INTRODUCTION
Acromegaly is a disease characterized by chronic growth hormone (GH) and insulin-like growth factor-1 (IGF-1) hypersecretion [
12]. It is primarily caused by a GH-secreting pituitary adenoma. Although surgical resection of the pituitary adenoma is the first choice of treatment for many patients, it restores normal IGF-1 levels in less than 60% of cases [
12]. In patients unsuitable or unwilling to undergo surgery, or in whom surgery fails to normalize plasma GH and IGF-1 concentrations, pharmacological intervention is the standard procedure [
12].
Somatostatin (SST) analogs and dopamine agonists (DAs) are useful in treating GH-secreting pituitary adenoma [
345]. As GH-secreting pituitary adenomas are associated with increased expression of SST and dopamine receptors, drugs targeting these receptors hold therapeutic potential against acromegaly [
34567]. However, they are relatively less effective for controlling hormonal secretion and reducing tumor sizes [
2345678]. SST analogs, such as lanreotide, have been consistently shown to reduce hormonal hypersecretion in 60% to 70% of patients [
123], whereas DAs, such as cabergoline (CAB), may be effective in up to 30% of patients with mildly elevated plasma IGF-1 concentrations [
12]. SST and DAs are useful for the treatment of acromegaly, but they are not cost-effective and cases of unresponsiveness as well as resistance have been reported [
9]. Therefore, there is a need for alternative pharmacological approaches to treat acromegaly.
Recently, a series of novel chimeric molecules consisting of a SST analog and a DA have been synthesized and are currently being tested [
1011121314]. The chimeric molecule used in this study acts on both SST receptors 2 and 5 as well as on dopamine receptor subtype 2; thus, it can be a promising candidate for the treatment of acromegaly and GH-secreting pituitary adenoma.
The main purpose of this study was to confirm the effect of BIM23B065 on GH-secreting pituitary adenoma and provide evidence for its approval as a new therapeutic option for acromegaly. Owing to increased efficiency via differentiated mechanisms, this chimeric drug is expected to overcome the low rate of responsiveness to previously used drugs.
Go to :

METHODS
Ethical statement
The Institutional Animal Care and Use Committee of Yonsei University Health System reviewed and approved (approval number: 2015-0403) all animal procedures. Experiments were carried out under the strict guidance of the Association for Assessment and Accreditation of Laboratory Animal Care. Animals were housed under standard conditions consisting of 12-hour light/dark cycles (lights were turned on at 7:00 AM) and a temperature of 22℃ to 24℃. The animals had ad libitum access to standard rodent chow and water, except during intended fasting periods designated for specific experimental protocols. All mice were maintained in accordance with the American Association of Laboratory Animal Care guidelines.
Cell culture
For in vitro experiments, the rat pituitary tumor cell line GH3 (American Type Culture Collection) was used. These cells were grown in Dulbecco's modified Eagle medium (DMEM)/high-glucose medium supplemented with 10% fetal bovine serum and penicillin-streptomycin solution (Hyclone Co., Logan, UT, USA). The cells were placed in a culture incubator that maintained atmospheric conditions of 37℃ and 5% CO2. The medium was changed within 3 days, and the cells were split with trypsin/ethylenediaminetetraacetic acid (EDTA) every week.
Experimental animals
The animal model used in this study was a previously developed mouse model, which expressed the phenotype of GH-secreting pituitary adenomas [
8]. A somatotroph-specific aryl hydrocarbon receptor interacting protein knockout (sAIPKO) mouse model was established using rGHp-Cretg/+; Aiplox/lox mice [
15]. All mice in this study were males above 40 weeks of age because most sAIPKO mice develop GH-secreting pituitary adenomas as they age (>40 weeks).
