This article has been
cited by other articles in ScienceCentral.
Abstract
From December 2019, Coronavirus disease 2019 (COVID-19) pneumonia (formerly known as the 2019 novel Coronavirus [2019-nCoV]) broke out in Wuhan, China. In this study, we present serial CT findings in a 40-year-old female patient with COVID-19 pneumonia who presented with the symptoms of fever, chest tightness, and fatigue. She was diagnosed with COVID-19 infection confirmed by real-time reverse-transcriptase-polymerase chain reaction. CT showed rapidly progressing peripheral consolidations and ground-glass opacities in both lungs. After treatment, the lesions were shown to be almost absorbed leaving the fibrous lesions.
Go to :

Keywords: COVID-19, 2019-nCoV, Coronavirus, Pneumonia, Tomography, X-ray computed
INTRODUCTION
Since December 2019, cases of pneumonia with unknown causes have emerged in succession in Wuhan, China (
12). On January 7, 2020, it was identified as a type of novel coronavirus (Coronavirus disease 2019, COVID-19) by virus typing. By January 30, 2020, a total of 7700 cases were confirmed and 170 cases died (
3). To date, there have been few reports of chest Computed tomography (CT) findings of COVID-19 pneumonia patients (
4). We report a confirmed case of COVID-19 pneumonia in a 40-year-old female. Written informed consent was waived by the Jiangxi Provincial People's Hospital Institutional Review Board.
Go to :

