Abstract
Purpose
To compare non-cycloplegic and cycloplegic refractive errors and evaluate the utility of cycloplegia in Korean children and young adolescents.
Methods
An anterospective study including 406 outpatients was conducted from September 2015 to December 2017. Pre and post-cycloplegic refractive errors for both eyes were measured using Ocucyclo® and Mydrin P® with an auto-refractor. Patients were divided into different groups according to age: group 1 (< 4 years), group 2 (4–6 years), group 3 (6–8 years), group 4 (8–10 years) and group 5 (< 20 years).
Results
A total of 203 patients were studied. Standard deviation (sphere post-pre) was 1.26 ± 1.02 diopters significant in all age groups (p < 0.05). The mean difference decreased with increasing age (r = 0.207, p < 0.05), however, 9% of group with age greater than 10 years old still had manifest refraction-cycloplegic refraction (MR-CR) difference greater than 2 diopters. There were no significant cylindrical or axial component value difference before and after cycloplegia (p = 0.071). Significantly greater MR-CR differences were observed in hypermetropes ≥ 6 years old and myopes ≤8 years old (p < 0.05). The prevalence of pre-cycloplegic eyes with anisometria was 22.6% and 32.6%, a total of 7.39% regressed after cycloplegia (p > 0.05).
Conclusions
After CR hyperopic shift was observed in all age groups. In patients with age greater than 10 years old, although statistically not significant, anisometropia and pseudomyopia still existed. Thus cycloplegic refraction should be performed in young adolescent to precisely measure and correct refractive error and avoid overcorrection.
Figures and Tables
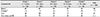
Table 2
Changes in the values of the spherical and cylindrical components before and after cycloplegia (both eyes)

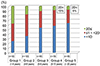
Table 3
Proportions of spherical, cylindrical, and axial differences before and after cycloplegia (both eyes)
References
1. Moses RA. Adler's physiology of the eye. 7th ed. St. Louis: CV Mosby;1981. p. 333–335.
2. Radhakrishnan H, Charman WN. Age-related changes in static accommodation and accommodative miosis. Ophthalmic Physiol Opt. 2007; 27:342–352.

3. Duane A. Studies in monocular and binocular accommodation, with their clinical application. Trans Am Ophthalmol Soc. 1922; 20:132–157.
4. Kim CK, Hong SH. Changes in refractive finding after using cycloplegics in young adult. J Korean Ophthalmol Soc. 1984; 25:341–345.
5. Krantz EM, Cruickshanks KJ, Klein BE, et al. Measuring refraction in adults in epidemiological studies. Arch Ophthalmol. 2010; 128:88–92.

6. Fotedar R, Rochtchina E, Morgan I, et al. Necessity of cycloplegia for assessing refractive error in 12-year-old children: a population-based study. Am J Ophthalmol. 2007; 144:307–309.

7. Chen J, Xie A, Hou L, et al. Cycloplegic and noncycloplegic refractions of Chinese neonatal infants. Invest Ophthalmol Vis Sci. 2011; 52:2456–2461.

8. Bannon RE. The use of cycloplegics in refraction. Am J Optom Arch Am Acad Optom. 1947; 24:513–568.

9. Maoury SD. Comparison of fixation targets during noncycloplegic retinoscopy. Am J Ophthalmol. 1967; 63:865.

10. Hiatt RL, Braswell R, Smith L, Patty JW. Refraction using mydriatic, cycloplegic, and manifest techniques. Am J Ophthalmol. 1973; 76:739–744.

11. Gwiazda J, Marsh-Tootle WL, Hyman L, et al. Baseline refractive and ocular component measures of children enrolled in the correction of myopia evaluation trial (COMET). Invest Ophthalmol Vis Sci. 2002; 43:314–321.
12. Fotouhi A, Morgan IG, Iribarren R, et al. Validity of noncycloplegic refraction in the assessment of refractive errors: the Tehran Eye Study. Acta Ophthalmol. 2012; 90:380–386.