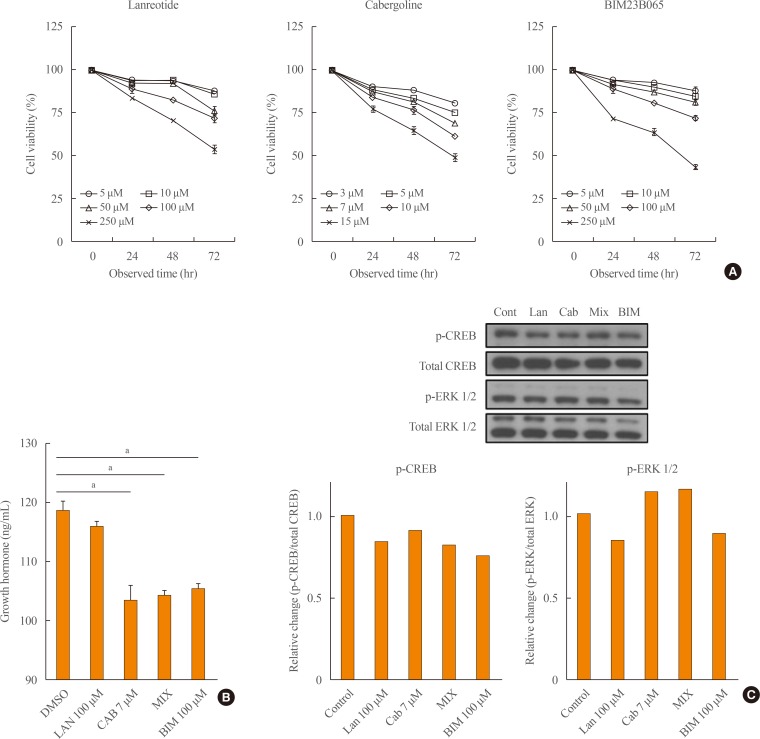
Cell proliferation assay
To test the cytotoxicity of drugs, MTS assays were performed. GH3 cells (100 µL) were seeded in a 96-well plate at a density of 4×103 cells/well. After 24 hours of incubation at 37℃ in a 5% CO2 incubator, the growth medium was replaced with DMEM/high-glucose medium without serum to induce starvation conditions. After 12 hours, media containing three different drugs, namely lanreotide (5, 10, 50, 100, or 250 µM), CAB (3, 5, 7, 10, or 15 µM), and BIM23B065 (5, 10, 50, 100, or 250 µM) were prepared. The control group was treated with dimethyl sulfoxide (DMSO). After treatment with drugs, the cells were incubated for 24, 48, and 72 hours in the incubator.
MTS solution (Promega, Madison, WI, USA) was diluted by mixing 150 µL of the solution with 1 mL of medium. The cells were treated with MTS medium for 1.5 hours in the incubator. The optical density was observed under 495 nm using a spectrophotometer (Versa Max microplate reader, Molecular Devices, San Jose, CA, USA).
GH and IGF-1 ELISA
The medium collected from the cell culture was tested for changes in GH levels before and after drug treatment. To determine the effect of the drug in normalizing GH and IGF-1 levels in the animal model, blood serum samples collected before and after treatment were tested. GH and IGF-1 levels were measured using rat/mouse growth hormone enzyme-linked immunosorbent assay (ELISA) kit 96-Well Plates (Millipore, Billerica, MA, USA) and mouse IGF-1 ELISA kit (Abcam, Cambridge, UK), respectively, according to the manufacturer's instructions.
Western blotting
Before drug treatment, the cells were seeded and stabilized for 24 hours. After treatment with drugs for 15 minutes, the plates were washed twice with 1X Dulbecco's Phosphate-Buffered Saline. The plates were then kept on ice and treated with protein lysis buffer, which is composed of 10% glycerol, 50 mM Na3VO4, 100 mM NaF, 100 mM phenylmethylsulfonyl fluoride, and 100 mM dithiothreitol mixed in radioimmunoprecipitation assay (RIPA) buffer. The cells were collected in 1.5 mL microcentrifuge tubes using a cell scraper and incubated on ice for 1 hour with frequent mixing. The samples were then centrifuged for 20 minutes at 15,380 g, and the supernatant was transferred to new Eppendorf tubes.
The protein concentrations were measured using Bradford assay (Bio-Rad laboratories, Hercules, CA, USA) and set to 50 µM for all samples. The samples were prepared with 10% sodium dodecyl sulfate-polyacrylamide gel electrophoresis (SDS-PAGE) buffer and denatured in a heating block at 95℃ for 5 minutes.