CASE REPORT
A 40-year-old female presented with a fever for 3-days, as well as chest tightness, and fatigue for 2-days was admitted to our emergency department. The patient was physically healthy before and had no underlying diseases. She did not travel to Wuhan city and denied any contact with patients with COVID-19 infection.
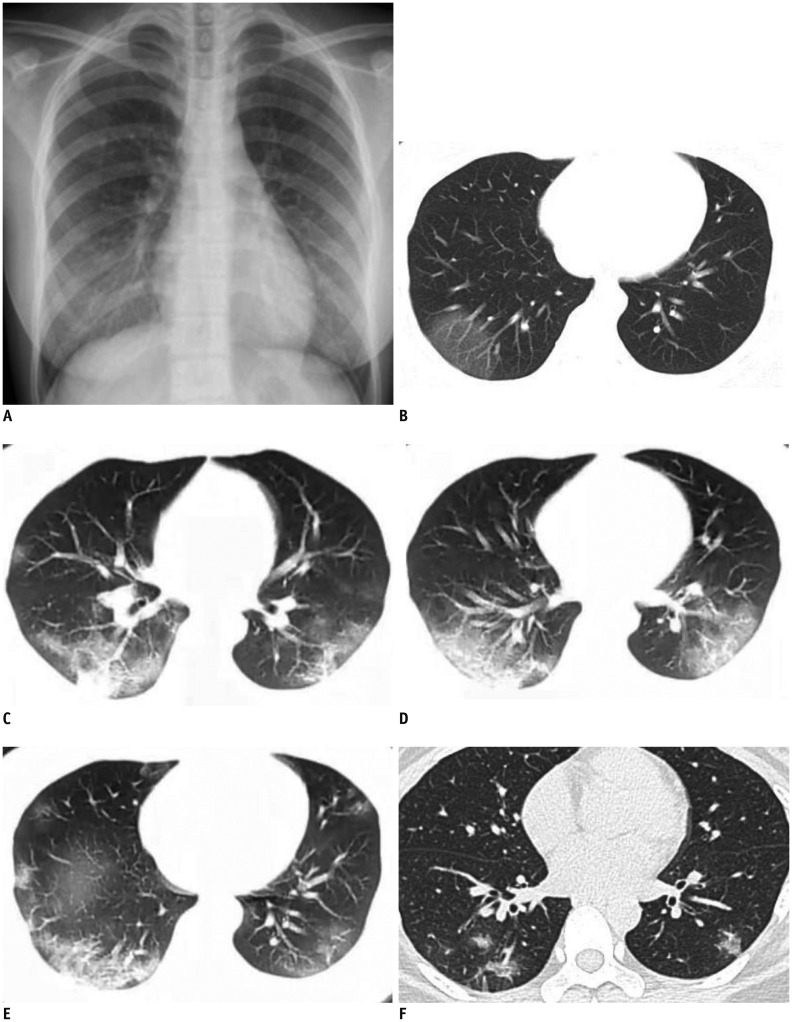
At admission, her body temperature was elevated to 38.9℃. Laboratory examinations showed normal leukocyte (4170/µL), neutrophils (59.6%), and lymphocytes (30.9%). There was an increase in hematocrit (0.456) and glucose (7.3 mmol/L) levels. The initial chest radiograph, taken 3-days after fever onset, was normal in both lungs (
Fig. 1A). On the same day, unenhanced chest CT showed ground-glass opacities (GGOs) in the subpleural area of the right lower lobe (
Fig. 1B), and the left lung was normal. She was given antibiotics for symptomatic treatment.
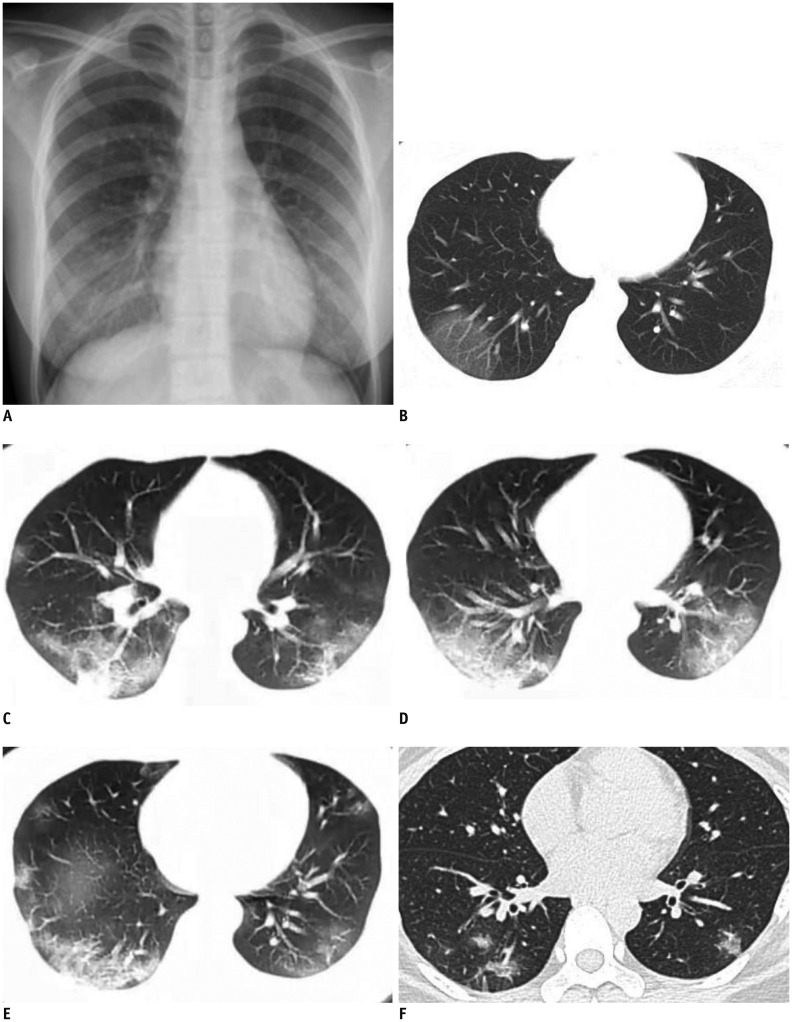 | Fig. 1
40-year-old female patient with Coronavirus disease 2019 pneumonia.
A, B. Initial posteroanterior chest radiograph and chest CT scan were performed on day of admission (3 days after onset of fever). Chest radiograph (A) shows no thoracic abnormalities. Axial CT scan (B) shows GGOs in subpleural area of right lower lobe. Left lung is normal. C–E. Follow-up chest CT scans taken 6 days after onset of fever show increased density of GGOs in right lower lobe, which then progressed into consolidations with perilobular thickening. Multifocal peripheral patchy areas of nodular consolidations and nodular GGO lesions are newly developed in subpleural areas of both lower lobes. F. Progressive resolution of parenchymal lesions is seen in follow-up high-resolution CT scan obtained on day 12. Patchy consolidations and GGOs in both lungs were almost absorbed leaving a few fibrous lesions that may represent residual organizing pneumonia. Repeat real-time reverse-transcriptase-polymerase chain reaction was negative and patient was discharged.
CT = computer tomography, GGO = ground-glass opacity