13. Jorge J, Queiros A, González-Méijome J, et al. The influence of cycloplegia in objective refraction. Ophthalmic Physiol Opt. 2005; 25:340–345.

14. Kleinstein RN, Jones LA, Hullett S, et al. Refractive error and ethnicity in children. Arch Ophthalmol. 2003; 121:1141–1147.

15. Huynh S, Kifley A, Rose K, et al. Astigmatism and its components in 6-year-old children. Invest Ophthalmol Vis Sci. 2006; 47:55–64.

16. Huynh S, Kifley A, Rose K, et al. Astigmatism in 12-year-old Australian children: comparisons with a 6-year-old population. Invest Ophthalmol Vis Sci. 2007; 48:73–82.

17. Castagno V, Fassa A, Carret M, et al. Hyperopia: a meta-analysis of prevalence and a review of associated factors among school-aged children. BMC Ophthalmol. 2014; 14:163.

18. Guha S, Shah S, Shah K, et al. A comparison of cycloplegic autorefraction and retinoscopy in Indian children. Clin Exp Optom. 2017; 100:73–78.

19. Dobson V, Harvey E, Miller J, Clifford-Donaldson CE. Anisometropia prevalence in a highly astigmatic school-aged population. Optom Vis Sci. 2008; 85:512–519.

20. Kim R, Lee SY. The ratio of accommodative-convergence to accommodation in patients with nonrefractive accommodative esotropia. J Korean Ophthalmol Soc. 2014; 55:267–270.

21. Hofmeister EM, Kaupp SE, Schallhorn SC. Comparison of tropicamide and cyclopentolate for cycloplegic refractions in myopic adult refractive surgery patients. J Cataract Refract Surg. 2005; 31:694–700.

22. Yang SW, Lee NY, Kim SY. The effect of cycloplegia on vision and stereopsis: comparison between before and after cycloplegia. J Korean Ophthalmol Soc. 2006; 47:1454–1458.
23. Anderson HA, Hentz G, Glasser A, et al. Minus-lens-stimulated accommodative amplitude decreases sigmoidally with age: a study of objectively measured accommodative amplitudes from age 3. Invest Ophthalmol Vis Sci. 2008; 49:2919–2926.

24. Shufelt C, Fraser-Bell S, Ying-Lai M, et al. Refractive error, ocular biometry, and lens opalescence in an adult population: the Los Angeles Latino Eye Study. Invest Ophthalmol Vis Sci. 2005; 46:4450–4460.

25. Gwiazda J, Deng L, Manny R, et al. Seasonal variations in the progression of myopia in children enrolled in the correction of myopia evaluation trial. Invest Ophthalmol Vis Sci. 2014; 55:752–758.

26. Morgan IG, Iribarren R, Fotouhi A, Grzybowski A. Cycloplegic refraction is the gold standard for epidemiological studies. Acta Ophthalmol. 2015; 93:581–585.

27. Choong YF, Chen AH, Goh PP. A comparison of autorefraction and subjective refraction with and without cycloplegia in primary school children. Am J Ophthalmol. 2006; 142:68–74.

28. Zhao J, Mao J, Luo R, et al. Accuracy of noncycloplegic autorefraction in school-age children in China. Optom Vis Sci. 2004; 81:49–55.

29. Liang CL, Hung KS, Park N, et al. Comparison of measurements of refractive errors between the hand-held Retinomax and on-table autorefractors in cyclopleged and noncyclopleged children. Am J Ophthalmol. 2003; 136:1120–1128.

30. Twelker JD, Mutti DO. Retinoscopy in infants using a near non-cycloplegic technique, cycloplegia with tropicamide 1%, and cycloplegia with cyclopentolate 1%. Optom Vis Sci. 2001; 78:215–222.

31. Sanfilippo PG, Chu BS, Bigault O, et al. What is the appropriate age cut-off for cycloplegia in refraction? Acta Ophthalmol. 2014; 92:e458–e462.





 PDF
PDF ePub
ePub Citation
Citation Print
Print







 XML Download
XML Download