Proteins were separated by size using gel electrophoresis and transferred to Immobilon polyvinylidene difluoride membranes by wet transfer technique. The obtained membranes were blocked with 5% skim milk for 1 hour to prevent non-specific binding with antibodies and probed with anti-phospho-cyclic AMP response element binding (CREB) (1:1,000, Cell Signaling Technology, Danvers, MA, USA), anti-total-CREB (1:1,000, Cell Signaling Technology), anti-phospho-extracellular signal-regulated kinase (ERK) 1/2 (1:2,000, Cell Signaling Technology), anti-total ERK 1/2 (1:4,000, Cell Signaling Technology) overnight at 4℃. The membrane was washed in 1X TBS-T solution and reacted with the secondary antibody (1:4,000, Thermo Fisher Scientific, Waltham, MA, USA) for another 1 hour at room temperature. After TBS-T washing, proteins on the membrane were detected using a West Save Up Western Blot detection kit (AbFrontier #LF-QC0101) on an enhanced chemiluminescence film.
Osmotic pump implantation
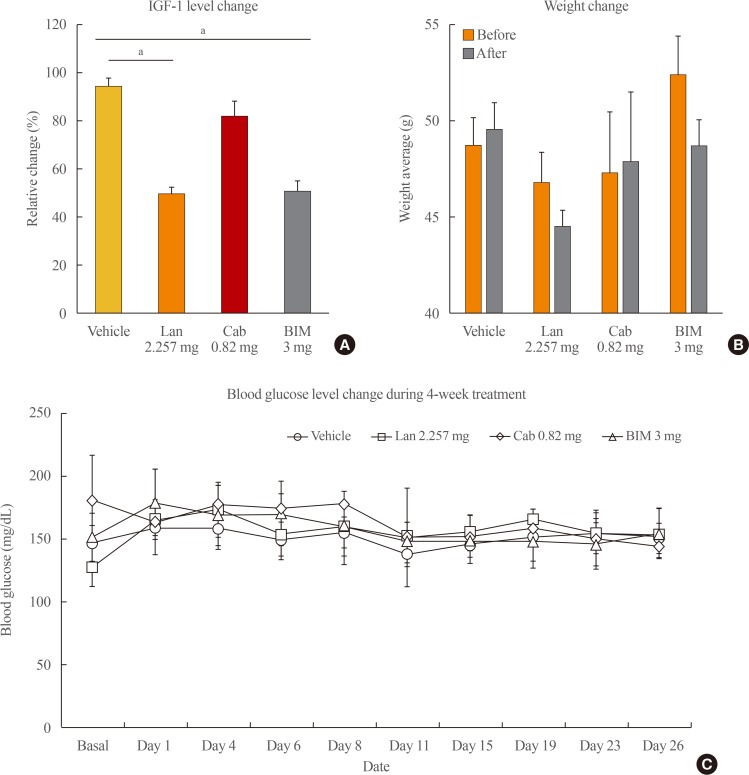
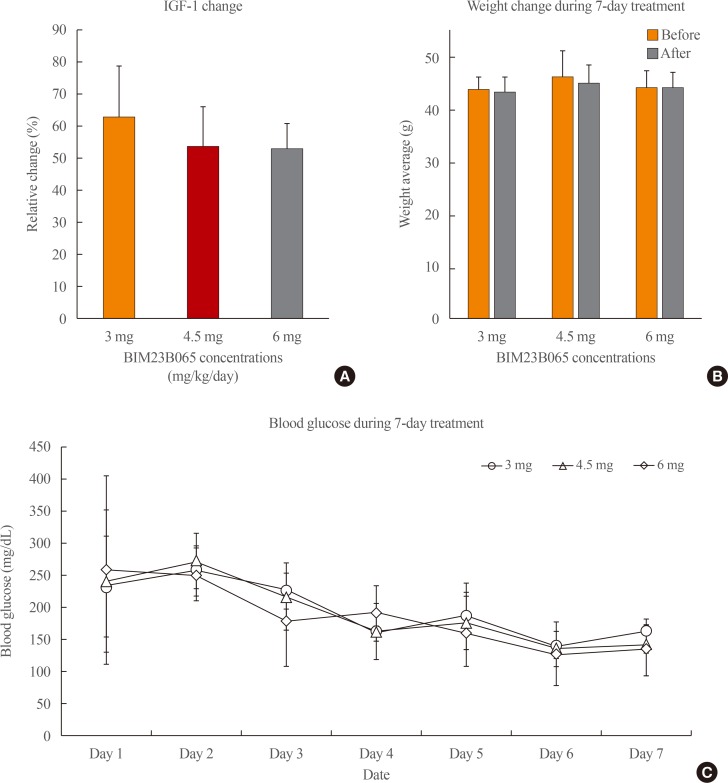
Establishment of the knockout model was confirmed by genotyping. To determine the dosage of the new chimeric molecule drug, three different doses of the drug were tested on sAIPKO mice. In total, 16 male mice (>40 weeks of age) were divided into four groups (vehicle, lanreotide, CAB, and chimeric molecule groups) of four mice each.
