INTRODUCTION
MATERIALS AND METHODS
Patients
CT Protocol
Image Analysis
Statistical Analysis
RESULTS
Baseline Chest Radiographic Findings
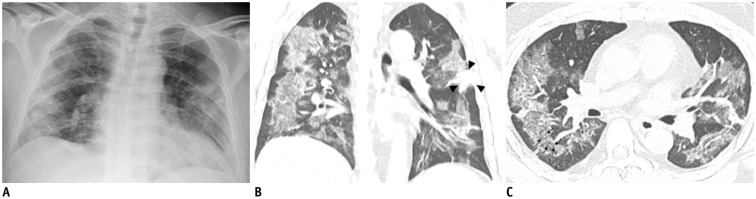 | Fig. 1Representative chest radiographic (A) and CT images (B, C) of COVID-19 pneumonia manifesting as confluent mixed ground-glass opacities and consolidation on CT.
A. Anteroposterior chest radiograph shows multifocal patchy peripheral consolidations in bilateral lungs, except for left upper lung zone. B, C. Coronal and axial chest CT images show confluent mixed ground-glass opacities and consolidative lesions in peripheral bilateral lungs. Discrete patchy consolidation (arrowheads) is noted in left upper lobe. On axial CT image (C), confluent lesions are mainly distributed in peripheral lung along bronchovascular bundles. Most of lesions spare juxtapleural area, and minor proportion of lesions touch pleura. Lesions contain multiple air-bronchograms, and air-bronchogram in superior segment of right lower lobe is distorted (arrows). COVID-19 = Coronavirus disease 2019, CT = computed tomography
|
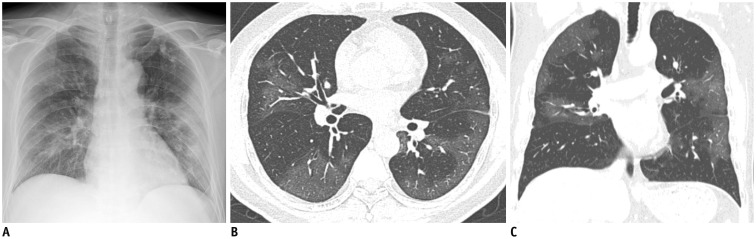 | Fig. 2Representative chest radiographic (A) and CT images (B, C) of COVID-19 pneumonia manifesting as confluent pure ground-glass opacities on CT.
A. Baseline anteroposterior chest radiograph shows patchy ground-glass opacities in right upper and lower lung zones and patchy consolidation in left middle to lower lung zones. Several calcified granulomas are incidentally noted in left upper lung zone. B, C. Baseline axial and coronal chest CT images show confluent pure ground-glass opacities involving both lungs. Most of confluent and patchy ground-glass opacities about pleura and fissure in peripheral lung. A few calcified granulomas are incidentally noted in left upper lobe.
|
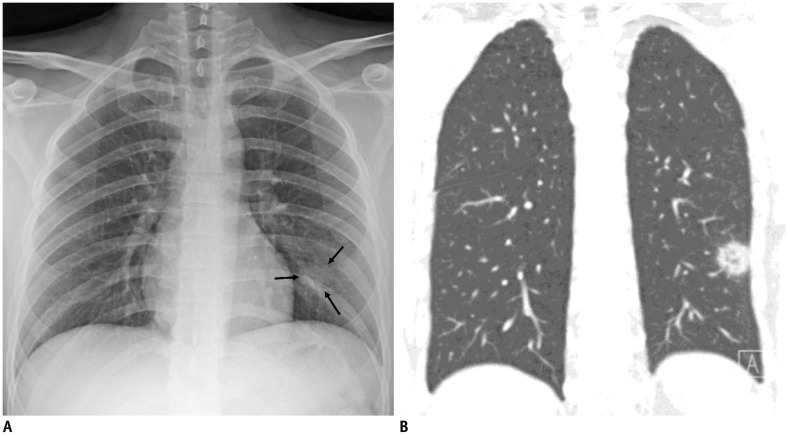 | Fig. 3Representative chest radiographic (A) and CT images (B) of COVID-19 pneumonia manifesting as single nodular lesion.
