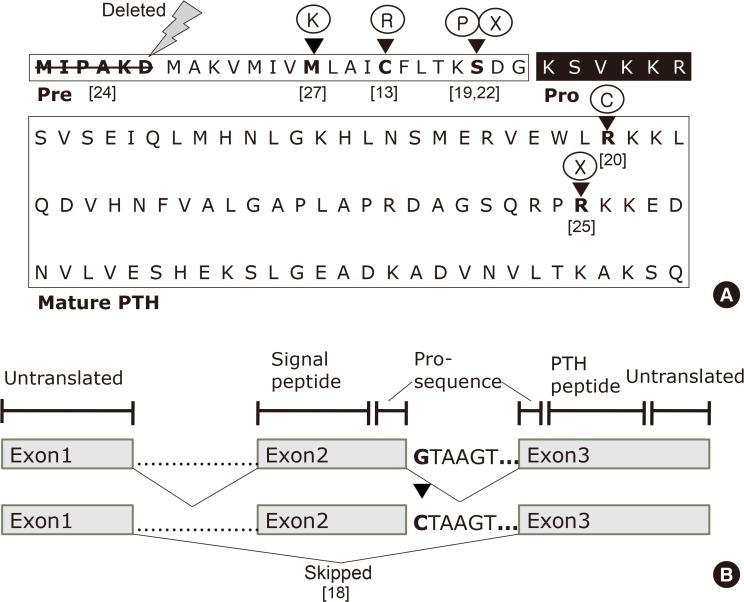
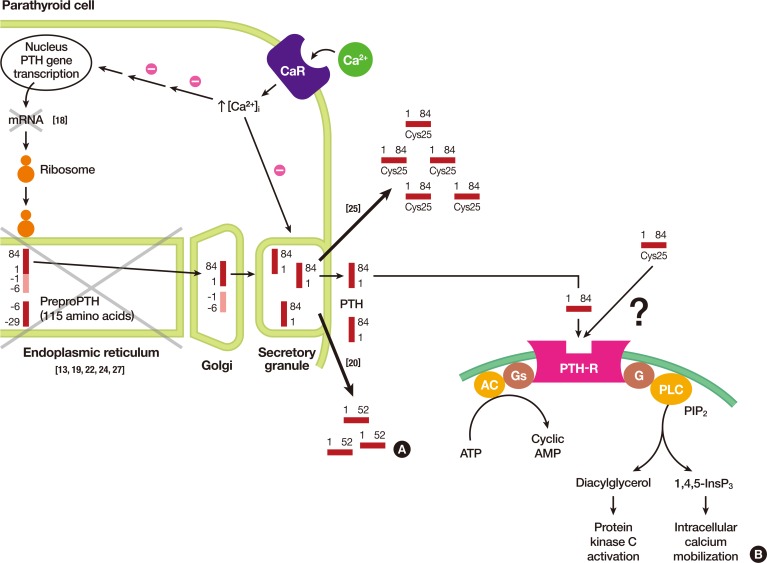
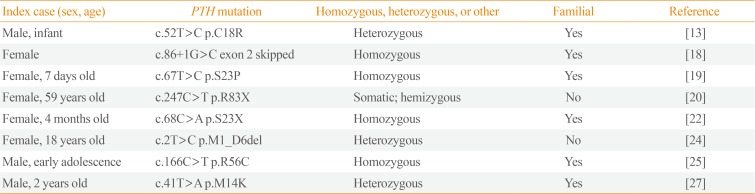
13. Arnold A, Horst SA, Gardella TJ, Baba H, Levine MA, Kronenberg HM. Mutation of the signal peptide-encoding region of the preproparathyroid hormone gene in familial isolated hypoparathyroidism. J Clin Invest. 1990; 86:1084–1087. PMID:
2212001.

14. Karaplis AC, Lim SK, Baba H, Arnold A, Kronenberg HM. Inefficient membrane targeting, translocation, and proteolytic processing by signal peptidase of a mutant preproparathyroid hormone protein. J Biol Chem. 1995; 270:1629–1635. PMID:
7829495.

15. Suprasdngsin C, Wattanachal A, Preeysombat C. Parathyroid hormone gene mutation in patient with hypoparathyroidism (Annual Research Abstract 164). 128. Bangkok: Mahidol University;2001.
16. Datta R, Waheed A, Shah GN, Sly WS. Signal sequence mutation in autosomal dominant form of hypoparathyroidism induces apoptosis that is corrected by a chemical chaperone. Proc Natl Acad Sci U S A. 2007; 104:19989–19994. PMID:
18056632.

17. Hammer GD, McPhee SJ. Chapter 17, Disorders of the parathyroids & calcium & phosphorus metabolism. Pathophysiology of disease: an introduction to clinical medicine. 7th ed. New York: McGraw-Hill Education;2014.
18. Parkinson DB, Thakker RV. A donor splice site mutation in the parathyroid hormone gene is associated with autosomal recessive hypoparathyroidism. Nat Genet. 1992; 1:149–152. PMID:
1302009.

19. Sunthornthepvarakul T, Churesigaew S, Ngowngarmratana S. A novel mutation of the signal peptide of the preproparathyroid hormone gene associated with autosomal recessive familial isolated hypoparathyroidism. J Clin Endocrinol Metab. 1999; 84:3792–3796. PMID:
10523031.

20. Au AY, McDonald K, Gill A, Sywak M, Diamond T, Conigrave AD, et al. PTH mutation with primary hyperparathyroidism and undetectable intact PTH. N Engl J Med. 2008; 359:1184–1186.
21. Lim SK, Gardella TJ, Baba H, Nussbaum SR, Kronenberg HM. The carboxy-terminus of parathyroid hormone is essential for hormone processing and secretion. Endocrinology. 1992; 131:2325–2330. PMID:
1425431.

22. Ertl DA, Stary S, Streubel B, Raimann A, Haeusler G. A novel homozygous mutation in the parathyroid hormone gene (PTH) in a girl with isolated hypoparathyroidism. Bone. 2012; 51:629–632. PMID:
22722080.

23. Goswami R, Mohapatra T, Gupta N, Rani R, Tomar N, Dikshit A, et al. Parathyroid hormone gene polymorphism and sporadic idiopathic hypoparathyroidism. J Clin Endocrinol Metab. 2004; 89:4840–4845. PMID:
15472173.

24. Tomar N, Gupta N, Goswami R. Calcium-sensing receptor autoantibodies and idiopathic hypoparathyroidism. J Clin Endocrinol Metab. 2013; 98:3884–3891. PMID:
23873991.

25. Lee S, Mannstadt M, Guo J, Kim SM, Yi HS, Khatri A, et al. A homozygous [Cys25]PTH(1-84) mutation that impairs PTH/PTHrP receptor activation defines a novel form of hypoparathyroidism. J Bone Miner Res. 2015; 30:1803–1813. PMID:
25891861.

26. White AD, Fang F, Jean-Alphonse FG, Clark LJ, An HJ, Liu H, et al. Ca(2+) allostery in PTH-receptor signaling. Proc Natl Acad Sci U S A. 2019; 116:3294–3299. PMID:
30718391.

27. Cinque L, Sparaneo A, Penta L, Mencarelli A, Rogaia D, Esposito S, et al. Autosomal dominant PTH gene signal sequence mutation in a family with familial isolated hypoparathyroidism. J Clin Endocrinol Metab. 2017; 102:3961–3969. PMID:
28938448.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download