The drug was administered for 7 days using Alzet mini-osmotic pumps (Durect Co., Cupertino, CA, USA). Osmotic pump was prepared according to the manufacturer's protocol. The drug concentration was calculated individually based on animal weight. For implantation surgery, the animals were subjected to anesthesia using isoflurane. After blood was withdrawn by retro-orbital bleeding, the pump was implanted under the epidermis on the dorsal posterior side of the animals as the incision wound was clipped. Blood glucose level and body weight were measured daily to monitor the condition of the animals.
After the concentration was set, the four groups were treated for one month. To reduce the stress associated with the insertion of the drug-release pumps, a 14-day release pump was used instead of a 7-day release pump. The test concentration of lanreotide was set at the same molar concentration as BIM23B065. CAB concentration was set based on previous animal studies [
1617]. The procedure and protocols were the same as the previous experiment, save for the pump type and monitoring frequency. The pump type was changed to 14-day release pump so that the pump was changed to a newly prepped pump after 2 weeks. In addition, the condition of animals was monitored every other day.
Lanreotide and BIM23B065 were provided by Ipsen (Boston, MA, USA) and CAB was purchased from Dongkoo Bio & Pharma (Seoul, Korea).
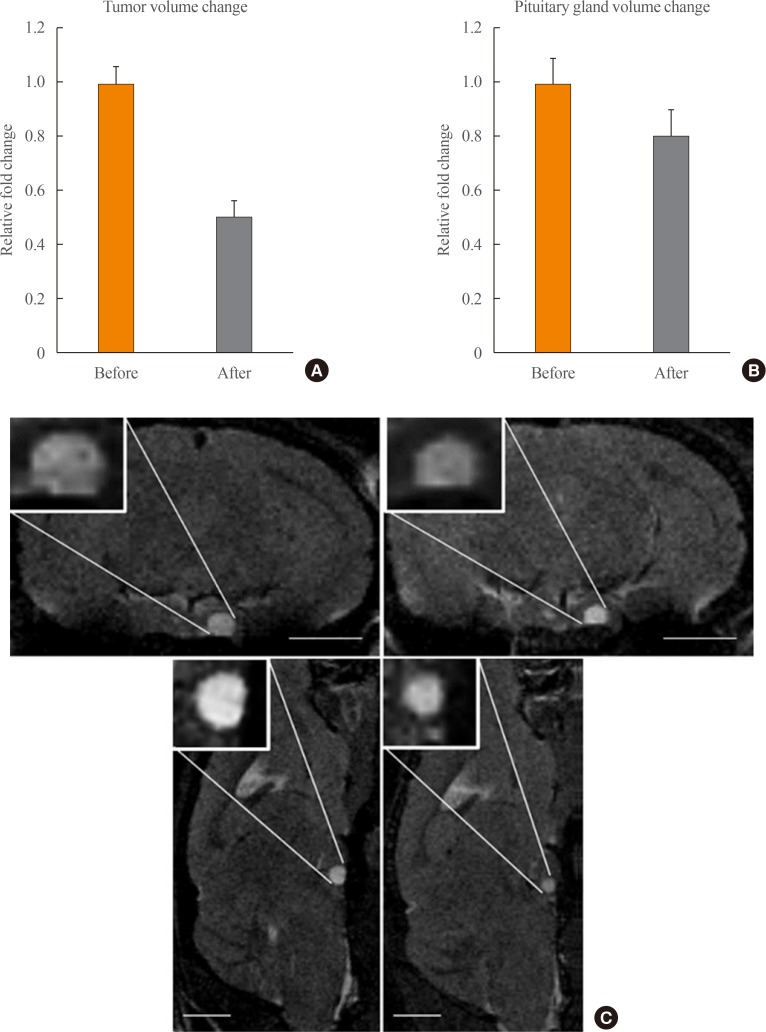
Magnetic resonance imaging
All magnetic resonance imaging (MRI) experiments were performed on a 9.4T Bruker BioSpec 94/20 USR small animal imaging system (Bruker BioSpin MRI GmbH, Ettlingen, Germany) equipped with 1H mouse body coil. T2-weighted MRI scan was performed, and tumor size was measured using OsiriX DICOM viewer before and after treatment with the chimeric molecule. The tumor volume was estimated according to equation 1: tumor volume=(length×width
2)/2 [
18].