|
At first, the patient did not show any respiratory symptoms, however, on day 6 after fever onset, she began coughing. A follow-up chest CT revealed an increased density of GGOs in the right lower lobe, which then progressed into consolidations with perilobular thickening. Moreover, multifocal peripheral patchy areas of nodular consolidations and GGO lesions were newly developed in the subpleural areas of the both lower lobes (
Fig. 1C–E). Laboratory examination showed decreased leukocyte (3390/µL) and eosinophils (0.0%); normal neutrophils (67.4%) and lymphocytes (23.7%); and increased C-reactive protein (8.00 mg/L). The influenza A antigen screening was negative. Finally, she was diagnosed with COVID-19 infection by real-time reverse-transcriptase-polymerase chain reaction (rRT-PCR) amplification of the viral DNA from a sputum sample.
The patient was isolated and treated with antiviral drug (lopinavir: 200 mg/capsule, 2 capsules each time, twice a day) and antibiotics (tabaxin [piperacillin + tazobactam]). After 6 days of treatment, the temperature of the patient dropped to normal and the symptoms disappeared. On day 12, a repeat rRT-PCR was negative and the patient was discharged. At the time of discharge, a repeat CT showed that the previous consolidations and GGOs in both lungs were almost absorbed leaving a few fibrous lesions that may represent residual organizing pneumonia (
Fig. 1F).
Go to :

DISCUSSION
Since December 2019, some hospitals in Wuhan have been suffering from pneumonia of unknown causes, later identified as a COVID-19 by the whole genome sequence analysis of the viruses in the respiratory samples from the patients (
5). This coronavirus belongs to the β genus, which was named COVID-19 by World Health Organization (
67). Most of the initial cases had a history of exposure to the South China Seafood Market in Wuhan city, and some cases rendered a family clustering feature. The source of infection is still unknown, however it is speculated that the infection may have been caused by bats or vipers (
8). The infection is mainly transmitted through respiratory droplets. The median time from onset to admission to the hospital was 9 days, and most patients were between 40 and 60 years-old. The clinical manifestations are mainly fever, fatigue, and dry cough, with gradual dyspnea in some cases and acute respiratory distress syndrome in severe cases (
239). In this case, the patient had no clear history of contact with the epidemic area, and both the leukocytes and lymphocytes were normal, thus it was misdiagnosed as common pneumonia at first.
In this case, the initial CT showed GGOs in the right lower lobe, the pathology of which may represent pulmonary edema or hyaline membrane formation (
4). The density of the lesions is so subtle that it can hardly be depicted by conventional radiographs. Therefore, routine CT examination is recommended for the patients suspected of COVID-19 to reduce missed diagnosis (
1). CT findings of this patient include the short-term progression of lesions, multiple patchy consolidations and GGOs in both lungs, especially in the peripheral lung zones of the lower lobes, which may represent alveolar injury, cellular and fibrous exudation. After treatment, the consolidations and GGOs were almost absorbed, leaving fibrous cord-like shadows that represent fibrosis.
In conclusion, we report the serial CT findings in a female patient with COVID-19. Chest CT showed rapidly developing multiple patchy consolidations and GGOs in both lungs, which were mainly distributed in the peripheral areas. In the later stage, there may be a possibility of development of fibrosis. And with high-resolution CT, it will be easier to find GGOs in the early stage. The imaging findings of COVID-19 overlap with other viral pneumonia, therefore, nucleic acid tests are recommended for prompt diagnosis and treatment.
Go to :





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download