Abstract
Purpose
Methods
Results
Conclusions
Figures and Tables
 | Figure 1Peak and trough intraocular pressure (IOP) of cytomegalovirus (CMV)-positive and CMV-negative hypertensive uveitis. In the CMV polymerase chain reaction (PCR) positive patients, the peak IOP during the duration of the disease was found to be lower than that of the negative patients, but no statistically significant difference was observed (p = 0.199). However, the trough IOP during the duration of the disease was statistically significantly higher in the CMV PCR-positive patients than in the negative patients (p = 0.007). *Student's t-test; †Mann-Whitney's U-test. |
 | Figure 2Baseline and intereye differences of corneal endothelial cell density of cytomegalovirus (CMV)-positive and CMV-negative hypertensive uveitis patients. A lower corneal endothelial cell density was found in the CMV polymerase chain reaction positive patients, but no statistically significant difference was noted (p = 0.244, student's t-test). However, we also examined the corneal endothelial cell density in the opposite eye to determine the difference in binocularity, and the results showed a significant difference between CMV-positive and negative groups (p = 0.048, Mann-Whitney's U-test). ECD = endothelial cell count. |
 | Figure 3Different corneal manifestations of cytomegalovirus (CMV) positive hypertensive anterior uveitis patients. A 25-year-old female patient with CMV-positive anterior uveitis showed a coin-like lesion (A) and a 55-year-old male patient showed ring-like opacity (B). In addition, a 27-year-old male patient showed a simple keratic precipitate (C) and a 72-year-old male patient showed multiple keratitic precipitate with iris pigmentation (D). |
 | Figure 4Iris changes associated with cytomegalovirus positive hypertensive anterior uveitis. When compared to the normal opposite eye (A), the iris atrophy was observed within the affected left eye (B) of a 25-year-old female patient. A 60-year-old male patient showed a spongy-like change of inferior iris stroma of the affected eye (D), compared to the normal opposite eye (C). |
 | Figure 5Serial changes of a 55-year-old male patient. At baseline examination, superior ring-like opacity of the cornea was shown (A) and after 2 months, aggravation of ring like opacity was observed (B). Round stromal opacity at the center of the ring-like opacity appeared 5 months later (C). After 7 months, ring like opacity was improved (D). |
Table 1
Characteristics of CMV positive and CMV negative hypertensive uveitis
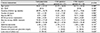
The medical records and the ophthalmic test results were able to compare the overall characteristics between patient groups with CMV positive and CMV negative hypertensive uveitis. Values are presented as mean ± standard deviation or number (%).
CMV = cytomegalovirus; M:F = male:female; BCVA = best-corrected visual acuity; RNFL = retinal nerve fiber layer; CCT = central corneal thickness.
*Student's t-test; †chi-square test; ‡Mann-Whitney's U-test.
Table 2
Patients list of CMV positive hypertensive anterior uveitis

Clinical features and progress of the enrolled CMV positive hypertensive anterior uveitis patients were summarized.
CMV = cytomegalovirus; BCVA = best-corrected visual acuity; F/U = follow-up; IOP = intraocular pressure; PCR = polymerase chain reaction; ECD = endothelial cell count; M = male; PO = per os (orally); DM = diabetes mellitus; TB = tuberculosis; F = female; KP = keratic precipitate; HTN = hytertension.
Table 3
Immunologic status of CMV positive and CMV negative hypertensive uveitis

There was no statistically significant difference in serologic tests between patient groups with CMV positive and CMV negative hypertensive uveitis. Values are presented as mean ± standard deviation number (%).
CMV = cytomegalovirus; WBC = white blood cell; ESR = erythrocyte sedimentation rate; CRP = C-reactive protein; RA = rheumatoid factor; IgM = immunoglobulin M; IgG = immunoglobulin G; Ab = antibody.
*Student's t-test; †Mann-Whitney's U-test.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download