Statistical analyses
Statistical analysis was performed using Microsoft Excel (Microsoft, Redmond, WA, USA). The results are expressed as mean±standard error of the mean of the results from three independent experiments with similar patterns. Differences were assessed by analysis of variance (ANOVA). P<0.05 was considered significant.
Go to :

DISCUSSION
Recently, the Acromegaly Guidelines reported that pharmaceutical treatment as well as surgical interventions can be administered as primary treatment options for acromegaly [
1]. The drugs used for GH-secreting pituitary adenoma treatment act on both SST and dopamine receptors [
12]. Although SST analogs and DAs have been reported for the treatment of GH-secreting pituitary adenomas, the response rate of SST is only between 60% to 70%. Moreover, DAs are reported to be effective only in cases of mild hormonal activity [
1]. Resistance to SST analogs has reduced the available treatment options. Therefore, a novel chimeric drug (BIM-23A760) was first synthesized to circumvent the issue of unresponsiveness to existing drugs [
101112131419]. This new chimeric molecule, which is a combination of the two most commonly used drugs for the treatment of pituitary diseases, is a potential drug candidate.
SST analogs and DAs act via different mechanisms. SST analogs have tumor static effects, while CAB (DA) causes apoptosis. As chimeric molecules exhibit two mechanisms, they are generally considered to possess the merits of both incorporated drugs and presumably have a synergistic effect. Previously synthesized chimeric molecules (BIM-23A760) have exhibited inhibitory effects on pituitary hormones such as GH and prolactin (PRL); however, some molecules showed ineffective outcomes [
11]. The examined chimeric molecule (BIM-23A760) presented positive outcomes only in reducing tumor size in non-functioning pituitary adenoma
in vivo [
13]. Moreover, it has also been reported to show inhibitory effects on the secretion of GH and PRL
in vitro only [
1019]. The present study showed that the chimeric molecule BIM23B065 is also effective in a pituitary adenoma mouse model.
According to the study that investigated the effects of an earlier version of this chimeric molecule, it was shown to suppress GH and PRL secretion from human acromegaly tumor cell cultures significantly better than individual SST analogs and DAs as well as their combination. This indicated that it acts on receptors other than SST receptors [
19]. However, after multiple dosing, an active metabolite of BIM-23A760 was formed and interfered with the parent compound, after which BIM-23A760 development was halted. Whereas, the main metabolite of BIM23B133 did not interfere with the parent compound, BIM23B065 and did not bind to any of the SST receptors, so BIM23B065 is more effective in reducing GH level and tumor size than BIM-23A760 [
20].
The chimeric molecule (BIM23B065) in this study was comprised of a SST analog (lanreotide) and a DA (CAB) in a 1:1 ratio. The chimeric molecule and not individual drugs was used because of heterodimerization between SST/DA receptor, assuming that the chimeric molecule interacts more effectively than individual drugs [
1119]. Being a novel agent and not just a mixture of two drugs, BIM23B065 was observed to be significantly more effective
in vitro than the mixture of lanreotide and CAB. In this study, we aimed to elucidate the mechanism of action of BIM23B065 in GH3 cells by investigating cell proliferation at different concentrations, CREB and ERK 1/2 phosphorylation, and changes in GH release.
BIM23B065 and lanreotide were similarly toxic to GH3 cells. However, CAB was effective at a much lower concentration than those of the other two drugs. Assuming that the chimeric molecule is made of a direct combination of a SST analog and a DA, the concentration of lanreotide administered to the animals was set equivalent to that of the chimeric molecule.
In vitro and
in vivo tests confirmed that the chimeric molecule was effective in lowering pituitary hormone activity. The animal model used in the study was a novel acromegaly mouse model that exhibited the phenotype of pituitary hyperplasia and eventual growth of pituitary tumors as the mice aged [
8]. The mice demonstrated similar clinical features to human acromegaly, wherein increased secretion of GH and expression of SST receptor type 2 (SSTR2), SSTR5, and dopamine receptor type 2 (DRD2) in the pituitary gland were observed.
