Abstract
Umbilical artery thrombosis is rare event and few prenatally diagnosed cases have been reported. Antenatal diagnosis is very critical, as it is associated with high risk of perinatal motility and morbidity such as intrauterine growth restriction and intrauterine fetal death. This study presents a rare case of intrauterine umbilical artery thrombosis, diagnosed by ultrasonography, at 32 weeks and 5 days of gestation in a 34-year-old woman who had an uneventful pregnancy. Early diagnosis with color Doppler ultrasonography is critical for pregnancy outcomes when fetal movement has diminished or intrauterine growth restriction is diagnosed, even though two umbilical artery already been confirmed on the first or the second-trimester ultrasonography scans.
Umbilical artery thrombosis is a rare condition associated with high risk of perinatal motility and morbidity such as intrauterine growth restriction and intrauterine fetal death.12 Shilling et al.1 retrieved seven cases from 116,000 births (0.006%) over a 13-year period and Sato and Benirschke2 obtained 11 cases from about 40,000 (0.025%) placenta pathology over a 30-year period. The affected infants were stillborn or had intrauterine growth restriction and live-born infants had a complicated neonatal course. The diagnosis for umbilical artery thrombosis is very critical for fetal outcomes because this pathologic result usually develops during third-trimester of gestation. If an earlier diagnosis is made before intrauterine fetal death and uncompromised fetal condition is noticed, the neonate can be rescued even if preterm baby was delivered. Herein, we present our experience of umbilical artery thrombosis during third-trimester of gestation with the relatedliteratures.
A 34-year-old woman, gravida 2, para 1, was taking antenatal care at our institution from the first-trimester of gestation. No abnormalities were found on the first and the second-trimester ultrasonography scans. The estimated fetal weight was concordant with gestational age. Three umbilical vessels were confirmed during the second ultrasonography scan.
At 32 weeks and 5 days of gestation, the patient complained she felt diminish of the fetal movement. The estimated fetal weight was at the 7th percentile with an estimated weight of 1,701 g. There was single paravesical color Doppler flow in the left umbilical artery that led to the diagnosis of a left single umbilical artery (Fig. 1A). The free umbilical cord of amniotic fluid showed one artery and highly twisted cord on the ultrasonography. The umbilical cord index was 0.476 coils/cm according to the 90th percentile.3 Doppler flow showed the resistance index (RI) in the umbilical artery was 0.48 (<5th percentile) and an increased diastolic flow in the middle cerebral artery (RI=0.64). Fetal heart rate monitoring showed “saw-tooth pattern” with bradycardia (Fig. 1B). Emergency cesarean section was performed. The newborn was male with a birth weight of 1,790 g. Apgar score was 4 at 1 minute and 6 at 5 minute. The pH of arterial umbilical cord gas was 7.167. The neonate was referred to the neonate intensive care unit and was discharged 4 weeks later.
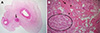
The placenta weighed 526 g and measured 18×14×4 cm according to the 50th percentile.4 The umbilical cord was inserted centrically and highly twisted with a diameter of 1.2 cm. Histologic examination confirmed the diagnosis of umbilical artery thrombosis. Three vessels were noted with thrombotic occlusion of one of umbilical arteries (Fig. 2A). The placenta microscopically presented necrotic and avasular villi embedded in large fibrinoid, and the collapsed intervillous space which consistent with early ischemic change (Fig. 2B).
The antenatal diagnosis of umbilical artery thrombosis is not usually difficult when using paravesical color Doppler flow, once the umbilical two arteries has been confirmed on the first or the second-trimester ultrasonography scans. However, it is not easy to distinguish it with congenital single umbilical artery without confirming normal umbilical two arteries. Therefore, in this study, it is called ‘pseudo-single umbilical artery’. Klaritsch et al.5 and Tanaka et al.6 suggested that closer sonographic evaluation of a cross section of the umbilical cord shows one artery with a small echogenic area between umbilical vein and artery which is suspected to be an occluded thrombotic umbilical arteryfor discrimination umbilical artery thrombosis from congenital single umbilical artery. Once umbilical artery thrombosis is suspected, the fetal should be carefully observed and emergency delivery will be need for rescuing the fetus from intrauterine death. Among the previously reported cases of umbilical artery thrombosis, only a few cases were diagnosed antenatally.789 Fortunately, the patient in this case visited the hospital because she felt diminish the fetal movement, and umbilical artery thrombosis was diagnosed on paravesical color Doppler ultrasonography. Emergency cesarean section was carried out as soon as abnormal heart beat pattern was discovered on the fetal heart rate monitoring. The abnormal fetal heart pattern that demonstrated marked increased variability of highly atypical nature, “saw-tooth pattern”, with bradycardia. This pattern might be associated with significant hypoxia or acidosis.10
In this case, hyper-coiled umbilical cord may have been the cause of umbilical artery thrombosis. Elongated and hypercoiled umbilical cord might have led to a reduction of blood flow5 leading to thrombosis of umbilical artery. The thrombus of umbilical artery migrates towards the placenta and cause hypoxia within the dependent placental vessels. Hypoxic conditions lead to ischemic necrosis of chorionic villi hindering the normal fetal growth. In the study of Shilling et al,1 all placentas showed evidence of hypo-perfusion such as avascular villi that are strongly associated with abnormal antenatal findings such intrauterine growth restriction acute and chronic monitoring abnormalities, oligohydramnios and stillbirth.1112 In order to prevent poor fetal outcomes of umbilical artery thrombosis, only early diagnosis and early delivery by careful maternal and fetal monitoring might have the favorable course.
Figures and Tables
Fig. 1
(A) There was single paravesical color Doppler flow in the left umbilical artery (arrow). (B)Fetal heart rate monitoring showed “saw-tooth pattern” with bradycardia.