A. Anteroposterior chest radiograph shows single nodular consolidation (arrows) in left lower lung zone. B. Coronal chest CT image taken on same day shows 2.3-cm ill-defined nodular lesion with reversed halo sign with thick rim in left lower lobe, abutting adjacent pleura.
|
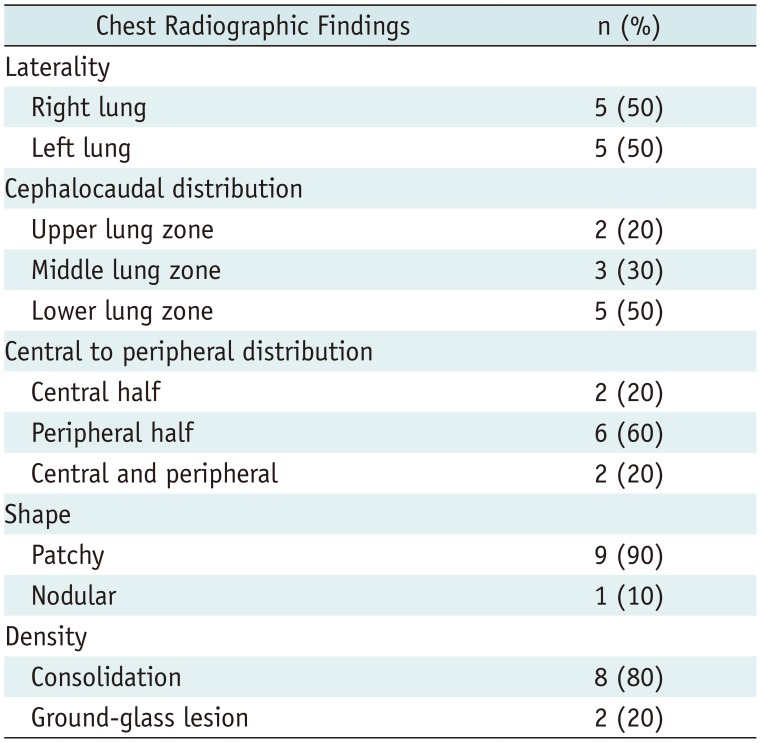
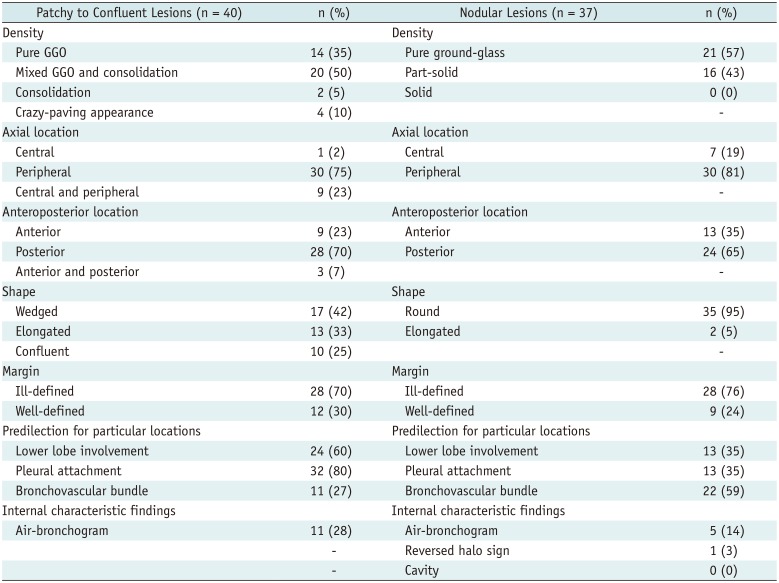
Table 1
Per-Lesion Analysis of Chest Radiographic Findings
Chest CT Findings
Table 2
Per-Lesion Analysis of Chest Computed Tomography Findings
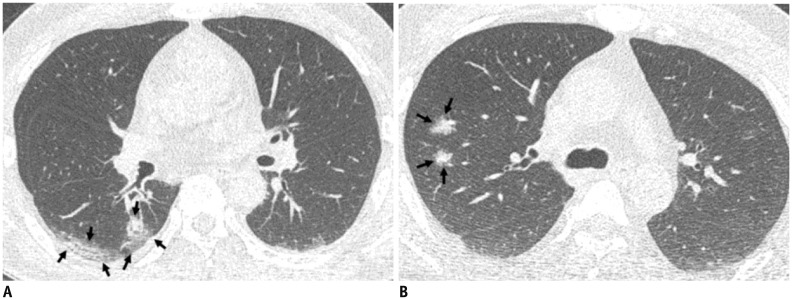 | Fig. 4Representative CT images (A, B) of COVID-19 pneumonia manifesting as radiograph-negative multiple patchy to nodular mixed ground-glass opacities and consolidations.
A. Axial chest CT image shows ill-defined mixed ground-glass opacities and consolidative lesions with patchy and elongated shape (arrows) touching pleura in superior segment of right lower lobe. B. Axial chest CT image shows ill-defined part-solid nodules (arrows; mixed ground-glass opacities and solid nodules) along bronchovascular bundles in posterior segment of right upper lobe.
|




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download