After 7 days of treatment with BIM23B065 in sAIPKO acromegalic mice, the level of IGF-1 was not uniformly decreased in each dosage group. It was assumed that the IGF-1 level was influenced by mechanical stress induced in the mice during the pump implant surgery. Additionally, the duration of the pump (7 days) may have been too short for the drug to demonstrate its full effect. However, no change in body weight was observed, indicating that the drug was not toxic. Based on the results of this experiment, we performed a second 4-week study with the duration of the pump changed to 14 days, so that surgical intervention was required only once during the entire treatment. BIM23B065 was delivered via the 14-day pump at a dose of 3 mg/kg/day.
The results of the second animal experiment were relatively uniform. Body weights and blood glucose levels were stable throughout the entire experimental duration. The IGF-1 level significantly decreased after BIM23B065 treatment as compared to after CAB and lanreotide treatment; the IGF-1 level in most of the BIM23B065-treated mice was reduced by 50% post-treatment.
Four weeks of treatment with BIM23B065 also significantly decreased tumor mass and size of the pituitary gland. Two of three sAIPKO mice with pituitary adenoma had hyperplastic tumors. Although MRI results may not be significant, it showed the size of tumor and hyperplasia pituitary shrinkage. Therefore, BIM23B065 could possibly be used in patients with pre-tumor abnormalities.
There are certain limitations to this study. First, the results showed that BIM23B065 had a similar effect to SST analogs, which was used as a positive control in the animal study. SST analog was ineffective in GH3 cells, but effective in animal model; however, the DA showed opposite effects. BIM23B065 was effective both in GH3 cells and in the animal model. Indeed, when applied to patients with sporadic GH-secreting pituitary adenoma caused by various genome changes, chimeric molecules may be effective in patients with non-responsive to lanreotide, but human studies have not confirmed in this study. Second, the sample size (n=5) was small. All five animals had hyperplasia and three of them had tumors. The effects of the drug were observed in all the animals compared with the control group. Thus, the chimeric molecule is effective in both hyperplasia and pituitary tumors. Third, it was impossible to fully understand the effects of BIM23B065 on metabolic parameters. The physical activity and blood glucose levels of the animals remained stable throughout the study, but there may be complications associated with the use of the novel drug. No adverse effects were observed in the liver and kidney; however, other side effects could exist. Therefore, examination of long-term effects with a larger number of experimental animals will be required in further studies. Finally, dose-dependent experiments of lanreotide and CAB could not be carried out in GH-secreting pituitary adenomas animal model. In the case of BIM series in both in vitro and in vivo, the treatment concentrations were determined after confirming the dose-dependent efficacy, and the same concentrations of lanreotide corresponding to the BIM series were treated. In the case of CAB, we proceeded with reference to existing paper references. Since we focus on the effects of the BIM series, the does-dependent experiments of lanreotide and CAB could not be carried out. Also, even in MRI results, the purpose of the study was to analyze the effects of biochemical activity on the primary end point. The analysis of tumor size changes in the animal model for the use of lanreotide and CAB did not proceed due to the limitation of the number of MRIs in experimental animals at the medical institution.
Previous studies have confirmed the inhibitory effect on cell proliferation and hormone secretion only
in vitro [
101112131419]. This study showed that BIM23B065 effectively decreased not only GH release in GH3 cells, but also IGF-1 levels in a GH-secreting pituitary adenoma mouse model. The reduction of hormone activity by BIM23B065
in vivo shows promising results for its future clinical use. However, GH levels remained unchanged (data not shown). This could be because GH is released in a pulsatile manner every three hours and could not be monitored at the accurate time. In addition, GH is a stress hormone that is sensitive to anesthesia or orbital venous congestion. The secretion of IGF-1, stimulated by GH, decreased. The chimeric molecule showed distinct effects compared to those of the combination of lanreotide and CAB, indicating that this is a novel drug and not just a mixture of two drugs. Based on the results of this study, BIM23B065 holds potential to be developed into a novel therapeutic agent for acromegaly. Future studies are warranted to investigate its effects further.
Go to :





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download