Fig. 2
(A) Three vessels were noted with thromboic occlusion of one of umbilical arteries (arrow; H&E, ×12). (B) The placenta microscopically presented necrotic and avasular villi (arrowheads) embedded in large fibrinoid (arrow), and the collapsed intervillous space (circle) which consistent with early ischemic change (H&E, ×40).
References
1. Shilling C, Walsh C, Downey P, Mooney E. Umbilical artery thrombosis is a rare but clinically important finding: a series of 7 cases with clinical outcomes. Pediatr Dev Pathol. 2014; 17:89–93.

2. Sato Y, Benirschke K. Umbilical arterial thrombosis with vascular wall necrosis: clinicopathologic findings of 11 cases. Placenta. 2006; 27:715–718.

3. Mittal A, Nanda S, Sen J. Antenatal umbilical coiling index as a predictor of perinatal outcome. Arch Gynecol Obstet. 2015; 291:763–768.

4. Thompson JM, Irgens LM, Skjaerven R, Rasmussen S. Placenta weight percentile curves for singleton deliveries. BJOG. 2007; 114:715–720.

5. Klaritsch P, Haeusler M, Karpf E, Schlembach D, Lang U. Spontaneous intrauterine umbilical artery thrombosis leading to severe fetal growth restriction. Placenta. 2008; 29:374–377.

6. Tanaka K, Tanigaki S, Matsushima M, Miyazaki N, Hashimoto R, Izawa T, et al. Prenatal diagnosis of umbilical artery thrombosis. Fetal Diagn Ther. 2014; 35:148–150.

7. Cook V, Weeks J, Brown J, Bendon R. Umbilical artery occlusion and fetoplacental thromboembolism. Obstet Gynecol. 1995; 85(5 Pt 2):870–872.

8. Lutfallah F, Oufkir N, Markou GA, Frimigacci D, Poncelet C. A case of umbilical artery thrombosis in the third trimester of pregnancy. Am J Case Rep. 2018; 19:72–75.

9. Oliveira GH, Dias Cde M, Vaz-Oliani DC, Oliani AH. Intrauterine thrombosis of umbilical artery - case report. Sao Paulo Med J. 2016; 134:355–358.

10. FreemanRF , Garite TG, NageotteMP , Miller LA. Fetal heart rate monitoring. 4th ed. Philadelphia: Lippincott Williams & Wilkins;2012. p. 149–151.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download